Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (36): 5886-5896.doi: 10.3969/j.issn.2095-4344.2915
Factors for the recurrence of lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: a meta-analysis
Qian Yuzhang1, Wang Nan1, Dong Yuqi1, Xie Lin2, Kang Ran2
- 1Third Clinical Medical College of Nanjing University of Chinese Medicine, Nanjing 210000, Jiangsu Province, China; 2Department of Orthopedics, Nanjing Integrated Traditional Chinese and Western Medicine Hospital, Nanjing University of Chinese Medicine, Nanjing 210000, Jiangsu Province, China
-
Received:2020-03-16Revised:2020-03-21Accepted:2020-04-18Online:2020-12-28Published:2020-10-27 -
Contact:Xie Lin, Chief physician, Doctoral supervisor, Department of Orthopedics, Nanjing Integrated Traditional Chinese and Western Medicine Hospital, Nanjing University of Chinese Medicine, Nanjing 210000, Jiangsu Province, China -
About author:Qian Yuzhang, Master candidate, Third Clinical Medical College of Nanjing University of Chinese Medicine, Nanjing 210000, Jiangsu Province, China -
Supported by:the Leading Talent Training of Chinese Medicine of Jiangsu Province, No. SLJ0210 (to XL); the Jiangsu Commission of Health Project No. H2018025
CLC Number:
Cite this article
Qian Yuzhang, Wang Nan, Dong Yuqi, Xie Lin, Kang Ran. Factors for the recurrence of lumbar disc herniation after percutaneous transforaminal endoscopic discectomy: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(36): 5886-5896.
share this article
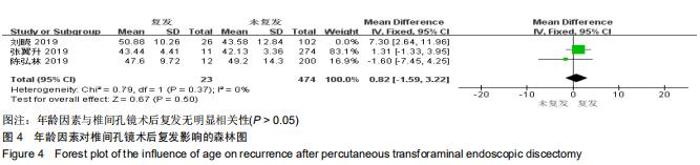
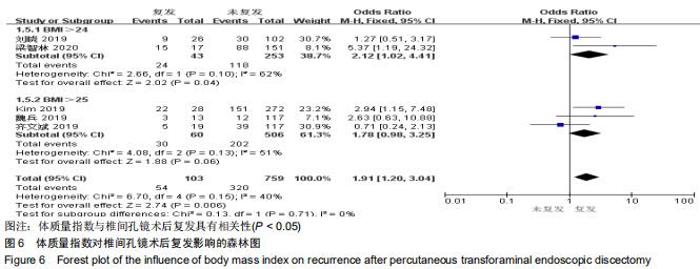
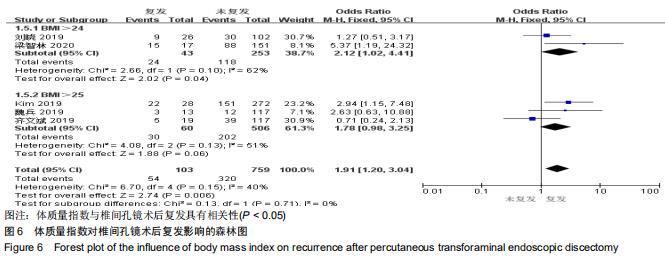
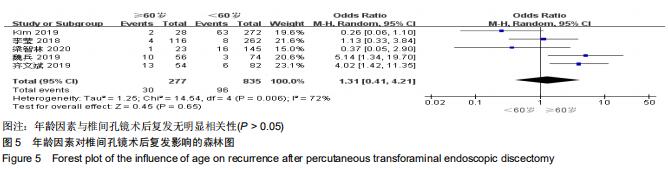
2.3.2 年龄因素对复发的影响 共8篇文献报告了年龄对椎间孔镜术后复发的影响[9-15,18],其中3篇文献比较了患者年龄的平均数及方差[12-13,15]。异质性检验分析显示:I2=70%,存在异质性,对纳入的文献进行敏感性分析,结果有1个研究对结果影响较大[12],遂予排除该项研究后,异质性检验分析显示:I2=0%,不存在异质性,故采用固定效应模型进行分析,Meta分析结果显示年龄对于椎间孔镜术后复发影响关系无显著性差异(MD=0.82,95%CI:-1.59-3.22,P=0.50),见图4。有5篇文献将患者年龄按分为≥60岁组 及<60岁组[9-11,14,18]。异质性检验分析显示:P=0.004,I2=72%,显示存在异质性,敏感性分析发现各文献对结果无明显影响,故采用随机效应模型进行分析,Meta分析结果显示,椎间孔镜术后患者复发与年龄差异无显著性 (OR=1.31,95%CI:0.41-4.21,P=0.65),见图5。 "
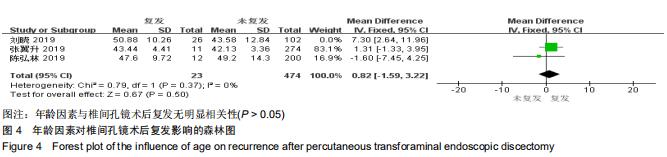
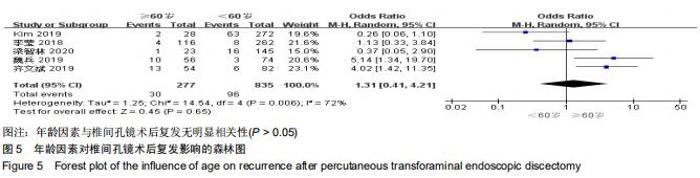
2.3.2 年龄因素对复发的影响 共8篇文献报告了年龄对椎间孔镜术后复发的影响[9-15,18],其中3篇文献比较了患者年龄的平均数及方差[12-13,15]。异质性检验分析显示:I2=70%,存在异质性,对纳入的文献进行敏感性分析,结果有1个研究对结果影响较大[12],遂予排除该项研究后,异质性检验分析显示:I2=0%,不存在异质性,故采用固定效应模型进行分析,Meta分析结果显示年龄对于椎间孔镜术后复发影响关系无显著性差异(MD=0.82,95%CI:-1.59-3.22,P=0.50),见图4。有5篇文献将患者年龄按分为≥60岁组 及<60岁组[9-11,14,18]。异质性检验分析显示:P=0.004,I2=72%,显示存在异质性,敏感性分析发现各文献对结果无明显影响,故采用随机效应模型进行分析,Meta分析结果显示,椎间孔镜术后患者复发与年龄差异无显著性 (OR=1.31,95%CI:0.41-4.21,P=0.65),见图5。 "
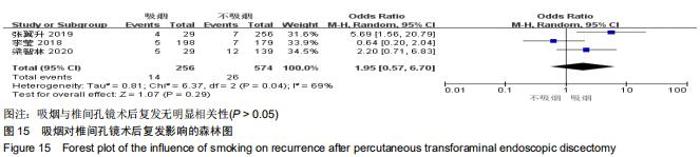
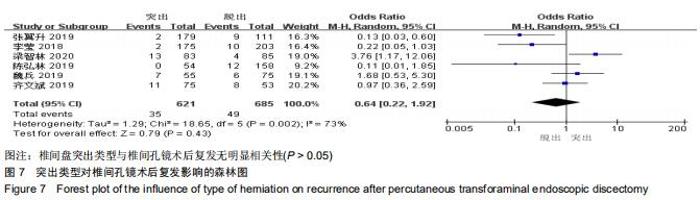
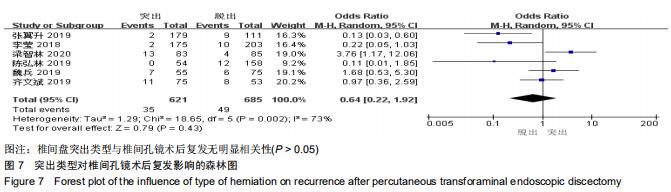
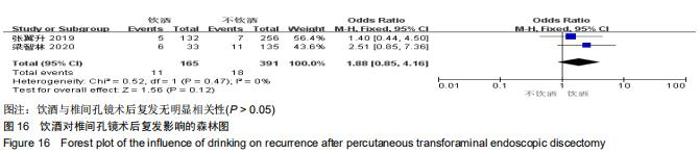
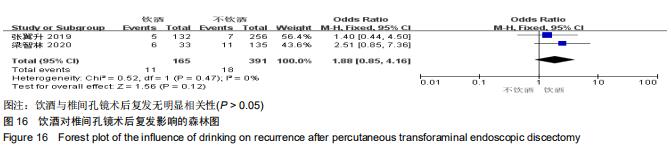
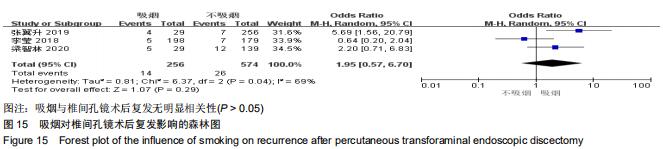
2.3.12 吸烟因素对复发的影响 有3篇文献报告了研究对象是否具有吸烟史[9,13,18],异质性检验分析显示I2=69%,有异质性,采用随机效应模型进行分析,Meta分析显示:OR=1.95,95%CI:0.57-6.70,P=0.29,结果显示患者是否具有吸烟史与其椎间孔镜术后复发无明显相关性,具体见图15。同时敏感性分析结果显示李莹等[18]对结果影响较大,当剔除该项研究时,其I2=16%,异质性较低,采用固定效应模型显示结果显示:OR=3.12,95%CI:1.33-7.32,P=0.009,提示吸烟与患者术后复发存在一定的相关性,与上述结果矛盾。因此吸烟对患者术后的复发可能存在一定的影响,但将来需要更多的研究来进一步明确其相关性。 "
|
[1] DEYO RA, MIRZA SK. Herniated lumbar intervertebral disk. N Engl J Med. 2016;374(18):1763-1772.
[2] BLAMOUTIER A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res. 2013;99(1 Suppl):S187-196.
[3] SNYDER LA, O'TOOLE J, EICHHOLZ KM, et al. The technological development of minimally invasive spine surgery. Biomed Res Int. 2014;(4):2014.
[4] MINAMIDE A, YOSHIDA M, YAMADA H, et al. Endoscope- assisted spinal decompression surgery for lumbar spinal stenosis. J Neurosurg Spine. 2013;19(6):644-671.
[5] HOOGLAND T, SCHUBERT M, MIKLITZ B, et al. Transforminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976). 2006;31(24):890-897.
[6] BAI J, ZHANG W, LIU X, et al. Percutaneous transforaminal endoscopic discectomy in the treatment of senior patients with lumbar degenerative disc disease. Exp Ther Med. 2018; 17(1):874-882.
[7] 冯帆,蔡毅,李颖波,等.腰椎间盘突出症7种手术修复方式差异的网络Meta分析[J].中国组织工程研究,2020,24(3):453-459.
[8] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603-605.
[9] 梁智林,海涌,杨晋才,等.经皮椎间孔镜治疗腰椎间盘突出症术后复发影响因素研究[J].中国骨与关节杂志,2020,9(1):5-10.
[10] KIM HS, YOU JD, JU C. Predictive Scoring and Risk Factors of Early Recurrence after Percutaneous Endoscopic Lumbar Discectomy. BioMed Research Int. 2019. doi: 10.1155/2019/6492675.
[11] 齐文斌,朱彦海.经皮椎间孔镜手术治疗腰椎间盘突出症的疗效观察及术后复发的相关因素分析[J].颈腰痛杂志,2019,40(6): 776-780.
[12] 刘晓.经皮椎间孔镜治疗腰椎间盘突出症术后复发的危险因素分析[D].南京:南京中医药大学,2019.
[13] 张翼升.经皮椎间孔镜治疗腰椎间盘突出症术后复发相关因素的研究[D].南宁:广西中医药大学,2019.
[14] 魏兵.腰椎间盘突出症患者椎间孔镜手术后复发的危险因素分析[J].实用骨科杂志,2019,25(2):101-104, 116.
[15] 陈弘林.腰椎间盘突出症内镜术后复发的影响因素分析[D].乌鲁木齐:新疆医科大学,2019.
[16] XU JT, LI YW, WANG B, et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation with modic changes via a transforaminal approach: a retrospective study. Pain physician. 2019;22(6):E601.
[17] 陈新宇,于崇龙,王嘉鹏,等.椎间孔镜治疗腰椎间盘突出症术后复发因素的探讨[J].临床医药文献电子杂志,2018,5(96):73-74.
[18] 李莹,唐谨,吴从俊,等.椎间孔镜下治疗腰椎间盘突出症术后复发相关因素及再次处理效果探讨[J].中国中医骨伤科杂志,2018, 26(11):37-41.
[19] KIM JM, LEE SH, AHN Y, et al. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg. 2007;50(2):82-85.
[20] VIALLE LR, VIALLE EN, SUÁREZ HENAO JE, et al. Lumbar disc herniation. Rev Bras Ortop. 2015;45(1):17-22.
[21] LIANG J, CHEN C, ZHAO H. Revision surgery after percutaneous endoscopic transforaminal discectomy compared with primary open surgery for symptomatic lumbar degenerative disease. Orthopaedic Surg. 2019;11(4): 620-627.
[22] PAN Z, HA Y, YI S, et al. Efficacy of transforaminal endoscopic spine system (tessys) technique in treating lumbar disc herniation. Med Science Monit. 2016;22:530-539.
[23] RUETTEN S, KOMP M, MERK H, et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine. 2008;33:931-939.
[24] 唐谨,李莹,吴从俊,等.经皮椎间孔镜与椎间盘镜下手术治疗腰椎间盘突出症效果比较的Meta分析[J].中国中医骨伤科杂志,2019, 27(3):23-28.
[25] SHIN EH, CHO KJ, KIM YT, et al. Risk factors for recurrent lumbar disc herniation after discectomy. Int Orthop. 2019; 43(4):963-967.
[26] LI Z, YANG H, LIU M, et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation:a retrospective analysis of three hundred twenty-one cases. Spine (Phila Pa 1976). 2018;43(21):1463-1469. [27] SUK KS, LEE HM, MOON SH, et al. Recurrent lumbar disc herniation: results of operative management. Spine. 2001; 26(6):672-676.
[28] CARRAGEE EJ, HAN MY, SUEN PW, et al. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003; 85(1):102-108.
[29] MOBBS RJ, NEWCOMBE RL, CHANDRAN KN. Lumbar discectomy and the diabetic patient: incidence and outcome. J Clin Neurosci. 2001;8(1):10-13.
[30] PARK CH, PARK ES, LEE SH, et al. Risk factors for early recurrence after transforaminal endoscopic lumbar disc decompression. Pain Physician. 2019;22(2):E133-E138.
[31] BILGE K, ZELIHA T, UMIT A. Functional results and the risk factors of reoperations after lumbar disc surgery. Eur Spine J. 2005;14:43-48.
[32] CINOTTI G, ROYSAM GS, EISENSTEIN SM, et al. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br. 1998;80(5):825-832.
[33] KIM KT, PARK SW, KIM YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976). 2009;34(24):2674-2678.
[34] MEREDITH DS, HUANG RC, NGUYEN J, et al. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J. 2010;10(7):575-580.
[35] 郑旭浩,张小磊,江立波,等.细胞自噬在糖尿病大鼠椎间盘退变中的作用[J].中国病理生理杂志,2013,29(11):2011-2016.
[36] HEINDEL P, TUCHMAN A, HSIEH PC, et al. Reoperation Rates After Single-level Lumbar Discectomy. Spine (Phila Pa 1976). 2017;42(8):E496-E501.
[37] CHENG J, WANG H, ZHENG W, et al. Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop. 2013;37(8):1511-1517.
[38] SENCER A, YORUKOGLU AG, AKCAKAYA MO, et al. Fully endoscopic interlaminar and transforaminal lumbar discectomy: short-term clinical results of 163 surgically treated patients. World Neurosurg. 2014;82(5):884-890.
[39] SHIMIA M, BABAEI-GHAZANI A, SADAT BE, et al. Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg. 2013;8(2):93-96.
[40] 天航,刘效仿,曹正霖,等.椎间孔镜治疗腰椎间盘突出症术后复发因素的探讨[J].江西医药,2016,51(1):9-11.
[41] LEE DY, LEE SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir. 2008;48(9): 383-388. [42] YAO Y, LIU H, ZHANG H, et al. Risk factors for recurrent herniation after percutaneous endoscopic lumbar discectomy. World Neurosurg. 2017;100:1-6. |
| [1] | . Changes in Lumbosacral Sagittal Plane Parameters of L5/S1 Disc Herniation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(在线): 1-6. |
| [2] | Zhong Yizheng, Huang Peizhen, Cai Qunbin, Zheng Liqin, He Xingpeng, Dong Hang. Microstructural indexes that determine the trabecular bone maximum stress of micro-finite element models [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1313-1318. |
| [3] | Cao Sheng, Kong Lingwei, Xu Kun, Sun Zhijie. Correlation of cervical sagittal force line parameters with degenerative segment and Pfirrmann classification in patients with cervical intervertebral disc degeneration [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1319-1324. |
| [4] | Wu Tianliang, Tao Xiuxia, Xu Hongguang. Influence of different bone mineral densities on cage subsidence after stand-alone oblique lateral interbody fusion: three-dimensional finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1352-1358. |
| [5] | Liu Jinyu, Zhang Hanshuo, Cui Hongpeng, Pan Lingzhi, Zhao Boran, Li Fei, Ding Yu. Finite element biomechanical analysis of minimally invasive treatment of cervical spondylotic myelopathy and accurate exercise rehabilitation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1359-1364. |
| [6] | Wen Xinghua, Ding Huanwen, Cheng Kai, Yan Xiaonan, Peng Yuanhao, Wang Yuning, Liu Kang, Zhang Huiwu. Three-dimensional finite element model analysis of intramedullary nailing fixation design for large femoral defects in Beagle dogs [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1371-1376. |
| [7] | You Zhengqiu, Zhang Zhongzu, Wang Qunbo. Early symptomatic intervertebral disc pseudocysts after discectomy detected on MRI [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1403-1409. |
| [8] | Li Chao, Zhang Peipei, Xu Mengting, Li Linlin, Ding Jiangtao, Liu Xihua, Bi Hongyan. Respiratory training improves morphological changes of the multifidus muscle in patients with chronic nonspecific lower back pain assessed by musculoskeletal ultrasound [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1417-1421. |
| [9] | Dang Yi, Du Chengyan, Yao Honglin, Yuan Nenghua, Cao Jin, Xiong Shan, Zhang Dingmei, Wang Xin. Hormonal osteonecrosis and oxidative stress [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1469-1476. |
| [10] | Wang Yanjin, Zhou Yingjie, Chai Xubin, Zhuo Hanjie. Meta-analysis of the efficacy and safety of 3D printed porous titanium alloy fusion cage in anterior cervical discectomy and fusion [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1434-1440. |
| [11] | Jiang Xiaocheng, Shi Lu, Wang Yinbin, Li Qiujiang, Xi Chuangzhen, Ma Zefeng, Cai Lijun. Systematical evaluation of bone fusion rate after interbody fusion in patients with osteoporosis and lumbar degenerative disease treated with teriparatide [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1427-1433. |
| [12] | Yang Zhishan, Tang Zhenglong. YAP/TAZ, a core factor of the Hippo signaling pathway, is involved in bone formation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1264-1271. |
| [13] | Bai Yulong, Li Zhonghai, Zhao Yantao, Xia Cencan, Shi Lei. History, current situation and prospect of tissue banks in China [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1306-1312. |
| [14] | Sun Jiajia, Zhu Haidi, Lu Yun, Zhang Kai. Comparison of bone metabolism markers between type 2 diabetes mellitus and non-type 2 diabetes mellitus patients with hip fracture [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1156-1160. |
| [15] | Huang Linke, Wei Linhua, Jiang Jie, Liu Qian, Chen Weiwei. Effects of estrogen combined with treadmill exercise on bone mass and articular cartilage in ovariectomized mice [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1166-1171. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||