Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (22): 3555-3560.doi: 10.3969/j.issn.2095-4344.2017.22.019
Previous Articles Next Articles
Aspirin effects on MG-63 cell proliferation on different modified titanium surfaces under fluid shear stress
- 1Stomatological Hospital, Southern Medical University, Guangzhou 510260, Guangdong Province, China; 2Guangdong Xieda Stomatological Hospital, Guangzhou 510399, Guangdong Province, China
-
Received:2017-06-19Online:2017-08-08Published:2017-09-01 -
Contact:Yang Xiao-yu, M.D., Chief physician, Master’s supervisor, Stomatological Hospital, Southern Medical University, Guangzhou 510260, Guangdong Province, China -
About author:Liang Zhong-lang, Master, Stomatological Hospital, Southern Medical University, Guangzhou 510260, Guangdong Province, China -
Supported by:the National Natural Science Foundation of China, No. 30500569
CLC Number:
Cite this article
Liang Zhong-lang, Liu Chang-hong, Li Shi-yi, Yang Xiao-yu.
share this article
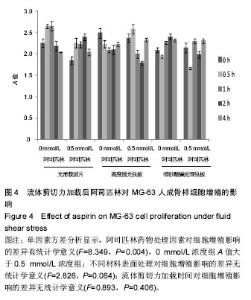
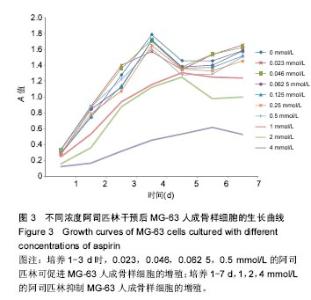
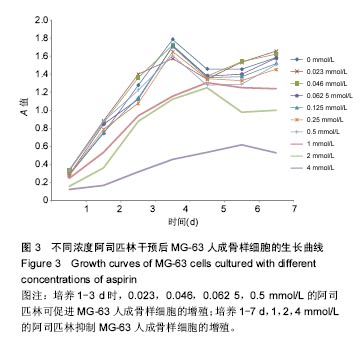
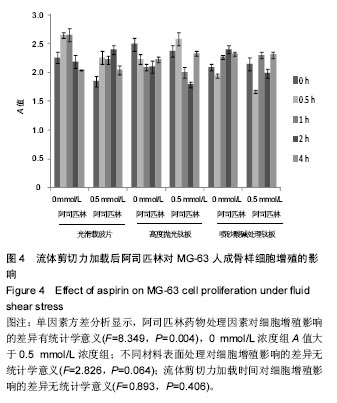
从不同浓度阿司匹林药物因素分析,所有适宜浓度组(0.023,0.046,0.062 5,0.125,0.25,0.5 mmol/L)与 0 mmol/L浓度组比较差异均无显著性意义;中高浓度、高于治疗剂量浓度组(1,2,4 mmol/L)与0 mmol/L浓度组比较差异均有显著性意义(P < 0.004)。其中细胞A值的均数由高到低排列为:0.023,0.046,0,0.062 5,0.125,0.25,0.5,1,2,4 mmol/L。 在培养第1天,0.023,0.046,0.5 mmol/L浓度组细胞A值高于0 mmol/L浓度组(P=0.006,P=0.025,P=0.016);在培养第2天,0.023,0.046,0.0625,0.5 mmol/L阿司匹林细胞A值高于0 mmol/L浓度组(P=0.002,P=0.006,P=0.019,P=0.002);培养第3天后,适宜浓度阿司匹林A值与0 mmol/L浓度组比较差异无显著性意义,提示在作用早期,0.023,0.046,0.062 5,0.5 mmol/L的阿司匹林可促进MG-63人成骨样细胞的增殖。根据药物梯度筛查的原则,实验选取了适宜浓度的最大值0.5 mmol/L阿司匹林来进行流体力学实验。 2.3 流体剪切力作用下阿司匹林对细胞增殖能力影响的检测 见图4。 析因设计的方差分析显示,阿司匹林药物处理因素与材料表面处理间不存在交互效应(F=2.193,P=0.115)。所以阿司匹林药物处理因素和材料表面处理因素对细胞增殖的影响各自改用单因素方差分析。阿司匹林药物处理因素对细胞增殖影响的差异有统计学意义(F=8.349,P=0.004),0 mmol/L浓度组A值大于0.5 mmol/L浓度组(2.260±0.244,2.148±0.276),提示在流体剪切力作用下,0.5 mmol/L阿司匹林可降低细胞的增殖活性。 从材料表面处理因素分析,不同材料表面处理对细胞增殖影响的差异无统计学意义(2.252±0.273,2.219± 0.273,2.140±0.244,F=2.826,P=0.064)。 从流体剪切力加载时间因素分析,加载时间对细胞增殖影响的差异无统计学意义(2.198±0.246,2.220±0.377,2.254±0.245,2.139±0.245,2.208±0.179,F=0.893,P=0.406)。 2.4 流体剪切力作用下0.5 mmol/L阿司匹林对不同材料表面细胞增殖的影响 在0.5 mmol/L阿司匹林干预下,不同材料对细胞增殖影响的差异无统计学意义(2.150±0.222,2.214±0.321,2.080±0.270,F=1.803,P=0.171)。在光滑载玻片上,0 mmol/L阿司匹林组的细胞A值高于0.5 mmol/L阿司匹林组(2.355±0.284,2.150±0.222,F=9.712,P=0.003)。在高度抛光和喷砂酸碱处理钛板上,0,0.5 mmol/L阿司匹林组的细胞A值比较差异无显著性意义(2.224±0.220,2.214±0.321,F=0.019,P=0.891;2.202±0.201,2.080±0.270,F=3.962,P=0.051)。 "
| [1]Cooper LF.A role for surface topography in creating and maintaining bone at titanium endosseous implants.J Prosthet Dent.2000;84(5):522-534.[2]Soboyejo WO,Nemetski B,Allameh S,et al.Interactions between MC3T3-E1 cells and textured Ti6Al4V surfaces.J Biomed Mater Res.2002;62(1):56-72.[3]Buser D,Schenk RK,Steinemann S,et al.Influence of surface characteristics on bone integration of titanium implants. A histomorphometric study in miniature pigs.J Biomed Mater Res. 1991;25(7):889-902.[4]Anselme K,Bigerelle M.Statistical demonstration of the relative effect of surface chemistry and roughness on human osteoblast short-term adhesion.J Mater Sci Mater Med.2006; 17(5):471-479.[5]Martin JY,Schwartz Z,Hummert TW,et al.Effect of titanium surface roughness on proliferation, differentiation, and protein synthesis of human osteoblast-like cells (MG63.J Biomed Mater Res.1995;29(3):389-401.[6]Mamalis AA,Markopoulou C,Vrotsos I,et al.Chemical modification of an implant surface increases osteogenesis and simultaneously reduces osteoclastogenesis: an in vitro study.Clin Oral Implants Res. 2011;22(6):619-626.[7]宿玉成,耿威,戈怡,等.现代口腔种植学[Z].200464.[8]雷欣,李世轶,钟凡,等. 流体剪切力和表面处理对钛表面成骨细胞增殖的影响[J].广东牙病防治, 2015,23(6):285-288.[9]钟汉铭,杨晓喻,刘长虹,等.流体剪切力作用下喷砂酸碱处理钛表面对原代成骨细胞Wnt/β-catenin信号通路关键蛋白mRNA表达的影响[J].广东牙病防治,2013,21(5):229-233.[10]Hasturk H,Kantarci A,Ohira T,et al.RvE1 protects from local inflammation and osteoclast- mediated bone destruction in periodontitis.FASEB J.2006;20(2):401-403.[11]周磊,岳新新.All-on-Four技术在口腔种植领域中的应用进展[J].口腔疾病防治,2017,25(1):1-7.[12]Fu JH,Bashutski JD,Al-Hezaimi K,et al.Statins, glucocorticoids, and nonsteroidal anti-inflammatory drugs: their influence on implant healing.Implant Dent.2012;21(5): 362-367.[13]De Luna-Bertos E,Ramos-Torrecillas J,Garcia-Martinez O,et al.Effect of aspirin on cell growth of human MG-63 osteosarcoma line.ScientificWorldJournal.2012;2012:834246.[14]Trancik T,Mills W,Vinson N.The effect of indomethacin, aspirin, and ibuprofen on bone ingrowth into a porous-coated implant.Clin Orthop Relat Res.1989;(249):113-121.[15]Carbone LD,Tylavsky FA,Cauley JA,et al.Association between bone mineral density and the use of nonsteroidal anti-inflammatory drugs and aspirin: impact of cyclooxygenase selectivity.J Bone Miner Res.2003;18(10): 1795-1802.[16]牛二龙.小剂量阿司匹林对去势大鼠骨髓基质干细胞成骨分化的影响[D].第四军医大学,2013.[17]Hochmuth RM,Mohandas N,Blackshear PJ.Measurement of the elastic modulus for red cell membrane using a fluid mechanical technique.Biophys J.1973;13(8):747-762.[18]Apostu D,Lucaciu O,Lucaciu GD,et al.Systemic drugs that influence titanium implant osseointegration.Drug Metab Rev.2017;49(1):92-104.[19]Vane JR.Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231(25):232-235.[20]Abate A,Yang G,Dennery PA,et al.Synergistic inhibition of cyclooxygenase-2 expression by vitamin E and aspirin.Free Radic Biol Med.2000;29(11):1135-1142.[21]Muller M,Raabe O,Addicks K,et al.Effects of non-steroidal anti-inflammatory drugs on proliferation, differentiation and migration in equine mesenchymal stem cells.Cell Biol Int. 2011;35(3):235-248.[22]Buckley MM,Brogden RN.Ketorolac. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential.Drugs.1990;39(1):86-109.[23]Chang JK,Li CJ,Liao HJ,et al.Anti-inflammatory drugs suppress proliferation and induce apoptosis through altering expressions of cell cycle regulators and pro-apoptotic factors in cultured human osteoblasts.Toxicology. 2009;258(2-3): 148-156.[24]Arikawa T,Omura K,Morita I.Regulation of bone morphogenetic protein-2 expression by endogenous prostaglandin E2 in human mesenchymal stem cells.J Cell Physiol.2004;200(3):400-406.[25]Chen ZW,Wu ZX,Sang HX,et al.Effect of aspirin administration for the treatment of osteoporosis in ovariectomized rat model.Zhonghua Yi Xue Za Zhi.2011; 91(13):925-929.[26]Yamaza T,Miura Y,Bi Y,et al.Pharmacologic stem cell based intervention as a new approach to osteoporosis treatment in rodents.PLoS One.2008;3(7):e2615.[27]王昌超,成业东,黄亚东,等.不同浓度阿司匹林对成骨细胞增殖的影响[J].山东医药,2015,55(44):28-29.[28]Guo Y,Zhang CY,Tian Y,et al.Effect of cyclooxygenase-2 on bone loss in ovariectomized rats. Zhonghua Fu Chan Ke Za Zhi.2012;47(6):458-462.[29]Li CJ,Chang JK,Wang GJ,et al.Constitutively expressed COX-2 in osteoblasts positively regulates Akt signal transduction via suppression of PTEN activity.Bone.2011; 48(2):286-297.[30]Fracon RN,Teofilo JM,Satin RB,et al.Prostaglandins and bone: potential risks and benefits related to the use of nonsteroidal anti-inflammatory drugs in clinical dentistry.J Oral Sci.2008; 50(3):247-252.[31]Urganus AL,Zhao YD,Pachman LM.Juvenile dermatomyositis calcifications selectively displayed markers of bone formation. Arthritis Rheum.2009;61(4):501-508.[32]Wei J,Wang J,Gong Y,et al.Effectiveness of combined salmon calcitonin and aspirin therapy for osteoporosis in ovariectomized rats.Mol Med Rep.2015;12(2):1717-1726.[33]刘显文,张超,刘曙光,等.骨保护素对去卵巢大鼠中种植体骨整合的影响[J].口腔疾病防治, 2016,24(11):634-639.[34]Ogata N,Chung UI,Tei Y,et al.Optimization of signaling pathways for bone regeneration.Clin Calcium. 2008;18(12): 1707-1712.[35]Chae YM,Heo SH,Kim JY,et al.Upregulation of smpd3 via BMP2 stimulation and Runx2.BMB Rep. 2009;42(2):86-90.[36]Krishnan V,Bryant HU,Macdougald OA.Regulation of bone mass by Wnt signaling.J Clin Invest. 2006;116(5):1202-1209.[37]钟汉铭.流体剪切力对不同钛表面成骨细胞Wnt/β-catenin信号通路关键成员表达的影响[D].南方医科大学,2013.[38]吴丹,丁寅,王琪.流体剪切力对大鼠成骨细胞增殖及细胞周期的影响[J].临床口腔医学杂志,2007,23(4):197-199.[39]Coleman ML,Marshall CJ,Olson MF.Ras promotes p21(Waf1/Cip1) protein stability via a cyclin D1-imposed block in proteasome-mediated degradation.EMBO J.2003;22(9): 2036-2046. |
| [1] | Wang Jianping, Zhang Xiaohui, Yu Jinwei, Wei Shaoliang, Zhang Xinmin, Xu Xingxin, Qu Haijun. Application of knee joint motion analysis in machanism based on three-dimensional image registration and coordinate transformation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(在线): 1-5. |
| [2] | Zhang Yufang, Lü Meng, Mei Zhao. Construction and verification of a full spine biomechanical model of adolescent scoliosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1351-1356. |
| [3] | Bai Zixing, Cao Xuhan, Sun Chengyi, Yang Yanjun, Chen Si, Wen Jianmin, Lin Xinxiao, Sun Weidong. Construction and biomechanical analysis of ankle joint finite element model in gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1362-1366. |
| [4] | Liu Feng, Feng Yi. Finite element analysis of different Kirschner wire tension bands on transverse patella fractures during gait cycle [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1367-1371. |
| [5] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [6] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [7] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [8] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [9] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [10] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [11] | Duan Chao, Shang Xiaoqiang, Duan Xianglin, Yang Ping, Tao Shengxiang. Stability of patellar claw versus loop plate combined with patellar claw for the treatment of comminuted fractures of the lower pole of the patella [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 934-937. |
| [12] | Wen Mingtao, Liang Xuezhen, Li Jiacheng, Xu Bo, Li Gang. Mechanical stability of Sanders II type calcaneal fractures fixed by two internal fixation methods [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 838-842. |
| [13] | Huang Hao, Hong Song, Wa Qingde. Finite element analysis of the effect of femoral component rotation on patellofemoral joint contact pressure in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 848-852. |
| [14] | Zheng Yongze, Zheng Liqin, He Xingpeng, Chen Xinmin, Li Musheng, Li Pengfei, Lin Ziling. Extended finite element modeling analysis of femoral neck fracture based on ABAQUS software [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 853-857. |
| [15] | Liu Yuhang, Zhou Jianqiang, Xu Xuebin, Qu Xingyue, Li Ziyu, Li Kun, Wang Xing, Li Zhijun, Li Xiaohe, Zhang Shaojie. Establishment and validation of finite element model of lower cervical spine in 6-year-old children [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(6): 870-874. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||