Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (44): 7071-7076.doi: 10.3969/j.issn.2095-4344.2014.44.004
Previous Articles Next Articles
Correlation of periprosthetic stress and bone mineral density after total knee arthroplasty
Zang Xue-hui, Sun Hui, Gao Li-hua, Ding Hui-xia, Miao Gui-qiang
- Second Department of Orthopedics, Nanhai Hospital Affiliated to Southern Medical University, Foshan 528200, Guangdong Province, China
-
Online:2014-10-22Published:2014-10-22 -
About author:Zang Xue-hui, Master, Associate chief physician, Second Department of Orthopedics, Nanhai Hospital Affiliated to Southern Medical University, Foshan 528200, Guangdong Province, China -
Supported by:the Foshan Municipal Scientific and Technological Project, No. 201208150
CLC Number:
Cite this article
Zang Xue-hui, Sun Hui, Gao Li-hua, Ding Hui-xia, Miao Gui-qiang. Correlation of periprosthetic stress and bone mineral density after total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(44): 7071-7076.
share this article
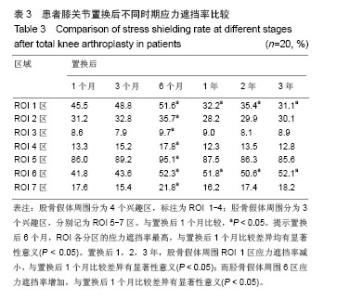
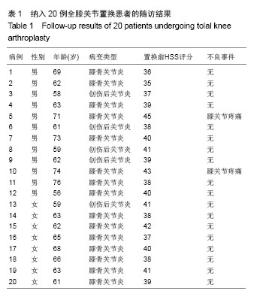
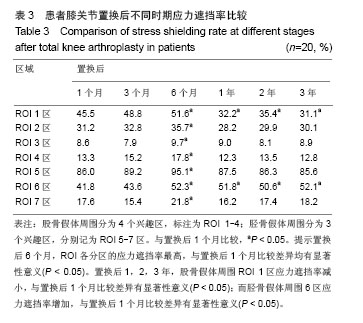
2.4 膝关节假体周围应力分析 在置换后1,3,6个月以及置换后1,2,3年分别检测ROI各区的应力遮挡变化。由结果可见,置换后6个月,ROI各分区的应力遮挡率最高,与置换后1个月比较差异均有显著性意义(P < 0.05)。置换后1,2,3年,股骨假体周围ROI 1区应力遮挡率减小,与置换后1个月比较,差异有显著性意义(P < 0.05);而胫骨假体周围6区应力遮挡率增加,与置换后1个月比较,差异有显著性意义(P < 0.05)。其中胫骨假体周围ROI 5区应力遮挡最明显,置换后6个月可达到91%,而随着随访的延长,ROI 5区应力遮挡率有所下降;股骨假体周围ROI 2区和胫骨假体周围ROI7区应力遮挡率较低,其中股骨假体周围ROI 3区应力遮挡最少,见表3。"
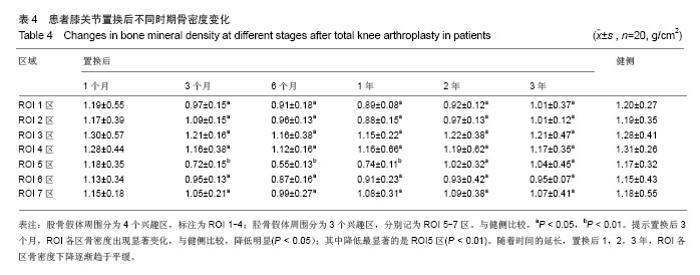
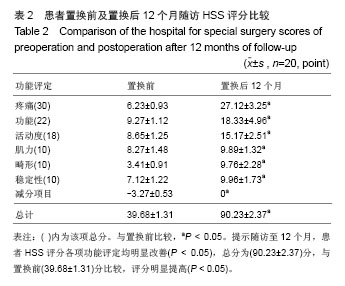
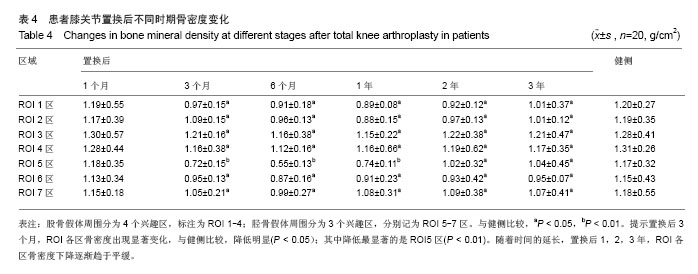
2.5 膝关节假体周围骨密度分析 在置换后1,3,6个月以及置换后1,2,3年利用骨密度仪分别检测ROI各区的骨密度。由结果可见,置换后1个月,ROI各区骨密度无明显变化,与健侧比较,差异无显著性意义(P > 0.05)。置换后3个月,ROI各区骨密度出现显著变化,与健侧比较,降低明显(P < 0.05);其中降低最显著的是ROI 5区(P < 0.01),骨密度相对下降较少的是ROI 2区和ROI 7区,骨密度下降最少的是ROI 3区。随着时间的延长,置换后1,2,3年,ROI各区不再继续下降,骨密度下降逐渐趋于平缓,见表4。 2.6 不良事件 在12个月的随访期间,所有患者均未发生感染或假体松动的情况,其中2例患者置换后出现较轻的但不影响正常活动的膝部关节疼痛。"
| [1]DeCrane SK, Stark LD, Johnston B, et al. Pain, opioids, and confusion after arthroplasty in older adults. Orthop Nurs. 2014; 33(4):226-232. [2]Losina E, Paltiel AD, Weinstein AM, et al. Lifetime medical costs of knee osteoarthritis management in the United States: Impact of extending indications for total knee arthroplasty. Arthritis Care Res (Hoboken). 2014; 21(2):312-317. [3]Zhang S, Paul J, Nantha-Aree M, et al. Empirical comparison of four baseline covariate adjustment methods in analysis of continuous outcomes in randomized controlled trials. Clin Epidemiol. 2014;6:227-235. [4]Skedros JG, Knight AN, Thomas SC, et al. Dilemma of high rate of conversion from knee arthroscopy to total knee arthroplasty.Am J Orthop (Belle Mead NJ). 2014;43(7): E153-158. [5]Minoda Y, Kobayashi A, Iwaki H, et al. Comparison of bone mineral density between porous tantalum and cemented tibial total knee arthroplasty components. J Bone Joint Surg Am. 2010;92(3):700-706. [6]Minoda Y, Ikebuchi M, Kobayashi A, et al. A cemented mobile-bearing total knee replacement prevents periprosthetic loss of bone mineraldensity around the femoral component: a matched cohort study. J Bone Joint Surg Br. 2010;92(6):794-798. [7]Grupp TM, Pietschmann MF, Holderied M, et al. Primary stability of unicompartmental knee arthroplasty under dynamic compression-shear loading in human tibiae. Clin Biomech (Bristol, Avon). 2013;28(9-10):1006-1013. [8]Herrera A, Rebollo S, Ibarz E, et al. Mid-term study of bone remodeling after femoral cemented stem implantation: comparison between DXA and finite element simulation. J Arthroplasty. 2014;29(1):90-100. [9]Jayasuriya RL, Buckley SC, Hamer AJ, et al. Effect of sliding-taper compared with composite-beam cemented femoral prosthesis loading regime on proximal femoral bone remodeling: a randomized clinical trial. J Bone Joint Surg Am. 2013;95(1):19-27. [10]Merle C, Sommer J, Streit MR, et al. Influence of surgical approach on postoperative femoral bone remodelling after cementless total hiparthroplasty. Hip Int. 2012;22(5):545-554. [11]Veldstra R, van Dongen A, Kraaneveld EC. Comparing alumina-reduced and conventional surface grit-blasted acetabular cups in primary THA: early results from a randomised clinical trial. Hip Int. 2012;22(3):296-301. [12]Stukenborg-Colsman CM, von der Haar-Tran A, Windhagen H, et al. Bone remodelling around a cementless straight THA stem: a prospective dual-energy X-ray absorptiometry study. Hip Int. 2012;22(2):166-171. [13]Hayashi S, Nishiyama T, Fujishiro T, et al. Periprosthetic bone mineral density with a cementless triple tapered stem is dependent on daily activity. Int Orthop. 2012;36(6):1137-1142. [14]Chandran P, Azzabi M, Andrews M, et al. Periprosthetic bone remodeling after 12 years differs in cemented and uncemented hip arthroplasties. Clin Orthop Relat Res. 2012; 470(5):1431-1435 [15]Nazari Moghadam K, Aghili H, Rashed Mohassel A, et al. A comparative study on sealing ability of mineral trioxide aggregate, calcium enriched cement andbone cement in furcal perforations. Minerva Stomatol. 2014;63(6):203-210. [16]Park YS, Lee JY, Suh JS, et al. Selective osteogenesis by a synthetic mineral inducing peptide for the treatment of osteoporosis. Biomaterials. 2014;35(37):9747-9754. [17]Boyde A, Davis GR, Mills D, et al. On fragmenting, densely mineralised acellular protrusions into articular cartilage and their possible role in osteoarthritis. J Anat. 2014;225(4): 436-446. [18]Crawford B, Kim DG, Moon ES, et al.Cervical vertebral bone mineral density changes in adolescents during orthodontic treatment. Am J Orthod Dentofacial Orthop. 2014;146(2): 183-189. [19]Kiriyama Y, Matsumoto H, Toyama Y, et al. A miniature tension sensor to measure surgical suture tension of deformable musculoskeletal tissues during joint motion. Proc Inst Mech Eng H. 2014;228(2):140-148. [20]Sun ZH, Liu YJ, Li H. Femoral stress and strain changes post-hip, -knee and -ipsilateral hip/knee arthroplasties: a finite element analysis. Orthop Surg. 2014;6(2):137-144. [21]Kwon OR, Kang KT, Son J, et al. Biomechanical comparison of fixed- and mobile-bearing for unicomparmental knee arthroplastyusing finite element analysis. J Orthop Res. 2014; 32(2):338-345. [22]Chan Â, Gamelas J, Folgado J, et al. Biomechanical analysis of the tibial tray design in TKA: comparison between modular and offset tibial trays. Knee Surg Sports Traumatol Arthrosc. 2014;22(3):590-598. [23]Deleuran T, Vilstrup H, Overgaard S, et al. Cirrhosis patients have increased risk of complications after hip or knee arthroplasty. Acta Orthop. 2014:1-6. [24]Simpson DJ, Kendrick BJ, Dodd CA, et al.Load transfer in the proximal tibia following implantation with a unicompartmental knee replacement: a static snapshot. Proc Inst Mech Eng H. 2011;225(5):521-529. [25]Husted H, Gromov K, Malchau H, et al. Traditions and myths in hip and knee arthroplasty. Acta Orthop. 2014:1-8. [26]Niemeläinen M, Kalliovalkama J, Aho AJ, et al. Single periarticular local infiltration analgesia reduces opiate consumption until 48 hours after total knee arthroplasty. Acta Orthop. 2014:1-6. [27]Lavernia CJ, Rodriguez JA, Iacobelli DA, et al. Bone mineral density of the femur in autopsy retrieved total knee arthroplasties. J Arthroplasty. 2014;29(8):1681-1686. [28]Kim KK, Won YY, Heo YM, et al. Changes in bone mineral density of both proximal femurs after total knee arthroplasty. Clin Orthop Surg. 2014;6(1):43-48. [29]van de Groes S, de Waal-Malefijt M, Verdonschot N. Probability of mechanical loosening of the femoral component in high flexion total knee arthroplasty can be reduced by rather simple surgical techniques. Knee. 2014;21(1):209-215. [30]Amirouche F, Choi KW, Goldstein WM, et al. Finite element analysis of resurfacing depth and obliquity on patella stress and stability in TKA. J Arthroplasty. 2013;28(6):978-984. [31]Lavernia CJ, Rodriguez JA, Iacobelli DA, et al. Bone mineral density of the femur in autopsy retrieved total knee arthroplasties. J Arthroplasty. 2014;29(8):1681-1686. [32]Kim KK, Won YY, Heo YM, et al. Changes in bone mineral density of both proximal femurs after total knee arthroplasty. Clin Orthop Surg. 2014;6(1):43-48. |
| [1] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [2] | Cai Qunbin, Zou Xia, Hu Jiantao, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei. Relationship between tip-apex distance and stability of intertrochanteric femoral fractures with proximal femoral anti-rotation nail: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 831-836. |
| [3] | Yang Weiqiang, Ding Tong, Yang Weike, Jiang Zhengang. Combined variable stress plate internal fixation affects changes of bone histiocyte function and bone mineral density at the fractured end of goat femur [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 890-894. |
| [4] | Song Chengjie, Chang Hengrui, Shi Mingxin, Meng Xianzhong. Research progress in biomechanical stability of lateral lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 923-928. |
| [5] | Liu Zhao, Xu Xilin, Shen Yiwei, Zhang Xiaofeng, Lü Hang, Zhao Jun, Wang Zhengchun, Liu Xuzhuo, Wang Haitao. Guiding role and prospect of staging and classification combined collapse prediction method for osteonecrosis of femoral head [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 929-934. |
| [6] | Chen Lu, Zhang Jianguang, Deng Changgong, Yan Caiping, Zhang Wei, Zhang Yuan. Finite element analysis of locking screw assisted acetabular cup fixation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 356-361. |
| [7] | Shu Qihang, Liao Yijia, Xue Jingbo, Yan Yiguo, Wang Cheng. Three-dimensional finite element analysis of a new three-dimensional printed porous fusion cage for cervical vertebra [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3810-3815. |
| [8] | Zhu Yun, Chen Yu, Qiu Hao, Liu Dun, Jin Guorong, Chen Shimou, Weng Zheng. Finite element analysis for treatment of osteoporotic femoral fracture with far cortical locking screw [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3832-3837. |
| [9] | Liu Jinyu, Ding Yiwei, Lu Zhengcao, Gao Tianjun, Cui Hongpeng, Li Wen, Du Wei, Ding Yu. Finite element biomechanical study of full endoscopic fenestration decompression for cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3850-3854. |
| [10] | Qin Wan’an, Cai Zhouyu, Wei Gejin, Lin Zhoudan. Finite element analysis of absorbable screws and ethibond sutures for the treatment of humerus shaft fractures caused by grenade throwing [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3855-3859. |
| [11] | Cai Qunbin, Yang Lijuan, Li Qiumin, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei . Feasibility of internal fixation removal of intertrochanteric fractures in elderly patients based on fracture mechanics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3313-3318. |
| [12] | Wei Yuanbiao, Guo Huizhi, Zhang Shuncong. Finite element analysis of cortical bone trajectory screw fixation on adjacent segments [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2799-2804. |
| [13] | Qu Xingyue, Zhou Jianqiang, Xu Xuebin, Zhang Shaojie, Li Zhijun, Wang Xing. Finite element analysis of screw-bone anti-pullout in four models of anterior lower cervical fixation in children [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2816-2821. |
| [14] | Ruan Hanjiang, Jin Genyang, Li Xinwu, Yao Jian, Wu Peng, Zhang Yin, Zhang Shuai, Xiao Jun . Biomechanical properties of three types of posterior single-segment fixation for type II Hangman’s fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2309-2314. |
| [15] | Fan Zhirong, Su Haitao, Zhou Lin, Huang Huida, Zhou Junde, Jiang Tao, Liu Zitao. Finite element analysis of novel femoral neck system for unstable femoral neck fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(15): 2321-2328. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 173
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 252
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||