Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (27): 4409-4415.doi: 10.3969/j.issn.2095-4344.2017.27.025
Previous Articles Next Articles
Lateral lumbar interbody fusion for adult degenerative scoliosis: how to provide evidence supports
Jin Yuan-zhe, Gong Wei-quan, Zhang Shao-kun
- the First Hospital of Jilin University, Changchun 130021, Jilin Province, China
-
Online:2017-09-28Published:2017-10-24 -
Contact:Zhang Shao-kun, M.D., the First Hospital of Jilin University, Changchun 130021, Jilin Province, China -
About author:Jin Yuan-zhe, Master, the First Hospital of Jilin University, Changchun 130021, Jilin Province, China -
Supported by:the Project of Ministry of Science and Technology of China, No. 2009ZX09502-011
CLC Number:
Cite this article
Jin Yuan-zhe, Gong Wei-quan, Zhang Shao-kun. Lateral lumbar interbody fusion for adult degenerative scoliosis: how to provide evidence supports [J]. Chinese Journal of Tissue Engineering Research, 2017, 21(27): 4409-4415.
share this article
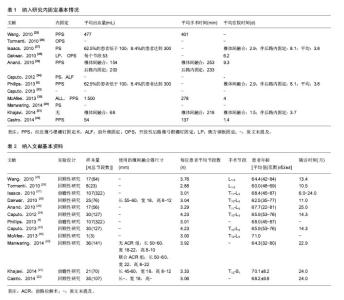
2.1 纳入文献的基本情况 共检索到165篇相关文献,根据题目和摘要进行筛选后余下23篇进行全文阅读筛选[5,9-30]。23篇中10篇由于纳入人群包含了除退行性脊柱侧凸之外的其他疾病患者,却没有对他们的数据进行分开报道而被排除[9-18];1篇纳入了退行性脊柱侧凸患者,使用了不同的干预措施,但由于未将其数据分开报道而被排除[19],随后剩余12篇文章纳入本综述[5,20-30],见表1。 纳入的研究均为观察性研究,其中3篇为前瞻性[5,21,27],其他为回顾性。其中Isaacs和Phillips两篇文献的数据来源于一个研究[5,27],Caputo的2篇文章虽未指出,但似乎也是来源于同一研究[23-24]。除2篇文献之外其他研究的样本量都较少[5,27],样本量不足40。纳入个体的平均年龄60-70岁。除了Castro等的研究外[22],其他研究中都使用了不同的内固定技术(表2)。 "
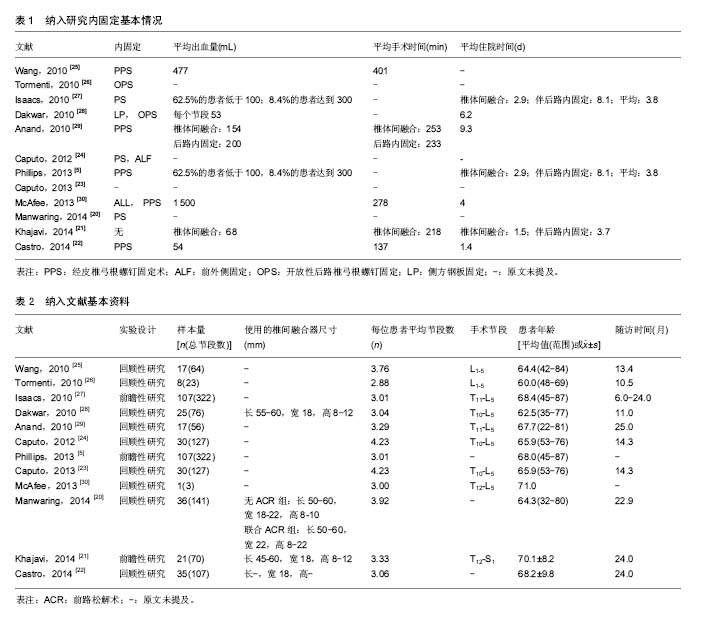
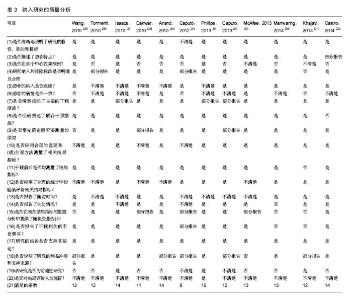
平均随访时间10.5-24个月之间。Manwaring等[20]的研究中患者被分为联合前路松解术(anterior column realignment,ACR)组和无前路松解术组。由于McAfee,Wang等[25,30]的研究纳入了其他疾病的患者,文章提取数据时仅提取了退行性脊柱侧凸患者的数据并对提取的数据进行了计算。Anand等的研究中由于只单独报告了退行性脊柱侧凸患者的手术相关数据,所以在其他结局的分析中并没有纳入此研究中的数据(表1)[29]。 2.2 纳入文献的质量评估 由于所有的研究都是病例系列研究,所以均使用了加拿大卫生经济研究所病例系列方法学质量评价工具对其进行评价。在12个研究中[5,20-30],Isaacs,Phillips,Dakwar,Castro等[5,22,27-28]的文献满足的项目不低于14条,所以文章认为这4篇文献所对应的研究质量较高。在各项目中,超过一半的文献不满足“是否在多个中心收集病例”(9篇),“患者的病情是否一致”(10篇),“该研究是否为前瞻性研究”(9篇)和“是否对结局评价人员施盲”(11篇)等项目(表3)。"

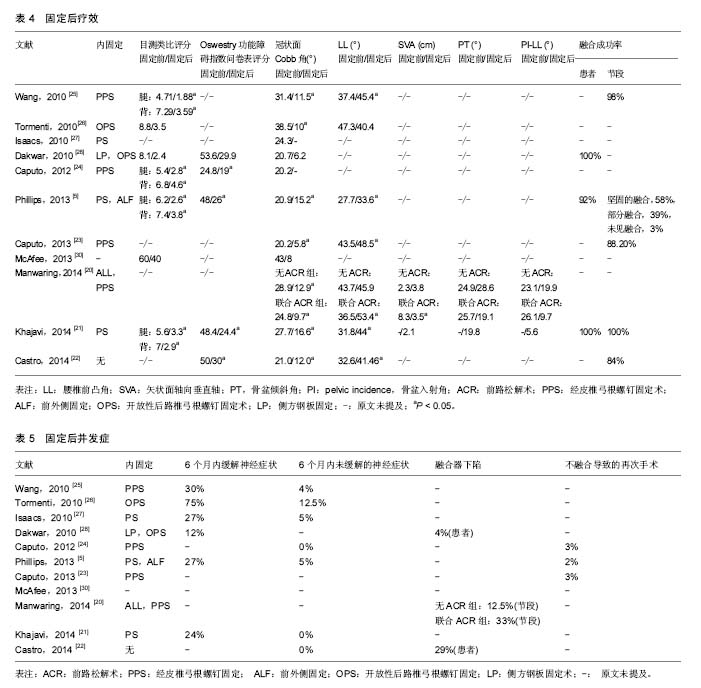
2.3 侧入路椎体间融合方法 在3篇单独报告椎体间融合的出血量研究当中[21-22,29],其血量在54-154 mL;当联合其他入路手术时,平均出血量增加200 mL[29]。但除了McAfee等[30]的研究外,其他研究平均出血量均未超过400 mL。单纯椎体间融合所需时间在137-253 min,平均每个节段所需时间为45-76 min。单纯椎体间融合后平均住院时间为1.4-2.9 d,合并其他内固定手术时住院时间在3.7-9.3 d。 所有研究中使用的植骨融合器大小较一致,长度均在45-60 mm,宽为18-22 mm,高为8-12 mm。在联合前路松解术的研究组中,使用的融合器长50-60 mm,高8-22 mm,宽22 mm,后倾角约30°。 2.4 侧入路椎体间融合治疗的临床指标 共有7篇文献报道了目测类比评分值的变化[5,24-26,28,30],其中有4篇报道了患者腿和后背的目测类比评分值在固定后较术前的改善差异有显著性意义[5,21,24-25]。除了McAfee等[30]的报道之外,其他研究中腿和背部的目测类比评分平均变化值均在2分以上(范围:腿2.3-3.6分;腰背2.2-4.1分)。共有5篇文献报道了Oswestry功能障碍指数问卷表评分值术前固定后的变化[5,21-22,24,28],其中4篇报道了其变化有显著性意义[5,21-22,24]。除了Caputo等于2012年发表的文献外,其他文献Oswestry功能障碍指数问卷表评分减少值都在20分以上(20-24分)。 2.5 侧入路椎体间融合的影像学资料 见表4。共有9篇文献报道了侧入路椎体间融合固定后冠状面Cobb角的矫正结果,所有的研究中Cobb角均有降低[5,20-23,25-26,28,30]。其中7篇文献表明固定前后Cobb角之间差异有显著性意义,矫正幅度范围在5.7°-28.5°之间[5,20-23,25-26]。矫正幅度在研究间的差异较大,但固定后Cobb角都在5.8°-16.6°。共有7篇文献报道了术前固定后的腰椎前凸角变化幅度[5,20-23,25-26],其中6篇中变化值有显著性意义[5,20-23,25],范围5°-12.2°。除了Khajavi等的研究外[21],其他研究均小于10°。仅Manwaring等的文献报道了矢状面轴向垂直轴,骨盆倾斜角,骨盆入射角与腰椎前凸角之差等值得固定前后变化[20],其中联合前路松解术组在固定后矢状面轴向垂直轴较术前的变化明显有显著性意义(术前8.3 cm,固定后3.5 cm,P < 0.017),骨盆倾斜角由术前的25.7°降低到19.1°,骨盆入射角与腰椎前凸角之差由术前的26.1°矫正为固定后的9.7°。无前路松解术组的矢状面轴向垂直轴由2.3升高到3.8,骨盆倾斜角由24.9°升到28.6°,骨盆入射角与腰椎前凸角之差由术前的23.1°矫正为19.9°[20]。Khajavi等[21]的文章中仅发表了固定后矢状面轴向垂直轴,PI和骨盆倾斜角的值,其中固定后矢状面轴向垂直轴为2.07 cm,骨盆倾斜角为19.8°,腰椎前凸角与PI之差为5.6°。共有6篇文献报告了固定后融合的成功率,92%-100%的患者和84%-98%的节段显示了骨性融合[5,21-23,25,28]。 2.6 侧入路椎体间融合的并发症 研究结果表明,固定后立即发生神经症状的风险较高。Tormenti[26]等的研究结果表明,6例(75%)患者出现了大腿感觉障碍或运动障碍;Caputo等[24]于使用了“相当一部分的患者”来形容发生此并发症的发生率。其他的研究中,此并发症的发生率在12%-30%。尽管在固定后此并发症发生率较高,但是大部分的症状均在6个月内可缓解。绝大部分研究的报告中,6个月内未得到缓解的比例患者比例为0%-5%(表5)。 3个研究报告了椎间融合器下陷的发生率,其中使用了前路钢板或者后路椎弓根进行固定的组中发生率为4%,而在行单纯椎体间融合的研究中,发生率为29%[20,22,28]。因为骨不融合而需要重新手术的并发症发生率为2%-3%。"
| [1] Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30(9):1082-1085.[2] Cho KJ, Kim YT, Shin SH, et al. Surgical treatment of adult degenerative scoliosis. Asian Spine J. 2014;8(3):371-381.[3] Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2-18.[4] Pawar A, Hughes A, Girardi F, et al. Lateral Lumbar Interbody Fusion. Asian Spine J. 2015;9(6):978-983.[5] Phillips FM, Isaacs RE, Rodgers WB, et al. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine (Phila Pa 1976). 2013; 38(21):1853-1861.[6] Phan K, Rao PJ, Scherman DB, et al. Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci. 2015;22(11):1714-1721.[7] Keorochana G, Setrkraising K, Woratanarat P, et al. Clinical outcomes after minimally invasive transforaminal lumbar interbody fusion and lateral lumbar interbody fusion for treatment of degenerative lumbar disease: a systematic review and meta-analysis. Neurosurg Rev. 2016. Doi: 10.1007/s10143-016-0806-8.[8] 王小琴,陈耀龙,渠清源,等.病例系列研究方法学质量评价工具解读[J].中国循证儿科杂志,2015,10(5):381-385.[9] Malham GM, Ellis NJ, Parker RM, et al. Maintenance of Segmental Lordosis and Disc Height in Standalone and Instrumented Extreme Lateral Interbody Fusion (XLIF). J Spinal Disord Tech. 2016. DOI: 10.1097/BSD. 0b013e3182aa4c94[10] Lee YS, Park SW, Kim YB. Direct lateral lumbar interbody fusion: clinical and radiological outcomes. J Korean Neurosurg Soc. 2014; 55(5):248-254.[11] Kim SJ, Lee YS, Kim YB, et al. Clinical and radiological outcomes of a new cage for direct lateral lumbar interbody fusion. Korean J Spine. 2014;11(3):145-151.[12] Johnson RD, Valore A, Villaminar A, et al. Pelvic parameters of sagittal balance in extreme lateral interbody fusion for degenerative lumbar disc disease. J Clin Neurosci. 2013;20(4):576-581.[13] Ahmadian A, Verma S, Mundis GM Jr., et al. Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4-5 spondylolisthesis: clinical outcomes. J Neurosurg Spine. 2013;19(3):314-320.[14] Marchi L, Oliveira L, Amaral R, et al. Anterior elongation as a minimally invasive alternative for sagittal imbalance-a case series. HSS J. 2012; 8(2):122-127.[15] Le TV, Vivas AC, Dakwar E, et al. The effect of the retroperitoneal transpsoas minimally invasive lateral interbody fusion on segmental and regional lumbar lordosis. Scientific World J. 2012;2012: 516706.[16] Sharma AK, Kepler CK, Girardi FP, et al. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 2011;24(4):242-250.[17] Karikari IO, Nimjee SM, Hardin CA, et al. Extreme lateral interbody fusion approach for isolated thoracic and thoracolumbar spine diseases: initial clinical experience and early outcomes. J Spinal Disord Tech. 2011;24(6):368-375.[18] Acosta FL, Liu J, Slimack N, et al. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine. 2011;15(1):92-96.[19] 吴增晖,冯永辉,马向阳,等.成人退行性腰椎侧凸的外科治疗[J].中国骨科临床与基础研究杂志,2011,3(1):18-21.[20] Manwaring JC, Bach K, Ahmadian AA, et al. Management of sagittal balance in adult spinal deformity with minimally invasive anterolateral lumbar interbody fusion: a preliminary radiographic study. J Neurosurg Spine. 2014;20(5):515-522.[21] Khajavi K, Shen AY. Two-year radiographic and clinical outcomes of a minimally invasive, lateral, transpsoas approach for anterior lumbar interbody fusion in the treatment of adult degenerative scoliosis. Eur spine J. 2014;23(6):1215-1223.[22] Castro C, Oliveira L, Amaral R, et al. Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis? Clin Orthop Relat Res. 2014;472(6):1776-1783.[23] Caputo AM, Michael KW, Chapman TM, et al. Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. J Clin Neurosci. 2013;20(11):1558-1563.[24] Caputo AM, Michael KW, Chapman TM Jr., et al. Clinical outcomes of extreme lateral interbody fusion in the treatment of adult degenerative scoliosis. ScientificWorldJournal. 2012;2012:680643.[25] Wang MY, Mummaneni PV. Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus. 2010;28(3):E9.[26] Tormenti MJ, Maserati MB, Bonfield CM, et al. Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus. 2010;28(3):E7.[27] Isaacs RE, Hyde J, Goodrich JA, et al. A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976). 2010;35(26 Suppl):S322-S330.[28] Dakwar E, Cardona RF, Smith DA, et al. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. 2010;28(3):E8.[29] Anand N, Rosemann R, Khalsa B, et al. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 2010;28(3):E6.[30] McAfee PC, Shucosky E, Chotikul L, et al. Multilevel extreme lateral interbody fusion (XLIF) and osteotomies for 3-dimensional severe deformity: 25 consecutive cases. Int J Spine Surg. 2013;7:e8-e19.[31] Hu SS. Blood loss in adult spinal surgery. Eur spine J. 2004;13 Suppl 1:S3-S5.[32] Le TV, Baaj AA, Dakwar E, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012; 37(14):1268-1273.[33] Schwab F, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35(25):2224-2231.[34] Saigal R, Mundis GM Jr., Eastlack R, et al. Anterior column realignment (acr) in adult sagittal deformity correction: technique and review of the literature. Spine (Phila Pa 1976). 2016;41 Suppl 8: S66-S73.[35] Haque RM, Mundis GM Jr., Ahmed Y, et al. Comparison of radiographic results after minimally invasive, hybrid, and open surgery for adult spinal deformity: a multicenter study of 184 patients. Neurosurg Focus. 2014;36(5):E13.[36] Leven D, Cho SK. Pseudarthrosis of the cervical spine: risk factors, diagnosis and management. Asian Spine J. 2016;10(4):776-786.[37] Raizman NM, O'Brien JR, Poehling-Monaghan KL, et al. Pseudarthrosis of the spine. J Am Acad Orthop Surg. 2009;17(8): 494-503.[38] Waddell B, Briski D, Qadir R, et al. Lateral lumbar interbody fusion for the correction of spondylolisthesis and adult degenerative scoliosis in high-risk patients: early radiographic results and complications. Ochsner J. 2014;14(1):23-31.[39] Benglis DM, Vanni S, Levi AD. An anatomical study of the lumbosacral plexus as related to the minimally invasive transpsoas approach to the lumbar spine. J Neurosurg Spine. 2009;10(2):139-144.[40] Lykissas MG, Aichmair A, Hughes AP, et al. Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J. 2014;14(5):749-758.[41] Pumberger M, Hughes AP, Huang RR, et al. Neurologic deficit following lateral lumbar interbody fusion. Eur spine J. 2012;21(6): 1192-1199. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Yu Chengxiang, Liu Lehong, Li Wenbo, Chen Jinshi, Ran Chunlei, Wang Zhongping. Correlation between spine-pelvic sagittal parameters and prognosis of vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1412-1417. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [5] | Liu Yuhang, Zhou Jianqiang, Xu Xuebin, Qu Xingyue, Li Ziyu, Li Kun, Wang Xing, Li Zhijun, Li Xiaohe, Zhang Shaojie. Establishment and validation of finite element model of lower cervical spine in 6-year-old children [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 870-874. |
| [6] | Li Yuqiao, Sun Tianwei, Ma Bin, Zhou Zhaohong, Dong Runbei, Wu Haiyang. A comparative study of imaging parameters and quality of life scores between subtypes of lumbar spondylolisthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 943-948. |
| [7] | Li Jian, Bao Zhengqi, Zhou Pinghui, Zhu Ruizhi, Li Zhixiang, Wang Jinzi. Effects of posterior single open-door laminoplasty and anterior cervical corpectomy fusion on cervical sagittal balance parameters in the treatment of multilevel cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 949-953. |
| [8] | Yi Xinrong, Jia Fuquan, He Xin, Zhang Shaojie, Ren Xiaoyan, Li Zhijun. Establishment of cervical bone age equation for male adolescents aged 8-16 years old in Hohhot based on thin-slice CT [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 954-958. |
| [9] | Liu Yiyi, Qiu Junqiang, Yi Longyan, Zhou Cailiang. Effect of resistance training on interleukin-6 and C-reactive protein in middle-age and elderly people: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(5): 804-812. |
| [10] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [11] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [12] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [13] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [14] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [15] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||