Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (31): 5066-5071.doi: 10.3969/j.issn.2095-4344.2017.31.025
Previous Articles Next Articles
Association of lumbar facet tropism and orientation with lumbar disc herniation
Zhou Qiang, Teng Dong-hui, Jiang Wen-xue
- Department of Orthopedics, Tianjin First Central Hospital, Tianjin 300192, China
-
Online:2017-11-08Published:2017-12-01 -
Contact:Jiang Wen-xue, Master’s supervisor, Chief physician, Department of Orthopedics, Tianjin First Central Hospital, Tianjin 300192, China -
About author:Zhou Qiang, M.D., Department of Orthopedics, Tianjin First Central Hospital, Tianjin 300192, China
CLC Number:
Cite this article
Zhou Qiang, Teng Dong-hui, Jiang Wen-xue. Association of lumbar facet tropism and orientation with lumbar disc herniation[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(31): 5066-5071.
share this article
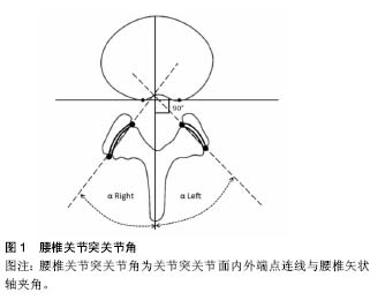
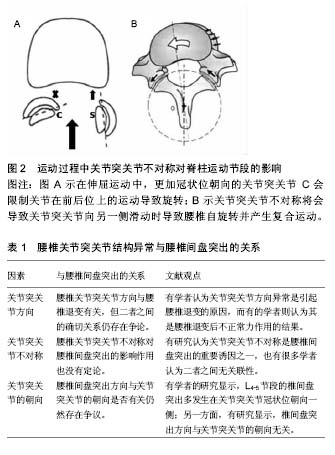
2.1 腰椎关节突关节基本功能 腰椎关节突关节是腰椎三关节复合体的重要组成部分,具有重要的功能。关节突关节可传导剪切力并协助椎间盘承载轴向负荷,Adams等[1-2]的研究发现,当直立位时关节突关节承载的轴向负荷为16%,而坐位时关节突关节承载的轴向负荷明显下降,这也解释了坐位时椎间盘压力高的原因。腰椎关节突关节为腰椎提供后方机械支持,在腰椎屈伸过程中起到稳定作用,并可防止椎间盘过度扭转。腰椎关节突关节的形状和朝向决定了其阻止脊柱过度运动的作用。更加矢状位倾斜的上腰椎的关节突关节,可以承担更多的伸屈运动功能,并抵抗冠状位旋转;更加冠状位倾斜的下腰椎的关节突关节,可以承担更多的冠状位旋转功能,同时抵抗伸屈运动和剪切力[3-4]。当脊柱进行矢状位上的运动时,关节突关节的关节面会进行倾斜。Masharawi等[5]认为关节突关节不对称把单切面的运动变为多切面运动。例如,在脊柱的矢状位运动时,由于冠状位朝向的关节突关节会阻止关节前后平面方向的运动,从而导致沿着矢状位朝向关节突关节做旋转运动。单独扭转并不能对椎间盘的完整性构成破坏,但当扭转合并屈曲时,将会对椎间盘的完整性形成破坏[6]。屈曲、扭转复合运动在关节突关节不对称时将会导致髓核向后外侧移动,如在屈曲合并向左旋转时,髓核会对右后外侧的纤维环形成挤压[7]。应用有限元分析,Schmidt等[8]发现在同样的载荷下,屈曲合并向左旋转时右后外侧的纤维环内侧纤维将承载最大的剪切力。多个生物力学研究表明屈曲合并旋转会对后外侧纤维环形成损伤[9-10]。 2.2 关节突关节方向与腰椎间盘突出的关系 腰椎关节突关节方向与腰椎退变之间的确切关系还存在争议,见 表1。腰椎关节突关节角是指关节突关节面内外端点连线与腰椎矢状轴夹角(图1)。腰椎关节突关节角方向异常被认为是造成腰椎退变的原因之一[10-15],研究显示腰椎退变性滑脱和矢状位朝向关节突关节有关[16-22]。Linova等[23]的研究发现腰椎关节突关节退变和矢状位朝向的关节突关节有关。Leonid等[3]的研究显示随着年龄的增长关节突关节变的更加向矢状位倾斜,提示退变引起的应力变化导致关节突关节再塑形,从而出现方向的改变。腰椎关节突关节方向与腰椎退变有关,但二者之间的确切关系仍存在争论。有的学者认为关节突关节方向异常是引起腰椎退变的原因,而有的学者则认为其是腰椎退变后不正常力作用的结果。"
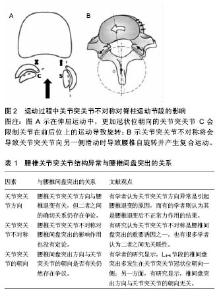
2.3 关节突关节不对称与腰椎间盘突出的关系 腰椎关节突关节不对称对腰椎间盘突出的影响作用也没有定论,见表1。Brailsford[24]首次对腰椎关节突关节不对称(tropism)进行了定义:腰椎关节突关节的左右不对称,其中一侧较另一侧更加向矢状位倾斜。文献报道腰椎关节突关节不对称在人群中发生的概率为10%-70.5%,腰椎关节突关节不对称最常发生L5-S1,其次为L4-L5[3,10]。关节突关节不对称可以改变腰椎活动时的生物力学构成,关节突角的不对称性可引起脊柱异常活动度的增加,使两侧关节突和椎间盘的承载不均匀,增加关节突退变和椎间盘损伤的机会,是可能导致相邻椎间盘退变的原因。 有大量关于腰椎关节突关节不对称与腰椎间盘突出关系的研究[10-13,25-30],有学者认为关节突关节不对称是腰椎间盘突出的重要诱因之一[11,25-26],也有很多学者认为二者之间无关联性[14,27-33]。Farfan等[25]提出日常活动中的扭转应力在腰椎间盘的早期退变和突出中起着重要作用,认为关节突关节不对称所造成的不稳与椎间盘的退变和突出有着密切的关系。他们还研究了纤维环破裂的方式和椎间盘的形态、位置与关节突大小、方向的关系、发现不对称的关节导致不对称的退变,对称的关节产生对称的退变。脊柱屈曲运动时,由于冠状位朝向关节突关节对椎体间剪切力的抵抗不足,导致冠状位朝向一侧的关节突会限制关节在前后平面内的运动,从而导致沿形态偏向矢状方向的一侧旋转。因此,不对称关节突关节可导致脊柱自动旋转运动(图2)[11]。运动节段的屈曲和扭转组合运动研究已经发现,不对称节段的运动将髓核转移后外侧,如屈曲加右轴向旋转过程中髓核被推向左后外侧环。不对称关节突关节会产生的不对称的轴向旋转,会对椎间盘施加额外的扭转负荷,进而导致椎间盘退变及突出。Cyron等[11]通过尸体生物力学实验观测到脊柱运动阶段承受载荷时,关节突关节不对称的运动节段其轴向旋转总是倾向于关节面斜的一侧,关节突关节的不对称增加了纤维环的扭转应力,因而关节突角不对称会增加椎间盘损伤和变性的概率。Noren等[26]的研究也得出类似的结论。但是,Boden等[27]的研究认为关节突关节不对称与椎间盘退变无关。Cassidy等[28]的研究发现关节突关节不对称与腰椎间盘突出发生无显著关联,腰椎关节突关节不对称并不能导致腰椎间盘突出。Adams等[1]认为关节突关节的形态与轴向旋转是无关的,无论关节突偏向矢状位或冠状位,均足以承受轴向旋转载荷,只有关节突关节破坏后才可能发生椎间盘损伤。腰椎间盘提出的位置与关节朝向无关。国内戴力扬等[33]报道141例L4/5及L5/S1椎间盘突出病例,发现这2个间隙椎间盘突出与关节突关节不对称的关系无显著相关性,该研究也不支持关节突关节不对称导致腰椎间盘突出的结论。 2.4 腰椎间盘突出方向与不对称关节突关节朝向的关系 腰椎间盘突出方向与关节突关节的朝向是否有关仍然存在争议,见表1。早在1967年,Farfan等[25]的研究发现椎间盘突出多发生在不对称关节突关节中的更加冠状位朝向一侧,他们的研究提示冠状位朝向的关节突关节承担较少的椎体间剪切力,因此当腰椎向更加冠状位朝向的关节突关节一侧旋转时纤维环将承受额外的扭转应力,容易导致该侧纤维环撕裂、髓核突出。Boden等[27]认为仅L4-5节段的椎间盘突出多发生在关节突关节冠状位朝向一侧。Loback等[34]的资料显示病变节段关节突关节不对称的发生率中央型椎间盘突出患者高于旁侧型椎间盘突出患者,椎间盘突出多发生在关节突关节冠状位朝向一侧[35]。张光铂等[36]的研究也显示关节突关节不对称与该节段的椎间盘变性有明显的相关性,腰椎关节突关节不对称节段椎间盘变性的发生率明显增加,且椎间盘突出多发生在更加冠状位朝向的关节突关节一侧。另一方面,Hagg[29]及Cassidy等[28]的研究显示,椎间盘突出方向与关节突关节的朝向无关,椎间盘突出即突向冠状位朝向一侧关节突关节和突向矢状位朝向一侧关节突关节并无统计学意义,二者之间并无关联性。"
| [1] Adams MA, Hutton WC. The effect of posture on the role of the apophysial joints in resisting intervertebral compressive forces. J Bone Joint Surg. 1980; 62: 358-362.?[2] Kalichmanand L, Hunter DJ. Lumbar facet joint osteoarthritis: a review. Semin Arthritis Rheum. 2007; 37: 69-80. ?[3] Leonid K, Pradeep S, Ali G, et al. Facet tropism and orientation: associations with facet joint osteoarthritis and degenerative spondylolisthesis. Spine. 2009; 34(16): E579-E585.[4] Cohen Steven P, Raja Srinivasa N. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007; 106:591-614.[5] Masharawi Y, Rothschild B, Salame K, et al. Facet tropism and interfacet shape in the thoracolumbar vertebrae: characterization and biomechanical interpretation. Spine. 2005;30:281-292.[6] Veres SP, Robertson PA, Broom ND. The influence of torsion on disc herniation when combined with flexion. Eur Spine J. 2010;19:1468-1478.[7] Fazey PJ, Song S, Monsas S, et al. An MRI investigation of intervertebral disc deformation in response to torsion. Clin Biomech. 2006;21:538-542.[8] Schmidt H, Kettler A, Heuer F, et al. Intradiscal pressure, shear strain, and fiber strain in the intervertebral disc under combined loading. Spine. 2007;32:748-755.[9] Drake JD, Aultman CD, McGill SM, et al. The influence of static axial torque in combined loading on intervertebral joint failure mechanics using a porcine model. Clin Biomech. 2005;20:1038-1045.[10] Karacan I, Aydin T, Sahin Z, et al. Facet angles in lumbar disc herniation: their relation to anthropometric features. Spine. 2004;29:1132-1136.[11] Cyron BM, Hutton WC. Articular tropism and stability of the lumbar spine. Spine. 1980;5:168-172.[12] Kunakornsawat S, Ngamlamaidt K, Tungsiripat R, et al. The relationship of facet tropism to lumbar disc herniation . J Med Assoc Thai. 2007;90(27):1337-1341.[13] Lee DY, Ahn Y, Lee SH. The influence of facet tropism on herniation of the lumbar disc in adolescents and adults . J Bone Jt Surg Br. 2006; 8:520-523.[14] Park JB, Chang H, Kim KW, et al. Facet tropism: a comparison between far lateral and posterolateral lumbar disc herniations. Spine, 2001; 26:677-679.[15] Adams MA, Hutton WC; The relevance of torsion to the mechanical derangement of the lumbar spine. Spine. 1981;6: 241-248.[16] Fitzgerald JA, Newman PH. Degenerative spondylolisthesis . J Bone Joint Surg Br. 1976; 58:184-192.[17] Grobler LJ, Robertson PA, Novotny JE, et al. Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology . Spine.1993;18:80-91. [18] Kim NH, Lee JW. The relationship between isthmic and degenerative spondylolisthesis and the configuration of the lamina and facet joints . Eur Spine J. 1995; 4:139-144.[19] Nagaosa Y, Kikuchi S, Hasue M, et al. Pathoanatomic mechanisms of degenerative spondylolisthesis. A radiographic study. Spine.1998; 23:1447-1451.[20] Sato K, Wakamatsu E, Yoshizumi A, et al. The configuration of the laminas and facet joints in degenerative spondylolisthesis. A clinicoradiologic study. Spine. 1989;14: 1265-1271.[21] Dai LY. Orientation and tropism of lumbar facet joints in degenerative spondylolisthesis. Int Orthop. 2001;25:40-42.[22] Fujiwara A, Tamai K, An HS, et al. Orientation and osteoarthritis of the lumbar facet joint. Clin Orthop Relat Res. 2001;385:88-94.[23] Linova L, Klindukhova A, Lib L, et al. Lumbar facet joint orientation and osteoarthritis: A cross-sectional study. J Back Musculoskelet Rehabil. 2013;26:421-426.[24] Brailsford JF. Deformities of the lumbosacral region of the spine . Br J Surg. 1928;16:562-627.[25] Farfan HF, Sullivan JD. The relation of facet orientation to intervertebral disc failure . Can J Surg. 1967;10:179-185.[26] Noren R, Trafimow J, Andersson GB, et al. he role of facet joint tropism and facet angle in disc degeneration . Spine. 1991;16:530-32.[27] Boden SD, Riew KD, Yamaguchi K, et al. Orientation of the lumbar facet joints: association with degenerative disc disease. J Bone Jt Surg Am. 1996;78: 403-411.[28] Cassidy JD, Loback D, Yong-Hing K, et al. Lumbar facet joint asymmetry. Intervertebral disc herniation. Spine. 1992;17: 570-574.[29] Hagg O, Wallner A. Facet joint asymmetry and protrusion of intervertebral disc. Spine. 1990;15:356-359.[30] Vanharanta H, Floyd T, Ohnmeiss D. The relationship of facet tropism to degenerative disc disease. Spine. 1993;18: 1000-1005.[31] Ishihara H, Matsui H, Osada R, et al. Facet joint asymmetry as a radiologic feature of lumbar intervertebral disc herniation in children and adolescents. Spine. 1997;22:2001-2004.[32] Ko HY, Park BK. Facet tropism in lumbar motion segments and its significance in disc herniation. Arch Phys Med Rehabil. 1997;78:1211-214.[33] 戴力扬,贾连顺.腰椎关节突关节不对称[J].中国脊柱脊髓杂志, 1996,6(3):106-108.[34] Loback D, Young-Hing K, Cassidy D, et al. The relationship between facet orientation and lumbar disc herniation: the role of torsion in intervertebral disc failure. Orthop Trans. 1985; 9:560-563.[35] Kénési C, Lesur E. Orientation of the articular processes at L4, L5, and S1. Possible role in pathology of the intervertebral disc. Anat Clin. 1985;7:43-47.[36] 张光铂,绳厚福,史振才. 腰椎关节突关节不对称与椎间盘变性[J].中国脊柱脊髓杂志,1997,7(5):199-201.[37] Manish C, Gaurav S, Shobha SA, et al. Association of facet tropism with lumbar disc herniation. Eur Spine J. 2013; 22(5): 1045-1052.[38] Wang JX, Yang XY. Age-Related Changes in the Orientation of Lumbar Facet Joints. Spine. 2009; 34: E596-E598.[39] 王大林,吴小涛,王黎明. 腰椎关节突关节不对称与青少年腰椎间盘突出症[J]. 中国脊柱脊髓杂志,2005,15(6):341-344.[40] Wang H, Zhou YJ. Facet tropism: possible role in the pathology of lumbar disc herniation in adolescents. Neurosurg Pediatr. 2016 ;18(1):111-115. [41] Wang H, Zhang Z, Zhou Y. Irregular Alteration of Facet Orientation in Lumbar Segments: Possible Role in Pathology of Lumbar Disc Herniation in Adolescents. World Neurosurg. 2016; 86:321-327.[42] Grogan J, Nowicki BH, Schmidt TA, et al. Lumbar facet joint tropism does not accelerate degeneration of the facet joints. AJNR Am J Neuroradiol. 1997;18(7):1325-1329. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [3] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [4] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [5] | Song Jiawei, Yang Yongdong, Yu Xing, Yang Jizhou, Wang Fengxian, Qu Yi, Bi Lianyong. Mid-term effect of Isobar EVO non-fusion dynamic fixation in the treatment of adjacent segment disease after lumbar fusion [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 908-913. |
| [6] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [7] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [8] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [9] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [10] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [11] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [12] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [13] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [14] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [15] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||