| [1] Boutelier P.Complications of Laparoscopic Cholecystectomy:Evaluation Study.Bull Acad Natl Med.1998;18:617-626.
[2] 黄志强.医源性胆道损伤:老问题,新意义[J].中国实用外科杂志, 1999,19(8):451.
[3] Takatsuki M,Yanaga K,Okudaira S,et al.Duct-to-duct biliary reconstruction in adult-to-adult living donor liver transplantation. Clin Transplant.2002;16:345-349.
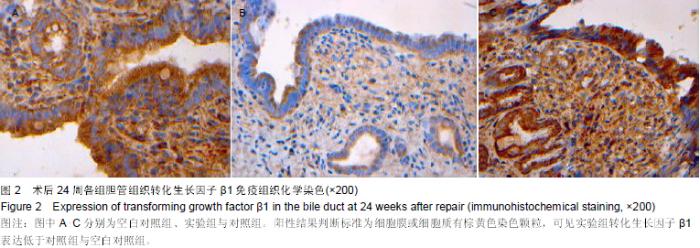
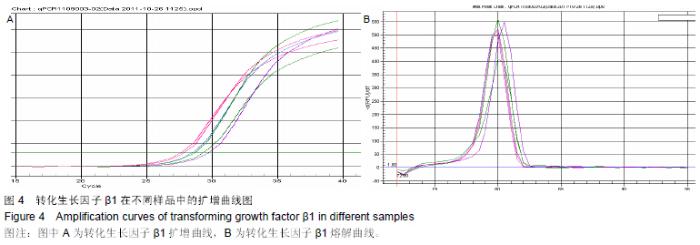
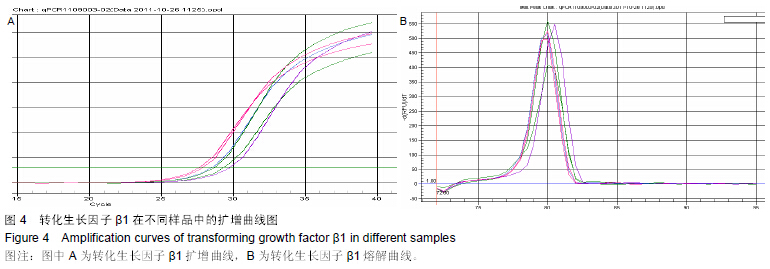
[4] 刘建明,马利林,施公胜.壁层腹膜修复胆管缺损模型组织中转化生长因子ß1的表达[J].南通医学院学报,2004,24(4):392-394.
[5] 刘亚光,张文福,牛力春,等.带蒂胆囊瓣转移修补肝外胆管壁缺损[J].西北国防医药杂志,2000,12(4):285-286.
[6] 李振水,李春林,赵延玲,等.带蒂空肠瓣移植修复肝外胆管缺损九例报告[J].齐鲁肿瘤杂志,1999,6(2):124-125.
[7] Comez NA,Alvarez LR,Mite A,et al.Repair of bileduct injuries with Gore-Tex vas-cular grafts:experimental study in dogs. Gastrointest Surg.2002;6(1):116.
[8] 任为,时德.胆管修复与重建材料的研究及其临床应用[J].中国普通外科杂志,2002,11(2):109-110.
[9] 窦春青,周宁新.组织工程化人工胆管材料学研究进展[J].解放军医学杂志,2007,32(3):672-673.
[10] Livesey SA,Herndon DN,Hollyoak MA,et al.Transplanted acellular allograft dermal matrix. Potential as a template for the reconstruction of viable dermis. Transplantation. 1995;60: 1-9.
[11] Wainwright DJ.Use of an acellular allografe dermal matrix (ALLoDerm) in the management of full-thickness burns.Burns. 1995;21:243-248.
[12] 刘流,梁德江,申鹏飞,等.脱细胞膀胱细胞外基质作为膀胱替代材料的实验研究[J].中华实验外科杂志,1999,16(2):181-182.
[13] 李健,李志强,杨汉林.脱细胞异体真皮基质口腔组织补片在颌面外科的应用[J].医学临床研究,2004,9(21):1070.
[14] 傅小兵,王德文.创伤修复基础[M].北京:人民军医出版社,1997: 12.
[15] Wahl SM. The role of transforming growth facto r- beta in inflammatory p rocesses. Imm unol Res.1991;10:249.
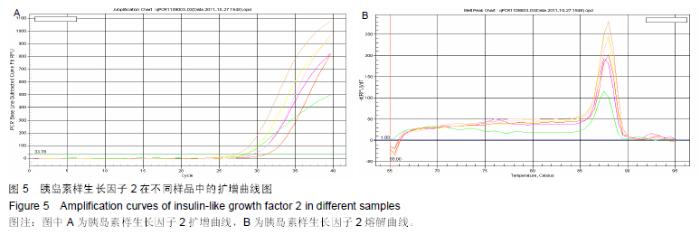
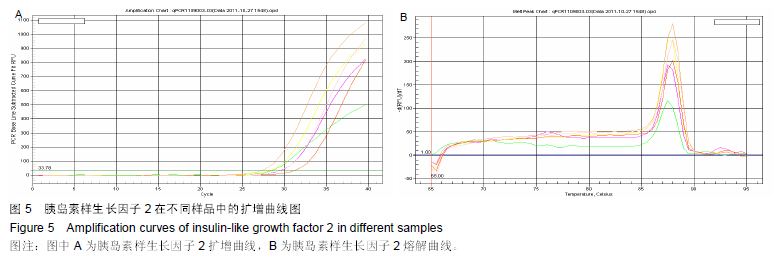
Zvibel Z,Brill S,Reid LM,et al.Insulin-like growth factor II regulation of gene expression in rat and human hepatomas.J Cell Physiol.1995;162(1):36-43. |