Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (31): 4989-4994.doi: 10.3969/j.issn.2095-4344.2017.31.012
Previous Articles Next Articles
Short-term efficacy of the proximal femoral nail antirotation system versus intertrochanteric antegrade nail system in the treatment of femoral intertrochanteric fracture
Liang Ning, Jiang Jun, Qiu Hai-bin, Daniel Porter, Wang Zhan-chang
- Department of Orthopedics, the First Affiliated Hospital of Tsinghua University, Beijing 100016, China
-
Online:2017-11-08Published:2017-12-01 -
Contact:Wang Zhan-chang, Master, Associate chief physician, Department of Orthopedics, the First Affiliated Hospital of Tsinghua University, Beijing 100016, China -
About author:Liang Ning, Master, Attending physician, Department of Orthopedics, the First Affiliated Hospital of Tsinghua University, Beijing 100016, China
CLC Number:
Cite this article
Liang Ning, Jiang Jun, Qiu Hai-bin, Daniel Porter, Wang Zhan-chang. Short-term efficacy of the proximal femoral nail antirotation system versus intertrochanteric antegrade nail system in the treatment of femoral intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2017, 21(31): 4989-4994.
share this article
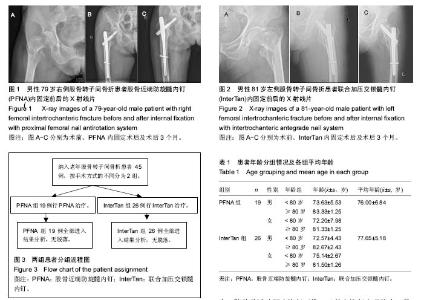
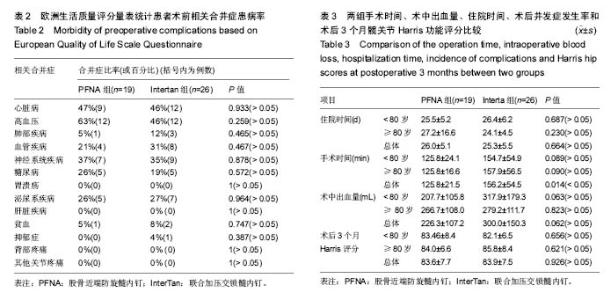
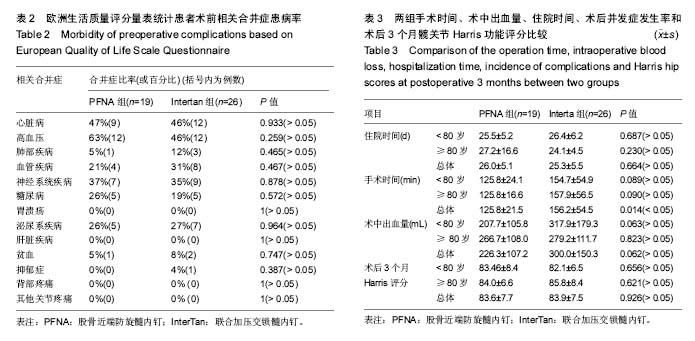
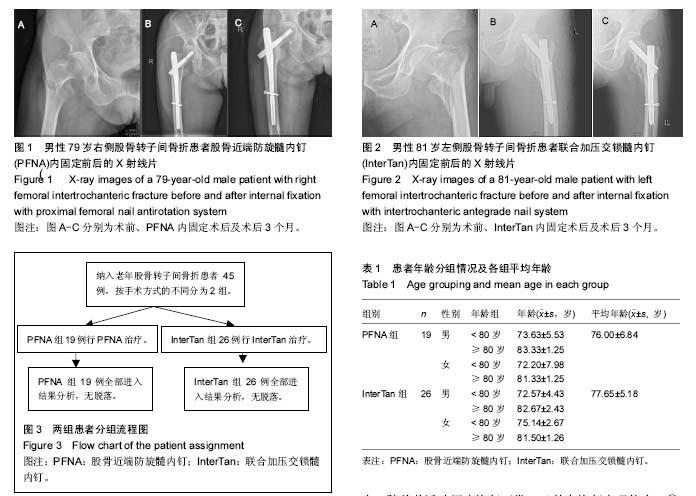
2.1 参与者数量分析 按意向性处理,纳入45例老年股骨转子间骨折患者,其中PFNA组19例,InterTan组26例,所有患者均进入结果分析,无脱落病例。患者分组流程图见图3。 2.2 基线资料比较 2组患者的性别组成及年龄差异无显著性意义;根据欧洲生活质量评分[5],显示相关合并症患病率差异无显著性意义,见表1,2。 2.3 住院时间 PFNA组患者的住院时间为16-32 d,InterTan组18-33 d,2组患者平均住院时间差异无显著性意义(P > 0.05),见表3。 2.4 手术时间 PFNA组患者的手术时间为95-165 min,InterTan组80-305 min,PFNA组平均手术时间明显缩短,且差异有显著性意义(P < 0.05),见表3。 2.5 术中出血量 PFNA组患者的术中出血量为100-500 mL,InterTan组100-800 mL,PFNA组平均术中出现量较少,但差异无显著性意义(P > 0.05),见表3。2.6 术后并发症的发生率 PFNA组共有2例患者出现了术后并发症,发生率为11%,其中泌尿系感染1例,肌间血栓1例;InterTan组共有5例患者出现了术后并发症,发生率为19%,其中泌尿系感染2例,肌间血栓3例。InterTan组术后并发症发生率较高,但2组差异无显著性意义(P > 0.05)。 2.7 术后3个月Harris功能评分 PFNA组患者术后3个月Harris评分为67-95分,InterTan组术后3个月Harris评分为68-96分,2组患者术后3个月平均Harris功能评分差异无显著性意义(P > 0.05),见表3。 "
| [1] Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporos Int. 2013;24(10):2725-2728.[2] Ong T, Anand V, Tan W, et al. Patient characteristics and outcomes of a hip fracture and comconitant fracture compared with hip fracture alone: results from a United Kingdom teaching hospital. Arch Orthop Trauma Surg. 2016; 136(4):463-467.[3] Bretherton CP, Parker MJ. Femoral medialization, fixation failures, and functional outcome in trochanteric hip fractures treated with either a sliding hip screw or an intramedullary nail from within a randomized trial. J Orthop Trauma. 2016;30(12): 642-646.[4] Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737-755.[5] Dawson J, Fitzpatrick R, Carr A, et al. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80-B:63-69.[6] Tsuda Y, Yasunaqa H, Horiquchi H, et al. Association between dementia and postoperative complications after hip fracture surgery in the elderly: analysis of 87,654 patients using a national administrative database. Arch Orthop Trauma Surg. 2015;135(11):1511-1517.[7] Switzer JA, Bozic KJ, Kates SL. Geriatric fracture care: Future trajectories: A 2015 AOA critical issues symposium. J Bone Joint Surg Am. 2017;99(8):e40.[8] Hotchen AJ, Vonberg FW, Ironside EC, et al. Predictors of infective outcomes following hip fracture:a cohort study. Gerontol Geriatr Med. 2016;2:2333721416649488.[9] Sheikh HQ, Hossain FS, Aqil A, et al. A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg. 2017;9(1): 10-18.[10] Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8): 1123-1126.[11] Novack V, Jotkowitz A, Etzion O, et al. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19(3):170-176.[12] Curtis EM, van der Velde R, Moon RJ, et al. Epidemiology of fractures in the United Kingdom 1988-2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016;87:19-26.[13] Dudko S, Kosior P, Kusz D, et al. Factors influencing treatment of proximal femoral fractures. Ortop Traumatol Rehabil. 2017;19(1):45-54.[14] Kaufer H. Mechanics of the treatment of hip injuries. Clin Orthop Relat Res. 1980;(146):53-61.[15] Adams CI, Robinson CM, Court-Brown CM, et al. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15(6):394-400.[16] Sadowski C, Lubbeke A, Saudan M, et al. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84-A(3):372-381.[17] Zhu Q, Xu X, Yang X, et al. Intramedullary nails versus sliding hip screws for AO/OTA 31-A2 trochanteric fractures in adults: A meta-analysis. Int J Surg. 2017;43:67-74.[18] Socci AR, Casemyr NE, Leslie MP, et al. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99-B(1): 128-133.[19] Bretherton CP, Parker MJ. Femoral medialization, fixation failures, and functional outcome in trochanteric hip fractures treated with either a sliding hip screw or an intramedullary nail from within a randomized trial. J Orthop Trauma. 2016;30(12): 642-646.[20] Queally JM, Harris E, Handoll HH, et al. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2014;(9):CD004961.[21] Cho HM, Lee K. Clinical and functional outcomes of treatment for Type A1 intertrochanteric femoral fracture in elderly patients: Comparison of dynamic hip screw and proximal femoral nail antirotation. Hip Pelvis. 2016;28(4):232-242.[22] Zeng X, Zhang N, Zeng D, et al. Proximal femoral nail antirotation versus dynamic hip screw fixation for treatment of osteoporotic type 31-A1 intertrochanteric femoral fractures in elderly patients. J Int Med Res. 2017;45(3):1109-1123.[23] Wang Q, Yang X, He HZ, et al. Comparative study of InterTan and dynamic hip screw in treatment of femoral intertrochanteric injury and wound. Int J Clin Exp Med. 2014; 7(12):5578-5582.[24] Sanders D, Bryant D, Tieszer C, et al. A multicenter randomized control trial comparing a novel intramedullary device (InterTan) versus convertional treatment (sliding hip screw) of geriatric hip fractures. J Orthop Trauma. 2017; 31(1): 1-8.[25] Huang Y, Zhang C, Luo Y. A comparative biomechanical study of proximal femoral nail(InterTan) and proximal femoral nail antirotation for interchanteric fractrues. Int Orthop. 2013; 37(12):2465-2473.[26] Zhang S, Zhang K, Jia Y, et al. InterTan nail versus Proximal Femoral Nail Antirotation-Asia in the treatment of unstable trochanteric fractures. Orthopedics. 2013;36(3):e288-294.[27] Queally JM, Harris E, Handoll HH, et al. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2014;9:CD004961.[28] Seyhan M, Turkmen I, Unay K, et al. Do PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures? A prospective clinical study. J Orthop Sci. 2015;20(6):1053-1061.[29] Zehir S, Sahin E, Zehir R. Comparison of clinical outcomes with three different intramedullary nailing devices in the treatment of unstable trochanteric fractures. Ulus Travma Acil Cerrahi Derq. 2015;21(6):469-476.[30] Yu W, Zhang X, Zhu X, et al. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J Orthop Surg Res. 2016;11:10.[31] Luo X, He S, Zeng D, et al. Proximal femoral nail antirotation versus hemiarthroplasty in the treatment of senile intertrochanteric fractures: Case report. Int J Surg Case Rep. 2017;38:37-42. [32] Jia L, Zhang K, Wang ZG, et al. Proximal femoral nail antirotation internal fixation in treating intertrochanteric femoral fractures of elderly subjects. J Biol Regul Homeost Agents. 2017;31(2):329-334.[33] Shin WC, Seo JD, Lee SM, et al. Radiographic Outcomes of Osteosynthesis Using Proximal Femoral Nail Antirotation (PFNA) System in Intertrochanteric Femoral Fracture: Has PFNA II Solved All the Problems? Hip Pelvis. 2017;29(2): 104-112. [34] Zhang H, Zeng X, Zhang N, et al. INTERTAN nail versus proximal femoral nail antirotation-Asia for intertrochanteric femur fractures in elderly patients with primary osteoporosis. J Int Med Res. 2017;45(4):1297-1309. [35] Shin YS, Chae JE, Kang TW, et al. Prospective randomized study comparing two cephalomedullary nails for elderly intertrochanteric fractures: Zimmer natural nail versus proximal femoral nail antirotation II. Injury. 2017;48(7): 1550-1557. [36] Esen E, Dur H, Atao?lu MB, et al. Evaluation of proximal femoral nail-antirotation and cemented, bipolar hemiarthroplasty with calcar replacement in treatment of intertrochanteric femoral fractures in terms of mortality and morbidity ratios. Eklem Hastalik Cerrahisi. 2017;28(1):35-40. [37] Sonmez MM, Camur S, Erturer E, et al. Strategies for Proximal Femoral Nailing of Unstable Intertrochanteric Fractures: Lateral Decubitus Position or Traction Table. J Am Acad Orthop Surg. 2017;25(3):e37-e44. [38] Zeng X, Zhan K, Zhang L,et al. Conversion to total hip arthroplasty after failed proximal femoral nail antirotations or dynamic hip screw fixations for stable intertrochanteric femur fractures: a retrospective study with a minimum follow-up of 3 years. BMC Musculoskelet Disord. 2017;18(1):38. [39] Park BJ, Cho HM, Min WB.Surgical Treatment of Undisplaced Femur Neck Fractures in Dementia Patients Using Proximal Femoral Nail Antirotation.Hip Pelvis. 2015;27(3):164-172. [40] Jiang X, Wang Y, Ma X, et al. Proximal Femoral Nail Antirotation Versus Reverse Less Invasive Stabilization System-distal Femur for Treating Proximal Femoral Fractures: A Meta-analysis.Medicine (Baltimore). 2016;95(14):e3168. |
| [1] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [2] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [3] | Xu Xinzhong, Wu Zhonghan, Yu Shuisheng, Zhao Yao, Xu Chungui, Zhang Xin, Zheng Meige, Jing Juehua. Biomechanical analysis of different ways of inserting Steinmann Pins into the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1313-1317. |
| [4] | Wei Guoqiang, Li Yunfeng, Wang Yi, Niu Xiaofen, Che Lifang, Wang Haiyan, Li Zhijun, Shi Guopeng, Bai Ling, Mo Kai, Zhang Chenchen, Xu Yangyang, Li Xiaohe. Biomechanical analysis of non-uniform material femur under different loads [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1318-1322. |
| [5] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [6] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [7] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [8] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [9] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [10] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [11] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [12] | Tian Chuan, Zhu Xiangqing, Yang Zailing, Yan Donghai, Li Ye, Wang Yanying, Yang Yukun, He Jie, Lü Guanke, Cai Xuemin, Shu Liping, He Zhixu, Pan Xinghua. Bone marrow mesenchymal stem cells regulate ovarian aging in macaques [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 985-991. |
| [13] | Hu Wei, Xie Xingqi, Tu Guanjun. Exosomes derived from bone marrow mesenchymal stem cells improve the integrity of the blood-spinal cord barrier after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 992-998. |
| [14] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [15] | Hou Jingying, Guo Tianzhu, Yu Menglei, Long Huibao, Wu Hao. Hypoxia preconditioning targets and downregulates miR-195 and promotes bone marrow mesenchymal stem cell survival and pro-angiogenic potential by activating MALAT1 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1005-1011. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||