Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (18): 2890-2899.doi: 10.3969/j.issn.2095-4344.2017.18.017
Previous Articles Next Articles
Fresh amniotic membrane for repair of acute peripheral nerve injury
- Third Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China
-
Received:2017-01-16Online:2017-06-28Published:2017-07-07 -
Contact:Tian De-hu, M.D., Chief physician, Professor, Third Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China -
About author:Ma Tao, Master, Third Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China -
Supported by:the Natural Science Foundation of Hebei Province, No. ZL20140066
CLC Number:
Cite this article
Ma Tao, Kou Wen-guan, Liu Guo-li, Bai Jiang-bo, Yu Kun-lun, Tian De-hu. Fresh amniotic membrane for repair of acute peripheral nerve injury[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(18): 2890-2899.
share this article

2.1 实验动物数量分析 SD大鼠60只,随机分为3组,每组20只。最终人羊膜组19只、生物膜组18只、空白对照组19只进入结果分析,因死亡脱落3只,逃跑1只。 2.2 大体观察结果 见图1。①3组大鼠手术切口均未出现感染,7 d切口拆线,切口一级愈合;②3组大鼠术后2周大部分出现手术侧下肢稍肿胀且跛行,精神状态差,进食减少。2周后肿胀、精神状态及饮食逐渐恢复,人羊膜组、生物膜组大鼠跛行时间较空白对照组短,活动量恢复更早;③人羊膜组、生物膜组与空白对照组相比足底和足趾皮肤溃疡大鼠数量少且溃疡恢复时间短;④术后2周,羊膜、生物膜局部稍有吸收,4周大部吸收,8,12周完全吸收;⑤人羊膜组、生物膜组神经和周围组织粘连较轻且粘连较疏松,活动度可,空白对照组神经和周围组织粘连广泛、紧密,不易分离。"

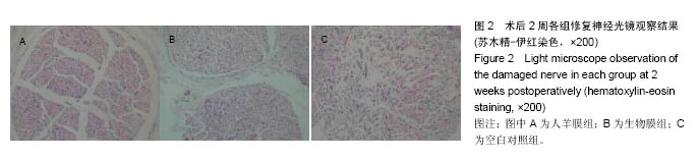
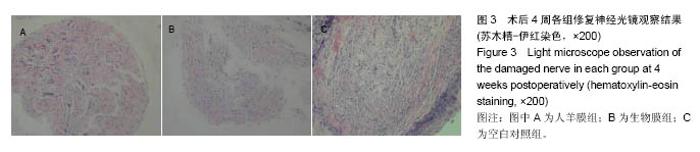
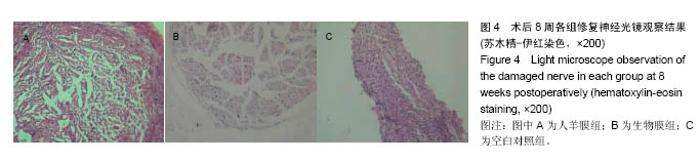
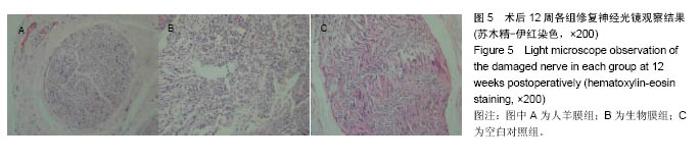
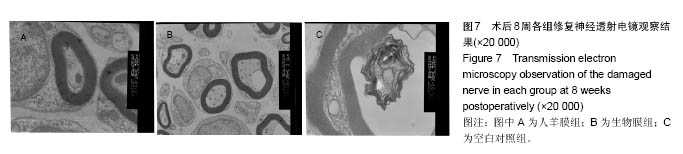
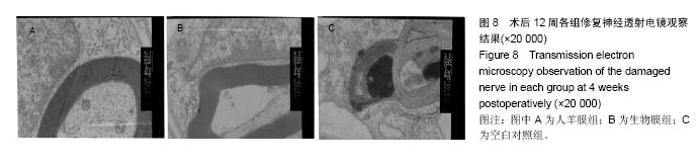
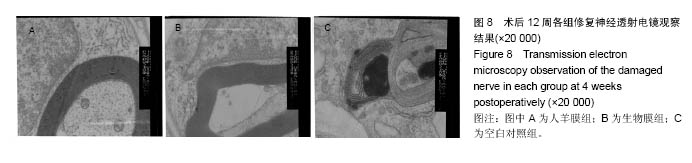
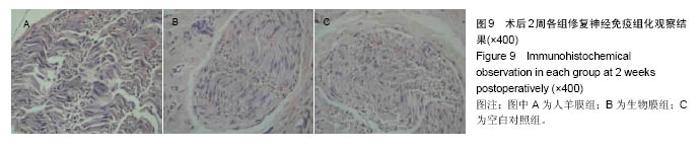
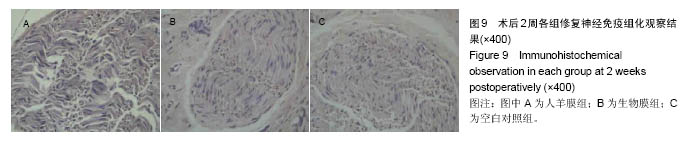
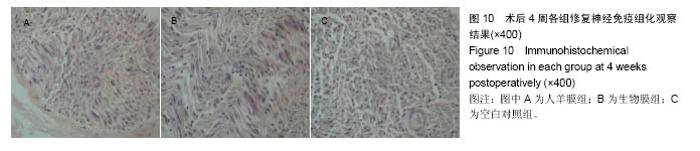
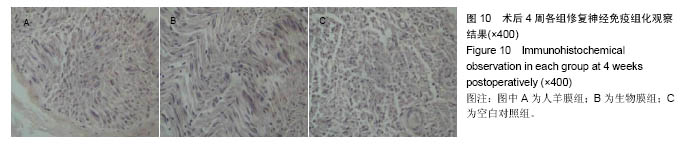
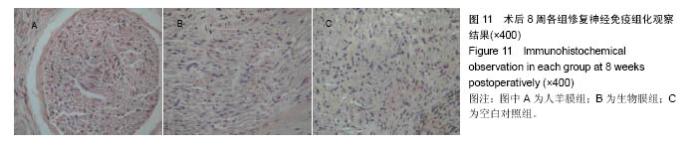
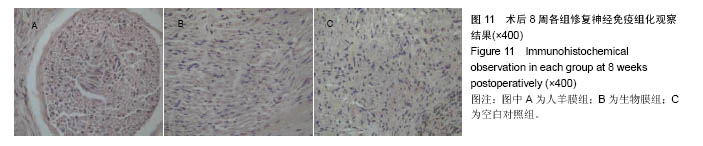
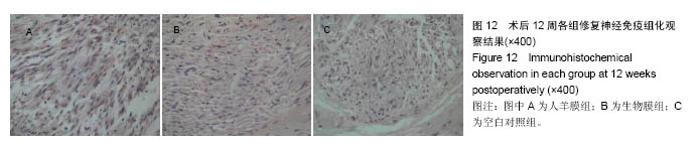
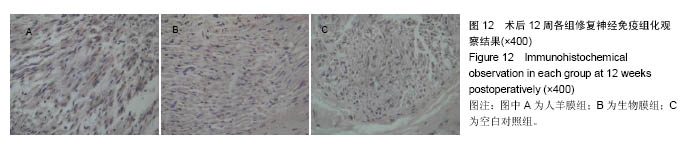
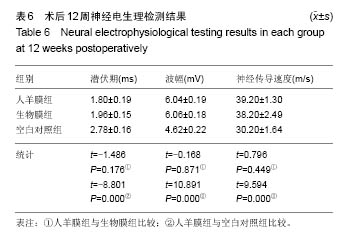
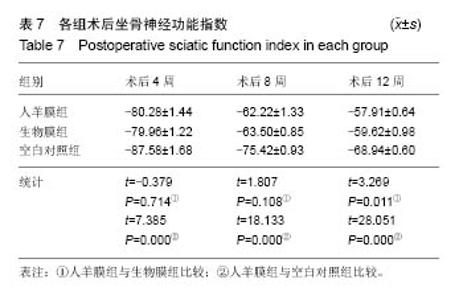
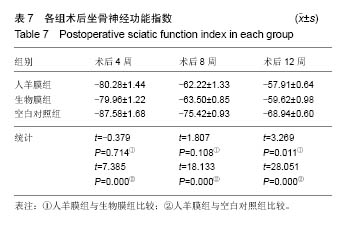
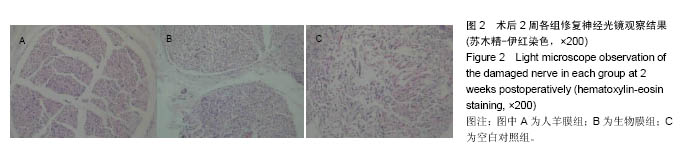
2.3 光镜观察结果 见图2-5。 术后2周:人羊膜组、生物膜组吻合口周围炎性细胞明显增多,许旺细胞增生,且排列紊乱,大量纤维组织增生。空白对照组吻合口周围大量炎性细胞浸润,纤维组织增生明显,吻合口周围杂乱无章。 术后4周:人羊膜组、生物膜组许旺细胞数量较前有所增加,并且形成了细胞索,炎性细胞较前有所减少,有部分神经轴突生长。空白对照组有许旺细胞增生,炎性细胞较前减少,但神经再生较少,并且有少量髓鞘碎片存在。 术后8周:3组中髓鞘碎片消失,再生神经纤维增多。人羊膜组、生物膜组炎性细胞基本消失,许旺细胞排列较规律,神经纤维较粗。空白对照组仍存在少量炎性细胞,许旺细胞排列较规律,但神经纤维较人羊膜组、生物膜组细。 术后12周:3组炎性细胞均基本消失,人羊膜组、生物膜组比空白对照组神经纤维密集且髓鞘厚度更厚。"
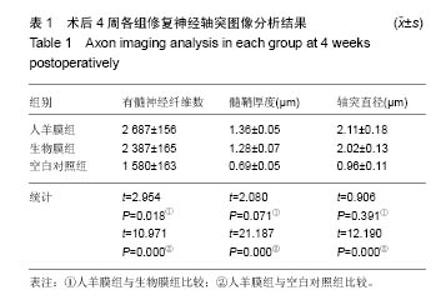
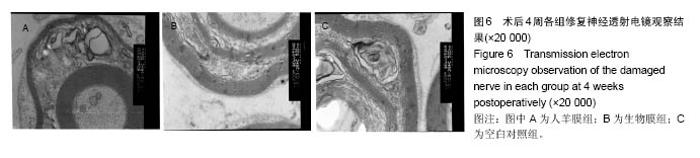
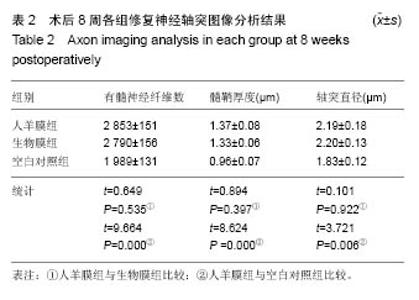
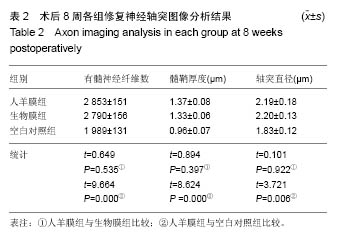
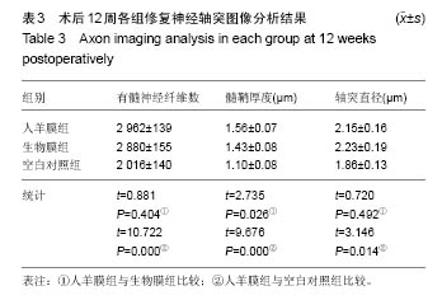
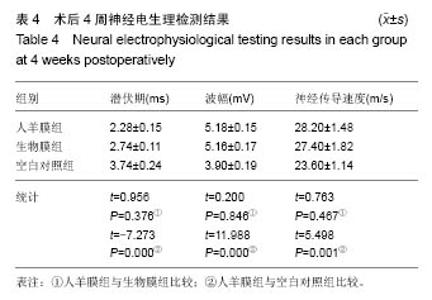
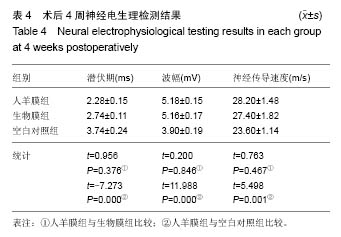
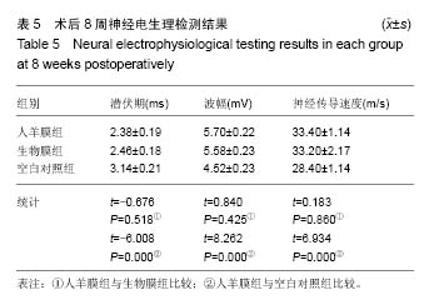
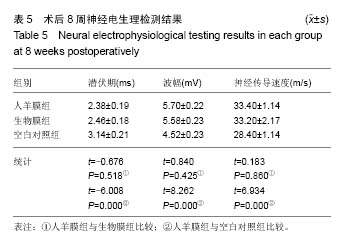
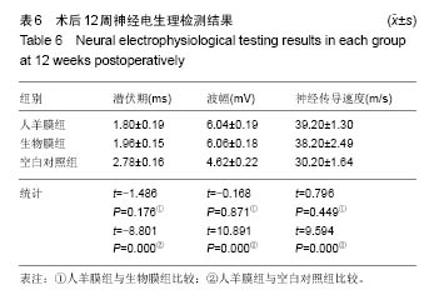
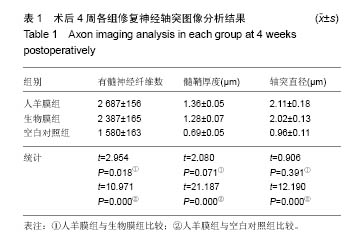
2.6 轴突图像分析 见表1-3。 术后4周:3组再生神经远段横截面有髓神经纤维数目较少,髓鞘厚度较薄,结构不成熟。人羊膜组、生物膜组吻合口远端横截面再生的有髓神经纤维数目、平均直径及髓鞘厚度均优于空白对照组,人羊膜组与空白对照组比较差异有显著性意义(P < 0.05),人羊膜组与生物膜组相比差异无显著性意义(P > 0.05)。 术后8,12周:3组吻合口远端横截面再生的有髓神经纤维数目、平均直径及髓鞘厚度均有所增加。人羊膜组、生物膜组吻合口远端横截面再生的有髓神经纤维数目、平均直径及髓鞘厚度均优于空白对照组,人羊膜组与空白对照组比较差异有显著性意义(P < 0.05),人羊膜组与生物膜组相比差异无显著性意义(P > 0.05)。"
| [1]Cajal RY, DeFelipe J, Jones EG. Regeneration and regeneration of the nervous system (translated by May RM). New York, Oxford: Oxford University Press,1991.[2]Millesi H. Brachial plexus injuries. Nerve grafting. Clin Orthop Relat Res. 1988;(237):36-42. [3]Rühmann O, Schmolke S, Bohnsack M, et al. Reconstructive operations for the upper limb after brachial plexus palsy. Am J Orthop (Belle Mead NJ). 2004;33(7):351-362.[4]张泽华,阮怀珍.基因治疗在周围神经损伤修复中的应用[J].创伤外科杂志,2002,4(6):377-380.[5]Verdú E, Ceballos D, Vilches JJ, et al. Influence of aging on peripheral nerve function and regeneration. J Peripher Nerv Syst. 2000;5(4):191-208.[6]Stoll G, Jung S, Jander S, et al. Tumor necrosis factor-alpha in immune-mediated demyelination and Wallerian degeneration of the rat peripheral nervous system. J Neuroimmunol. 1993; 45(1-2):175-182.[7]Taskinen HS, Röyttä M. The dynamics of macrophage recruitment after nerve transection. Acta Neuropathol. 1997; 93(3):252-259. [8]Perry VH, Brown MC, Gordon S. The macrophage response to central and peripheral nerve injury. A possible role for macrophages in regeneration. J Exp Med. 1987;165(4):1218-1223.[9]Beuche W, Friede RL. The role of non-resident cells in Wallerian degeneration. J Neurocytol. 1984;13(5):767-796.[10]Griffin JW, George R, Lobato C, et al. Macrophage responses and myelin clearance during Wallerian degeneration: relevance to immune-mediated demyelination. J Neuroimmunol. 1992;40(2-3):153-165.[11]Sunderland S. Nerve and nerve injury.New York: Churchill Livingston,1987:173-176.[12]Lundborg G, Dahlin LB, Danielsen N, et al. Nerve regeneration in silicone chambers: influence of gap length and of distal stump components. Exp Neurol. 1982;76(2):361-375.[13]Danforth D, Hull RW. The microscopic anatomy of the fetal membranes with particular reference to the detailed structure of the amnion. Am J Obstet Gynecol. 1958;75(3):536-550.[14]Bourne GL. The microscopic anatomy of the human amnion and chorion. Am J Obstet Gynecol. 1960;79:1070-1073.[15]Miki T, Strom SC. Amnion-derived pluripotent/multipotent stem cells. Stem Cell Rev. 2006;2(2):133-142.[16]Dluzen DE, McDermott JL, Anderson LI, et al. Age-related changes in nigrostriatal dopaminergic function are accentuated in +/- brain-derived neurotrophic factor mice. Neuroscience. 2004;128(1):201-208.[17]Akle CA, Adinolfi M, Welsh KI, et al. Immunogenicity of human amniotic epithelial cells after transplantation into volunteers. Lancet. 1981;2(8254):1003-1005.[18]Adinolfi M, Akle CA, McColl I, et al. Expression of HLA antigens, beta 2-microglobulin and enzymes by human amniotic epithelial cells. Nature. 1982;295(5847):325-327.[19]Sakuragawa N, Enosawa S, Ishii T, et al. Human amniotic epithelial cells are promising transgene carriers for allogeneic cell transplantation into liver. J Hum Genet. 2000;45(3): 171-176.[20]Houlihan JM, Biro PA, Harper HM, et al. The human amnion is a site of MHC class Ib expression: evidence for the expression of HLA-E and HLA-G. J Immunol. 1995;154(11): 5665-5674.[21]Hunt JS, Wood GW. Interferon-gamma induces class I HLA and beta 2-microglobulin expression by human amnion cells. J Immunol. 1986;136(2):364-367.[22]李沫.预防大鼠坐骨神经修复中瘢痕黏连及促进神经再生的作用研究[D].西安:第四军医大学,2012.[23]Dahlin LB, Lundborg G. Use of tubes in peripheral nerve repair. Neurosurg Clin N Am. 2001;12(2):341-352.[24]Johnson EO, Soucacos PN. Nerve repair: experimental and clinical evaluation of biodegradable artificial nerve guides. Injury. 2008;39 Suppl 3:S30-36.[25]宋永周,郭威,崔慧先,等.人羊膜在神经组织工程中的应用进展[J].生物医学工程研究,2007,26(4):375-378.[26]詹球,王磊,童亚林,等.京尼平交联冻存人羊膜对大鼠损伤神经修复及预防粘连的作用[J].华南国防医学杂志,2013,27(4): 234-237.[27]范伟杰,杨志明,邓力,等.羊膜的基础和临床应用研究进展[J].中国修复重建外科杂志,2006,20(1):65-68.[28]Kamiya K, Wang M, Uchida S, et al. Topical application of culture supernatant from human amniotic epithelial cells suppresses inflammatory reactions in cornea. Exp Eye Res. 2005;80(5):671-679.[29]Solomon A, Rosenblatt M, Monroy D, et al. Suppression of interleukin 1alpha and interleukin 1beta in human limbal epithelial cells cultured on the amniotic membrane stromal matrix. Br J Ophthalmol. 2001;85(4):444-449.[30]刘礼.金异体生物羊膜修复周围神经损伤的实验研究[D]. 南昌:南昌大学,2010.[31]张殿英,姜保国,傅忠国,等.周围神经损伤后 S-100 蛋白的分布和变化研究[J].中国矫形外科杂志,2002,9(4):348-351. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | Kong Yamin, Yan Juntao, Ma Bingxiang, Li Huawei. Massage vibration intervenes with MyoD expression and proliferation and differentiation of muscle satellite cells in rats with sciatic nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1160-1166. |
| [3] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [4] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [5] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [6] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [7] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [8] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [9] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [10] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [11] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [12] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [13] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [14] | Sun Xinzheng, Chen Xiaoke, Wang Chenghao, He Hui. Exercise improves pain induced by sciatic nerve injury in animal models: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 321-328. |
| [15] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||