Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (28): 4529-4535.doi: 10.3969/j.issn.2095-4344.2017.28.017
Previous Articles Next Articles
Establishment and assessment of small animal models of osteoarthritis
Wu Wei, Li Hui, Zou Jun, Wang Miao
- Shanghai University of Sport, Shanghai 200438, China
-
Revised:2017-06-16Online:2017-10-08Published:2017-11-10 -
Contact:Wang Miao, Teaching assistant, Physician, Shanghai University of Sport, Shanghai 200438, China -
About author:Wu Wei, Master, Teaching assistant, Shanghai University of Sport, Shanghai 200438, China -
Supported by:the National Natural Science Foundation of China, No. 81572242; the Key Laboratory of Human Sports Ability Development and Guarantee in Shanghai (Shanghai University of Sport), No. 11DZ2261100
CLC Number:
Cite this article
Wu Wei, Li Hui, Zou Jun, Wang Miao. Establishment and assessment of small animal models of osteoarthritis[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(28): 4529-4535.
share this article

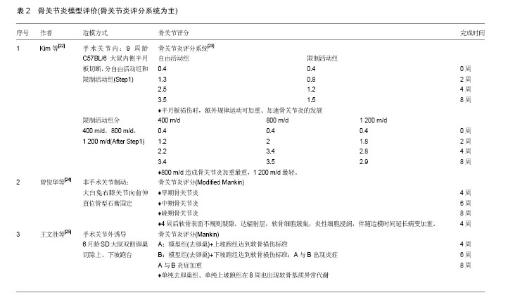
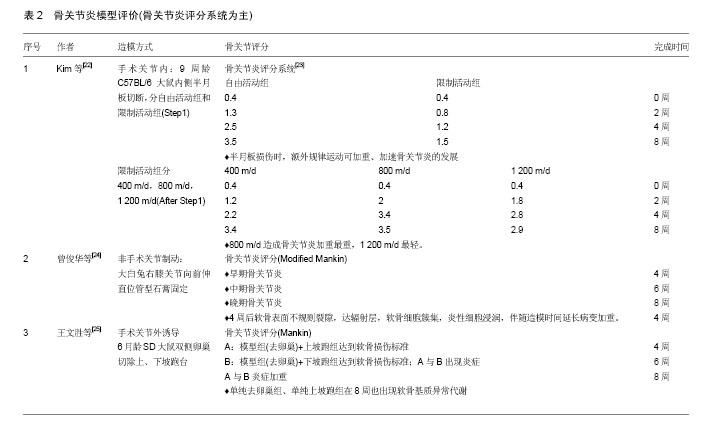
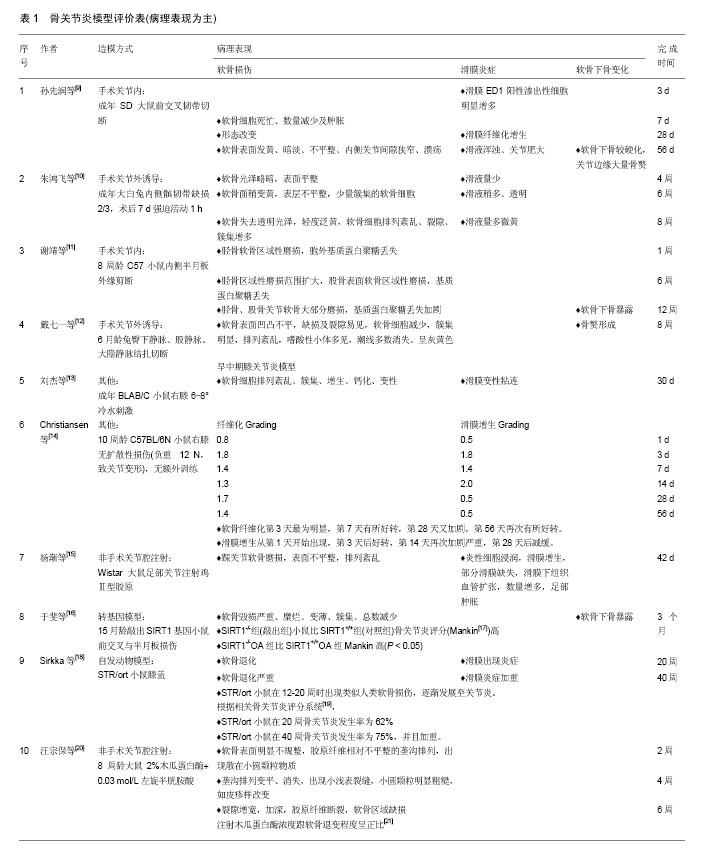
2.1 骨关节炎建模方法 骨关节炎模型的制造主要有非手术类、手术类、自发动物模型及转基因模型等[2]。非手术类包括关节制动及关节腔注射,手术类包括关节内手术及关节外诱导,自发动物模型主要包括C57黑鼠、Hartley豚鼠、B6C3F1栗鼠和转基因动物模型等[3]。本文将近几年内有关骨关节炎小动物模型非手术关节制动、非手术关节腔注射、关节内手术、手术关节外诱导、自发动物模型、转基因模型及其他建模方式中具有代表性的文章进行汇总,详见表1,2。 骨关节炎的病理基础主要有3方面,分别为软骨损伤、软骨下骨变化及滑膜炎症。软骨损伤包括软骨磨损、糜烂、溃疡等,软骨下骨变化包括硬化、骨赘,滑膜炎症包括滑膜增生、引起炎症程度等[4-5]。骨关节炎评价方法有骨关节炎评分(OA Score)、病理组织形态评价、炎症标志物(Inflammatory Marker)和影像学等[6-8]。本文骨关节炎模型评价主要从模型的病理表现及相关的骨关节炎评分系统两方面进行总结,详见表1,2。"
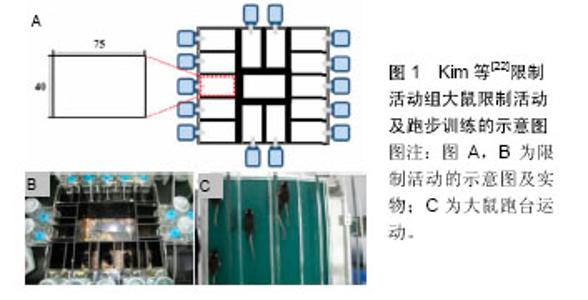
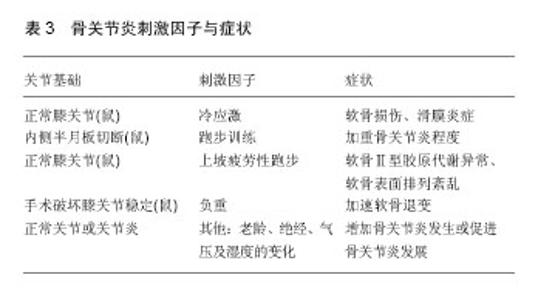
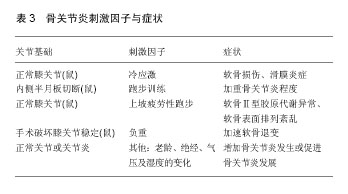
2.2 刺激模型的因子 骨关节炎的刺激因子加速了关节炎的发展,使之趋于恶化。骨关节炎是一种以软骨破坏、软骨下骨硬化及滑膜炎症为特征的退行性关节疾病,当软骨破损时由于软骨内无血管且缺乏神经支配,导致自愈能力差且软骨损伤初期对损伤疼痛敏感较低[26-27]。某些刺激因子通过对软骨的刺激持续破坏软骨,促进了骨关节炎的发展。刺激因子还可通过刺激滑膜大量分泌滑液,造成滑膜炎症,损害软骨,同样促进骨关节炎的发展[28]。本文将近几年常见刺激因子总结如下: 刘杰等[13]将BLAB/C小鼠右膝进行6-8 ℃冷水刺激,1.5 h/d,未对小鼠右膝进行其他任何处理造成损伤,30 d后出现软骨损伤及滑膜炎症的症状。冷刺激可造成关节软骨损伤及滑膜炎症,促进骨关节炎的发展。Kim等[22]将C57BL/6大鼠内侧半月板切断制造模型后,分成自由活动组和限制活动组(仅限原地活动),见图1。经过8周观察发现,额外规律运动(自由活动)可加重、加速骨关节炎的发展。在此基础上,每天对限制活动组大鼠进行跑步训练,依次分为400 m/d、800 m/d和1 200 m/d,再经过8周后发现,800 m/d的跑量对大鼠骨关节炎的程度加重最严重。骨关节炎发生时,额外的运动可促进其发展。钟名金等[29]研究发现,大白兔骨关节炎时,与笼养自由活动相比,早期合理的运动并不会加重膝关节软骨损伤(运动始于术后第5天,运动强度为5 d/周,10 min/d,跑台速度为0.3英里/h)。Wang等[25]研究中发现,仅单纯行上坡疲劳性跑步训练8周后(坡度+15°,跑台的训练频率为28 m/min、60 min/d、6 d/周),软骨Ⅱ型胶原即可出现异常代谢。Tang等[30]研究发现,16-18周龄健康Wistar大鼠(未经任何处理)6周完成坡度5°的30 km跑台训练后,其软骨表面染色(India ink)变得不规律,异染性(safranin-O)几乎消失,Mankin评分达到骨关节炎水平。 李炳辉等[31]将大白兔右膝用手术方法将其关节稳定性破坏后,再进行2 h/d的直立负重,并且制造经典的Hulth模型作比较。研究发现,直立负重可使关节软骨在短期内发生退变,促进骨关节炎的发展。 流行病学研究中,骨关节炎与年龄密切相关。大数据研究发现,欧洲国家男性50岁、女性40岁以后骨关节炎的发生率明显上升,65岁以后为50%,75岁以后高达85%[32]。国内研究中发现,40岁以后患膝骨关节炎的概率增加,且随着年龄的增长,膝骨关节炎的发生呈不断增高的趋势,女性较男性患膝骨关节炎更高[33]。关节炎是老年人常见的退行性疾病,随着年龄的增长,关节软骨退变、破损,软骨下骨骨赘,滑膜炎症等日趋严重,影响膝关节的结构和功能。而女性绝经后,患骨关节炎的概率较高,其原因可能是雌激素水平下降后,通过作用于软骨和软骨下骨的雌激素受体,影响关节软骨周围内环境,导致软骨退变[34]。在周君等[35]研究中,成功利用去卵巢新西兰白兔,10周后其软骨出现明显退变。此过程中,没有进行任何造成膝关节损伤的措施。 当运动强度过大可导致正常关节软骨损伤,且会加重已损伤的关节软骨及滑膜炎症等。负重及冷应激可刺激软骨、滑膜等,促进骨关节炎发展。年龄和女性绝经的因素也是影响骨关节炎发生发展的重要因子。此外,气压及湿度变化等因子也可以促进骨关节炎的发展[36-37]。详见表3。"
| [1] Iversen MD. Rehabilitation in terventions for pain and disability in osteoarthritis: a review of interventions including exercise, manual techniques, and assistive devices. Orthop Nurs. 2012;31(2):103-108.[2] Sunk IG, Bobacz K, Hofstaetter JG, et al. Increased expression of discoidin domain receptor 2 is linked to the degree of cartilage damage in human knee joints: a potential role in osteoarthritis pathogenesis. Arthritis Rheum. 2007; 56(11):3685-3692. [3] He MJ, Jing L, Tao ZK, et al. Optimal animal model of osteoarthritis. Chinese Journal of Tissue Eng Res. 2013; 17(46):8096-8074.[4] Bellido M, Lugo L, Roman-Blas JA, et al. Subchondral bone microstructural damage by increased remodeling aggravates experimental osteoarthritis preceded by osteoporosis. Arthritis Res Ther. 2010;12(4):R152.[5] Schroeppel JP, Crist JD, Anderson HC, et al. Molecular regulation of articular chondrocyte function and its significance in osteoarthritis. Histol Histopathol. 2011;26(3): 377-394.[6] Little CB, Smith MM. Animal models of osteoarthritis. Current Rheumatology Reviews. 2008;4(4):175-182.[7] Thote T, Lin AS, Raji Y, et al. Localized 3 D analysis of cartilage composition and morphology in small animal models of joint degeneration. Osteoarthritis Cartilage. 2013;21(8): 1132-1141.[8] Garcia-Arnandis I, Guillen M, Gomar F, et al. High-mobility group box 1 potentiates the proin-flammatory effects of interleukin 1β in osteoarthritic synoviocytes. Arthritis Res Ther. 2010;12:R165. [9] 孙先润,唐涛,李跃琼,等.SD大鼠膝前交叉韧带切断后骨关节的变化[J].中国矫形外科杂志.2013,21(22):2294-2298.[10] 朱鸿飞,冯伟,刘益杰,等.髌韧带内侧缺损构建兔膝骨关节炎模型初探[J].上海中医药杂志.2012,46(1):11-18.[11] 谢靖,杨冠.一种新的半月板切断导致小鼠骨关节炎建立的方法[J].军事医学, 2013,37(9):708-711.[12] 戴七一,覃学流,袁经阳,等.兔骨内高压型膝关节骨性关节炎模型的建立[J]. 中国组织工程研究与临床康复,2011,15(20): 3645-3648. [13] 刘杰,王晓黎,郭俊生.冷应激引发小鼠骨关节炎模型的建立[J].环境与职业医学.2011,28(5):289-292.[14] Christiansen BA, Anderson MJ, Lee CA, et al. Musculoskeletal changes following non-invasive knee injury using a novel mouse model of post-traumatic osteoarthritis. Osteoarthritis Cartilage. 2012;20(2012):773-782.[15] Yang J, Cai HD, Zeng YL, et al. Establishment and evaluation the arthritis model induced by collagen in rats. Strait Pharmaceut J. 2014;26(9):27-31.[16] 于斐,雷鸣,曾晖,等. 高龄小鼠沉默信息调节因子1基因敲除后膝骨关节炎模型的建立[J]. 中国组织工程研究, 2015,19(49): 7895-7901. [17] Mankin HJ, Dorfman H, Lippiello L, et al. Biochemical and metabolic abnormalities in articular cartilage from osteoarthritic human hips. II. Correlation of morphology with biochemical and metabolic data. J Bone Joint Surg Am. 1971;53(3):523-537.[18] Kyostio-Moore S, Nambiar B, Hutto E, et al. STR/ort mice, a model for spontaneous osteoarthritis, exhibit elevated levels of both local and systemic Inflammatory markers. Comp Med. 2011;61(4):346-355.[19] Chambers MG, Kuffner T, Cowan SK, et al. Expression of collagen and aggrecan genes in normal and osteoarthritic murine knee joints. Osteoarthritis Cartilage. 2002;10:51-61. [20] Wang ZB, Xu YL, Liao WM, et al. Cartilage surface of early osteoarthritis in rats induced by papain under scanning electron microscope. Chin J Tissue Eng Res. 2014;18(2): 177-182.[21] 韩冠英,凌沛学,王凤山,等.不同浓度木瓜蛋白酶建立兔膝骨关节炎模型的比较研究[J].中国骨伤.2012,5(25):424-429. [22] Kim BJ, Kim DW, Kim SH, et al. Establishment of a reliable and reproducible murine osteoarthritis model. Osteoarthritis Cartilage. 2013;21(2013):2013-2020.[23] Glasson S, Blanchet T, Morris E. The surgical destabilization of the medial meniscus (DMM) model of osteoarthritis in the 129/Sv Ev mouse. Osteoarthritis Cartilage. 2007;15: 1061-1069.[24] 曾俊华,马笃军,彭力平,等.实验兔膝骨关节炎模型的建立及鉴定[J].中国临床研究,2016,29(5):679-682.[25] Wang WS, Chen W, Shen BL, et al. Effect of uphill or downhill running training on articular cartilage degeneration and inflammatory responses of knee osteoarthritis rats. Chin J Tissue Engi Res. 2016;20(2):197-201. [26] Otrock ZK, Mahfouz RA, Makarem JA, et al. Understanding the biology of angiogenesis: review of the most important molecular mechanisms. Blood Cells Mol Dis. 2007;39(2): 212-220.[27] Fowkes LA, Toms AP. Bone marrow oedema of the knee. Knee.2010;17(1):1-6.[28] Ayral X. Synovitis: a potential predictive factor of structural progression of medial tibiofemoral knee osteoarthritis-results of a 1 year longitudinal arthroscopic study in 422 patients. Osteoarthritis Cartilage. 2005;13:361-367.[29] 钟名金,刘振龙,张继英,等.跑台运动对兔前交叉韧带断裂后膝关节软骨的影响[J].中国运动医学杂志,2016,35(4):349-356.[30] Tang T, Muneta T, Nimura A, et al. Serum keratan sulfate transiently increases in the early stage of osteoarthritis during strenuous running of rats: protective effect of intraarticular hyaluronan injection. Arthritis Res Ther. 2008;10:R13.[31] 李炳辉,牛东生,孙玺淳,等.直立负重法与Hulth法建立兔膝骨关节炎模型的对比研究[J].宁夏医科大学学报,2013,35(3): 256-262.[32] Abstracts of the IOF-ECCEO12 European Congress on Osteoporpsis and Osteoarthritis, March 21-24, 2012 and the 2nd IOF-ESCEO Pre-clinical Symposium, March 23-24, 2012, Bordeaux, France. Osteoporpsis Int, 2012;23(Suppl 2 ):25-35.[33] 赵昌盛,钟群杰,林剑浩.中国膝关节骨关节炎流行病学调查现状[J].广东医学,2016;37(13):2050-52.[34] Roman-Blas JA, Casta ES, Largo R, et al. Osteoarthritis associated with estrogen deficiency. Arthritis Res Ther. 2009;11(5):241.[35] 周君,郭华,夏璐,等.去卵巢对兔膝关节软骨及基质金属蛋白酶-13表达的影响[J].中国老年学杂志,2102;10(32):4235-4237.[36] Tsai WS, Yang YH, Wang LC, et al. Abrupt temperature change triggers arthralgia in patients with juvenile rheumatoid arthritis. J Microbiol Immunol Infect. 2006;39(6):465-470.[37] Patberg WR, Rasker JJ. Weather effects in rheumatoid arthritis:from controversy to consensus A review. J Rheumatol. 2004;31:1327-1334.[38] Gregory MH, Capito N, Kuroki K, et al. A review of translational animal models for knee osteoarthritis.Arthritis. 2012;2012:764621.[39] Niu HJ, Wang Q. Ultrasonic reflection coefficient and surface roughness index of OA articular cartilage: relation to pathological assessment. BMC Musculoskeletal Disoeders. 2012;13:1-137.[40] Pedersen DR, Goetz JE, Kurriger GL, et al. Comparative digital cartilage histology for human and common osteoarthritis models. Orthop Res Rev. 2013;2013(5):13-20.[41] Yang SB, Liu YJ, Feng W, et al. Establishment of knee osteoarthritis models in rabbits based on joints’ mechanical instability method. SH J TCM Apr. 2015;49(4):11-15.[42] Sun YS, Yao YF, Fang D, et al. Expression of Indian hedgehog protein and Runt related transcription factor 2 in rats with osteoarthritis caused by anterior cruciate ligament transection. Chin J Tissue Eng Res. 2015;19(18):2820-2824. [43] 熊元,赵振国,李传郡,等.兔膝骨关节炎模型的制备及鉴定[J].实验动物科学,2013,30(3):31-34.[44] Chen K, Chen ZJ, Fu HN, et al. Investigation on the establishment of rabbit Knee osteoarthritis model. Laboratory Animal Science. 2014;31(5):33-35.[45] Zhang RK, Yang LK, Ye ZQ, et al. Establishing a rat osteoarthritis model based on knee joint instability. Chin J Tissue Eng Res. 2013;17(37):6628-6635. [46] Sunk IG, Bobacz K, Hofstaetter JG, et al. Increased expression of discoidin domain receptor 2 is linked to the degree of cartilage damage in human knee joints: a potential role in osteoarthritis pathogenesis. Arthritis Rheum. 2007; 56(11):3685-3692.[47] Rodriguez RR, Seegmiller RE, Stark MR, et al. A type XI collagen mutation leads to increased degradation of type II collagen in articular cartilage. Osteoarthritis Cartilage. 2004;12(4):314-320.[48] Zhou C,You Y, Shen WX, et al. Deficiency of sorting nexin 10 prevents bone erosion in collagen-induced mouse arthritis through promoting NFATc1 degradation. Ann Rheum. 2016;75: 1211-18.[49] 乙军,周业庭,徐丹,等.实验性兔膝骨关节炎模型的建立[J].临床和实验医学杂志,2012,11(24):1921-23.[50] Rutgers M, van Pelt MJ, Dhert WJ, et al. Evaluation of histological scoring systems for tissue-engineered, repaired and osteoarthritic cartilage. Osteoarthritis Cartilage. 2010; 18(1):12-23.[51] Gerwin N, Bendele AM, Glasson S, et al. The OARSI histopathology initiative: recommendations for histological assessments of osteoarthritis in the rat. Osteoarthritis Cartilage. 2010;18(suppl 3):S24–S34.[52] McCoy AM. Animal models of osteoarthritis: comparisons and key considerations. Vet Pathol. 2015;52(5):803-818.[53] Poole R, Blake S, Buschmann M, et al. Recommendations for the use of preclinical models in the study and treatment of osteoarthritis.Osteoarthritis Cartilage. 2010, 18(suppl 3): S10-S16.[54] Loeser RF, Olex AL, McNulty MA, et al. Microarray analysis reveals agerelated differences in gene expression during the development of osteoarthritis in mice. Arthritis Rheum. 2012; 64(3):705-717.[55] Cook JL, Hung CT, Kuroki K, et al. Animal models of cartilage repair.Bone Joint Res. 2014; 3(4):89-94.[56] Arzi B, Wisner ER, Huey DJ, et al. A proposed model of naturally occurring osteoarthritis in the domestic rabbit.Lab Anim (NY). 2012;41(1):20-25.[57] Glassony SS, Chambersz MG, Van Den Berg WB, et al. The OARSI histopathology initiativeerecommendations for histological assessments of osteoarthritis in the mouse. Osteoarthritis Cartilage. 2010;18:S17-S23. |
| [1] | Zhang Jichao, Dong Yuefu, Mou Zhifang, Zhang Zhen, Li Bingyan, Xu Xiangjun, Li Jiayi, Ren Meng, Dong Wanpeng. Finite element analysis of biomechanical changes in the osteoarthritis knee joint in different gait flexion angles [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1357-1361. |
| [2] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [3] | Jin Tao, Liu Lin, Zhu Xiaoyan, Shi Yucong, Niu Jianxiong, Zhang Tongtong, Wu Shujin, Yang Qingshan. Osteoarthritis and mitochondrial abnormalities [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1452-1458. |
| [4] | Wang Baojuan, Zheng Shuguang, Zhang Qi, Li Tianyang. Miao medicine fumigation can delay extracellular matrix destruction in a rabbit model of knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1180-1186. |
| [5] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [6] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [7] | Liu Dongcheng, Zhao Jijun, Zhou Zihong, Wu Zhaofeng, Yu Yinghao, Chen Yuhao, Feng Dehong. Comparison of different reference methods for force line correction in open wedge high tibial osteotomy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 827-831. |
| [8] | Zhou Jianguo, Liu Shiwei, Yuan Changhong, Bi Shengrong, Yang Guoping, Hu Weiquan, Liu Hui, Qian Rui. Total knee arthroplasty with posterior cruciate ligament retaining prosthesis in the treatment of knee osteoarthritis with knee valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 892-897. |
| [9] | He Junjun, Huang Zeling, Hong Zhenqiang. Interventional effect of Yanghe Decoction on synovial inflammation in a rabbit model of early knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 694-699. |
| [10] | Lin Xuchen, Zhu Hainian, Wang Zengshun, Qi Tengmin, Liu Limin, Suonan Angxiu. Effect of xanthohumol on inflammatory factors and articular cartilage in a mouse mode of osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 676-681. |
| [11] | Xu Lei, Han Xiaoqiang, Zhang Jintao, Sun Haibiao. Hyaluronic acid around articular chondrocytes: production, transformation and function characteristics [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 768-773. |
| [12] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [13] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [14] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [15] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||