Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (49): 7341-7348.doi: 10.3969/j.issn.2095-4344.2016.49.007
Previous Articles Next Articles
Establishment and evaluation of the animal model of acute spinal cord injury
Wu Yang-peng, Fan Xiao, Zhang Li
- Key Laboratory of Ministry of Education of the People’s Republic of China, School of Orthopaedics and Traumatology of TCM, Fujian University of Traditional Chinese Medicine, Fuzhou 350122, Fujian Province, China
-
Received:2016-09-06Online:2016-11-30Published:2016-11-30 -
Contact:Zhang Li, M.D., Professor, Doctoral supervisor, Key Laboratory of Ministry of Education of the People’s Republic of China, School of Orthopaedics and Traumatology of TCM, Fujian University of Traditional Chinese Medicine, Fuzhou 350122, Fujian Province, China -
About author:Wu Yang-peng, Studying for master’s degree, Key Laboratory of Ministry of Education of the People’s Republic of China, School of Orthopaedics and Traumatology of TCM, Fujian University of Traditional Chinese Medicine, Fuzhou 350122, Fujian Province, China -
Supported by:the National Natural Science Foundation of China, No. 81273775; the Millions Talents Engineering of Fujian Province, No. 2014[4]
CLC Number:
Cite this article
Wu Yang-peng, Fan Xiao, Zhang Li. Establishment and evaluation of the animal model of acute spinal cord injury[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(49): 7341-7348.
share this article
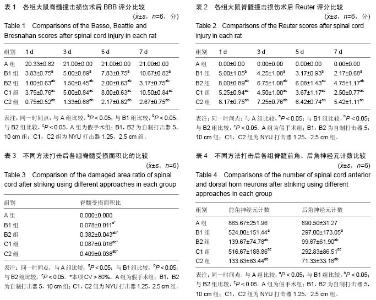
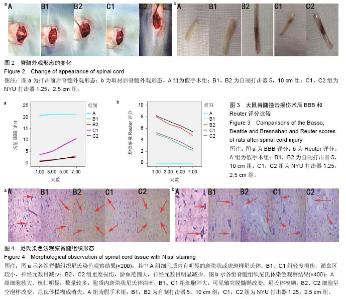
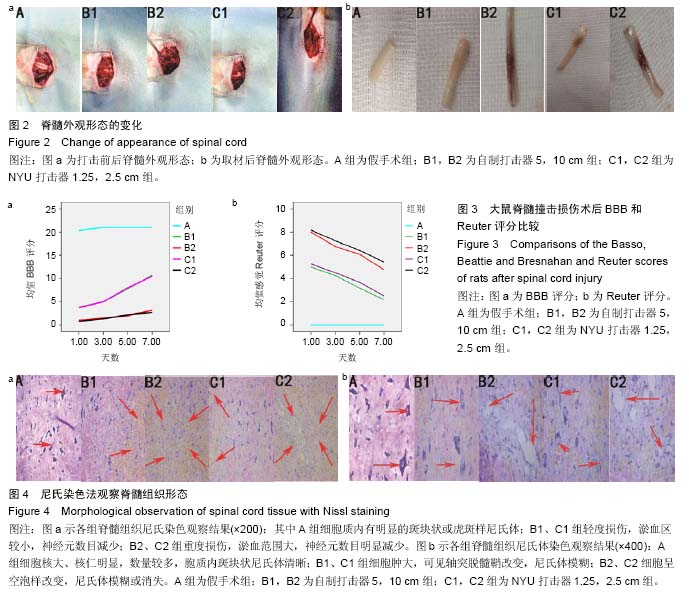
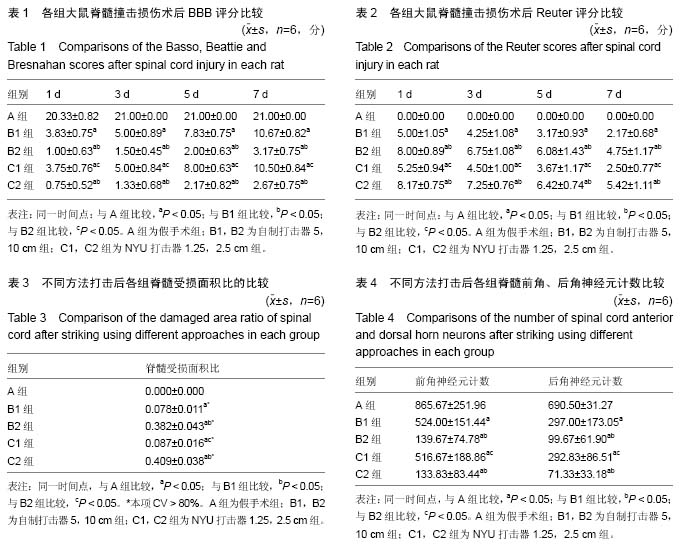
2.1 实验动物数量分析 选用30只雌性SD大鼠,随机分为5组,在实验过程中,由于麻醉剂量过大和术后感染导致2只大鼠死亡,死亡后立即选2只体质量接近的大鼠按原来造模方法造模后补上。 2.2 模型稳定性 脊髓损伤模型研究众多,包括脊髓撞击损伤模型、脊髓缺血损伤模型、脊髓压迫损伤模型等等,然而临床中由于车祸撞击或地震等重物撞击脊柱造成的脊髓损伤更为多见,故经典的Allen’s重物坠落法建立的脊髓损伤模型,其临床相似性高。而本实验基于经典Allen’s法的基本原理进行改良,模型更接近临床,并与稳定性高的NYU打击模型进行比较,来证实本实验模型的稳定性,结果可靠,可控制好,操作简便,易于复制。 2.3 两种打击器制备的脊髓损伤模型脊髓外观形态 造模时,正常脊髓节段呈乳白色透亮条索状,后正中沟明显,且伴有血管走行,打击后,硬脊膜完整,硬脊膜下出现不同程度水肿、淤血(见图2a);脊髓损伤术后1周,损伤局部组织间有不同程度的粘连,不同打击器及不同打击高度损伤后,受损脊髓段出现不同程度的淤血,但硬脊膜均保持完整,B2、C2组淤血明显(见图2b)。 2.4 急性脊髓损伤动物模型的评估 2.4.1 术后常见症状 ①死亡:A组1只,因麻醉剂量过大,麻醉后死亡,又随机抽取1只体质量相近的正常雌鼠补上;B2组1只,术后见双下肢浮肿、血尿明显,并有自噬足指、眼睛红色变淡、体质量明显减轻等表现,于术后5 d出现死亡,可能与术后泌尿系统感染、贫血有关;②无尿便:B2、C2组损伤较重,大部分术后3 d均无尿便,需行人工按摩促排便;③血尿:A组及大部分B1、C1轻度损伤的大鼠均无血尿,而B2、C2组损伤较重者,部分出现不同程度的血尿,经抗生素治疗及加强术后护理后,基本恢复;④伤口渗血:C2组出现一只伤口少量渗血,经碘伏消毒纱布包扎后,第2天未见渗血。 2.4.2 行为学评分 BBB评分:A组术后1 d,部分大鼠运动功能未完全恢复,术后3 d全部恢复到21分;余各组均出现不同程度的运动功能障碍,其中B2、C2组术后1 d,大鼠后肢几乎全瘫,术后3-7 d均出现不同程度的功能恢复(见图3a),B1和C1、B2和C2同一时间点BBB评分比较,差异无显著性意义(P > 0.05),余各组组间BBB评分比较,差异有显著性意义(P < 0.05)(见表1),说明同一打击器,随着打击高度的增加,相应BBB评分则降低。 感觉评分:A组术后1 d,全部感觉功能正常;余各组均出现不同程度的感觉功能障碍,其中B2、C2组术后1 d肌力、肌张力、牵张发射消失,部分大鼠可见背部感觉部分存在,疼痛回收迟钝,而B1、C1组术后1d肌力消失,肌张力、牵张反射、疼痛回缩反射、背部感觉存在,术后3-7 d均出现不同程度的功能恢复(见图3b),B1和C1、B2和C2同一时间点感觉评分比较,差异无显著性意义(P > 0.05),余各组组间感觉评分比较,差异有显著性意义(P < 0.05),见表2。 2.4.3 组织学观察 尼氏染色后,A组见脊髓灰、白质分界清晰,呈蝴蝶状,神经元细胞核大、核仁明显、数量较多,神经细胞质内有明显的斑块状或虎斑样尼氏体;余各组在灰质中央或两侧均有不同程度的淤血灶,组织破坏明显(见图4a)。损伤处可见灰质神经元肿胀,细胞间质水肿,轴突有脱髓鞘改变,部分细胞呈空泡样改变,神经元数目明显减少,尼氏体模糊或消失(见图4b)。 2.4.4 不同方法打击后脊髓受损面积比 用Motic Med 6.0显微图像分析系统,选则手动分析法测得损伤处像素数与脊髓横截面总像素数,从而计算出受损面积比。A组未见明显受损区,比值为0;B1和B2、C1和C2组随打击的高度的增加而升高,组间差异有显著性意义(P < 0.05),B1和C1、B2和C2损伤面积比差异无显著性意义(P > 0.05),见表3。CV-B1=0.141,CV-B2=0.113, CV-C1=0.184,CV-C2=0.093,证明两种打击器每次打击的结果差异较小,稳定性较好。 2.4.5 不同方法打击后脊髓前、后角神经元计数 用Motic Med 6.0显微图像分析系统,运用免疫组化图像分析法对前、后角神经元阳性目标进行半定量分析;A组前、后角神经元数目最多,尼氏体明显;B1和B2、C1和C2组随打击的高度的增加而减少,组间差异有显著性意义 (P < 0.05),B1和C1、B2和C2损伤后前、后角神经元及尼氏体半定量分析差异无显著性意义(P > 0.05),见表4。"
| [1] Iwamoto S, Higashi A, Ueno T, et al. Protective effect of sivelestat sodium hydrate (ONO-5046) on ischemic spinal cord injury. Interact Cardiovasc Thorac Surg. 2009;8(6):606-609. [2] Etz CD, Homann TM, Luehr M, et al. Spinal cord blood flow and ischemic injury after experimental sacrifice of thoracic and abdominal segmental arteries. Eur J Cardiothorac Surg. 2008;33(6):1030-1038. [3] 金华,郭光琼,李江,等.脊髓缺血再灌注损伤模型的改进及对大鼠神经行为学的影响[J].中风与神经疾病杂志, 2012, 29(10):879-882. [4] Margolis JM, Juneau P, Sadosky A, et al.Health care resource utilization and medical costs of spinal cord injury with neuropathic pain in a commercially insured population in the United States. Arch Phys Med Rehabil. 2014;95(12): 2279-2287. [5] Varma AK, Das A, Wallace GT, et al.Spinal cord injury: a review of current therapy, future treatments, and basic science frontiers. Neurochem Res. 2013;38(5): 895-905. [6] Nagoshi N, Fehlings MG. Investigational drugs for the treatment of spinal cord injury: review of preclinical studies and evaluation of clinical trials from Phase I to II. Expert Opin Investig Drugs. 2015;24(5): 645-658. [7] Zhang SX, Huang F, Gates M, et al. Tail nerve electrical stimulation combined with scar ablation and neural transplantation promotes locomotor recovery in rats with chronically contused spinal cord. Brain Res. 2012;1456: 22-35. [8] Jones CF, Lee JH, Kwon BK, et al.Development of a large-animal model to measure dynamic cerebrospinal fluid pressure during spinal cord injury: Laboratory investigation. J Neurosurg Spine. 2012;16(6): 624-635. [9] 张俐,张纪浩,陈凯,等.活血通督汤对脊髓缺血再灌注损伤NF-κB、VCAM-1表达的作用[J].中华中医药杂志, 2015, 30(4):1020-1023. [10] Awad H, Ankeny DP, Guan Z, et al.A mouse model of ischemic spinal cord injury with delayed paralysis caused by aortic cross-clamping. Anesthesiology. 2010; 113(4): 880-891. [11] Su YF, Lin CL, Lee KS, et al.A modified compression model of spinal cord injury in rats: functional assessment and the expression of nitric oxide synthases. Spinal Cord. 2015;53(6): 432-435. [12] Nout YS, Ferguson AR, Strand SC, et al.Methods for functional assessment after C7 spinal cord hemisection in the rhesus monkey. Neurorehabil Neural Repair. 2012;6(6): 556-569. [13] Xue F, Wei Y, Chen Y, et al.A rat model for chronic spinal nerve root compression. Eur Spine J. 2014; 23(2): 435-446. [14] Zibly Z, Schlaff CD, Gordon I, et al.A novel rodent model of spinal metastasis and spinal cord compression. BMC Neurosci. 2012; 13: 137. [15] Svensson E, Schillberg B, Kling AM, et al.Reliability of the balanced inventory for spinal disorders, a questionnaire for evaluation of outcomes in patients with various spinal disorders. J Spinal Disord Tech. 2012;25(4): 196-204. [16] Seifert JL, Bell JE, Elmer BB, et al.Characterization of a novel bidirectional distraction spinal cord injury animal model. J Neurosci Methods. 2011;197(1): 97-103. [17] Kandhare AD, Shivakumar V, Rajmane A, et al. Evaluation of the neuroprotective effect of chrysin via modulation of endogenous biomarkers in a rat model of spinal cord injury. J Nat Med. 2014;68(3): 586-603. [18] Fehlings MG, Wilson JR, Frankowski RF, et al. Riluzole for the treatment of acute traumatic spinal cord injury: rationale for and design of the NACTN Phase I clinical trial. J Neurosurg Spine. 2012;17(1 Suppl): 151-156. [19] Li H, Roy Choudhury G, Zhang N, et al.Photothrombosis- induced Focal Ischemia as a Model of Spinal Cord Injury in Mice. J Vis Exp. 2015;(101): e53161. [20] Falowski S, Ooi YC, Sabesan A, et al.Spinal cord injury induced by a cervical spinal cord stimulator. Neuromodulation. 2011;14(1): 34-36; discussion 36-37. [21] Alilain WJ, Horn KP, Hu H, et al.Functional regeneration of respiratory pathways after spinal cord injury. Nature. 2011;475(7355): 196-200. [22] Rabchevsky AG, Patel SP, Duale H, et al.Gabapentin for spasticity and autonomic dysreflexia after severe spinal cord injury. Spinal Cord. 2011;49(1):99-105. [23] Zheng Y, Zhang YP, Shields LB, et al.Effect of heparin following cervical spinal cord injuries in rats. Neurosurgery. 2011;69(4): 930-941; discussion 941. [24] Gruner JA.A monitored contusion model of spinal cord injury in the rat. J Neurotrauma. 1992;9(2): 123-126; discussion 126-128. [25] Huan W, Wu X, Zhang S, et al.Spatiotemporal patterns and essential role of TNF receptor-associated factor 5 expression after rat spinal cord Injury. J Mol Histol. 2012;43(5): 527-533. [26] Rosas OR, Torrado AI, Santiago JM, et al.Long-term treatment with PP2 after spinal cord injury resulted in functional locomotor recovery and increased spared tissue. Neural Regen Res. 2014;9(24): 2164-2173. [27] Basso DM, Beattie MS, Bresnahan JC. A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma. 1995;12(1): 1-21. [28] 吕静.大鼠脊髓损伤模型的建立及行为学评分[D].中南大学,2011. [29] 李剑锋,冯世庆,夏润福,等.不同程度脊髓背侧压迫损伤模型大鼠脊髓损伤致伤器的设计[J].中国组织工程研究, 2015,19(18):2856-2861. [30] 黄霖,唐勇,杨睿,等.通用型脊髓打击器的研制与脊髓损伤动物模型的建立[J].中国脊柱脊髓杂志,2008,18(9):688-693. [31] 陈霄雷,林雷雷,邵璐斐,等.大鼠脊髓打击器研制及其制备的脊髓损伤模型稳定性评价[J]. 宁夏医科大学学报, 2014,36(7):716-719. [32] 陈德英,程赛宇,肖艳,等.坐骨神经损伤后相应脊髓前角运动神经元的形态学变化[J].中国临床康复,2002,6(10): 1424-1425. [33] 陈德英,程赛宇,肖燕,等. 神经元尼氏染色法在坐骨神经损伤研究中的应用[J]. 创伤外科杂志,2001,13(z1):35-37. [34] 王力,孙丽,窦慧慧,等. 大鼠新型挫伤型脊髓损伤模型的建立及评价[J]. 神经解剖学杂志,2010,26(6):638-642. [35] 熊春翔,宗少晖,曾高峰,等. 大鼠Allen’s脊髓损伤模型的建立及评价[J]. 广西医科大学学报,2011,28(2):215-217. [36] 蔡文琴,阮怀珍,黎海蒂.医用神经生物学基础[M].重庆:西南师范大学出版社,2001: 41. [37] 陈凯.活血通督汤对兔脊髓缺血再灌注损伤后肢运动功能及细胞凋亡的影响[D].福建中医药大学,2014. [38] 陈向华,张俐,王和鸣,等.丹参酮及电针对脊髓缺血再灌注损伤细胞因子IL-1β、IL-1Ra、IL-8的影响[J].中华中医药杂志,2012,27(4):987-991. [39] 张俐,林庆宾.丹参及丹参酮Ⅱ-A磺酸钠对脊髓缺血再灌注损伤IL-1β、ICAM-1及MPO表达的影响[J].中华中医药杂志,2012,27(8):2042-2047. [40] 张俐,安国尧,张文光,等.丹参酮-ⅡA磺酸钠对脊髓缺血再灌注损伤NF-κB、VCAM-1和血液流变性的影响[J].中国骨伤,2012,28(12):1016-1020. [41] 林庆宾,张俐.活血通督汤对脊髓缺血再灌注损伤神经细胞凋亡的影响[J]. 中国中医骨伤科杂志,2014,22(8):1-11. |
| [1] | Min Youjiang, Yao Haihua, Sun Jie, Zhou Xuan, Yu Hang, Sun Qianpu, Hong Ensi. Effect of “three-tong acupuncture” on brain function of patients with spinal cord injury based on magnetic resonance technology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-8. |
| [2] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [3] | Jiang Hongying, Zhu Liang, Yu Xi, Huang Jing, Xiang Xiaona, Lan Zhengyan, He Hongchen. Effect of platelet-rich plasma on pressure ulcers after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1149-1153. |
| [4] | Wan Ran, Shi Xu, Liu Jingsong, Wang Yansong. Research progress in the treatment of spinal cord injury with mesenchymal stem cell secretome [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1088-1095. |
| [5] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [6] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [7] | Ma Binxiang, He Wanqing, Zhou Guangchao, Guan Yonglin. Triptolide improves motor dysfunction in rats following spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 701-706. |
| [8] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [9] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [10] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [11] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [12] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [13] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [14] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [15] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||