Chinese Journal of Tissue Engineering Research
Previous Articles Next Articles
Human umbilical cord blood mesenchymal stem cell transplantation improves the liver function of liver cirrhosis rats
Liao Jin-mao1, Hu Xiao-xuan1, Li Zhuo-ri2
- 1Department of Hepatopathy, People’s Hospital of Hunan Province, Changsha 410006, Hunan Province, China; 2Department of Hepatobiliary Surgery, Haikou 570311, Hainan Province, China
-
Received:2012-10-21Revised:2012-12-06Online:2013-07-02Published:2013-07-02 -
Contact:Hu Xiao-xuan, Master, Chief physician, Professor, Department of Hepatopathy, People’s Hospital of Hunan Province, Changsha 410006, Hunan Province, China hxx5527392@sina.com -
About author:Liao Jin-mao★, Master, Physician, Department of Hepatopathy, People’s Hospital of Hunan Province, Changsha 410006, Hunan Province, China xlyyan5300@163.com
CLC Number:
Cite this article
Liao Jin-mao, Hu Xiao-xuan, Li Zhuo-ri . Human umbilical cord blood mesenchymal stem cell transplantation improves the liver function of liver cirrhosis rats[J]. Chinese Journal of Tissue Engineering Research, doi: 10.3969/j.issn.2095-4344.2013.27.010.
share this article

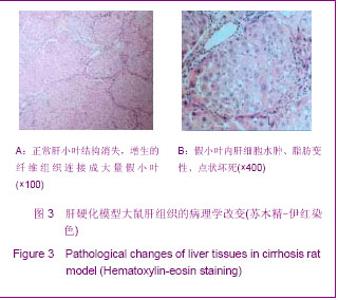
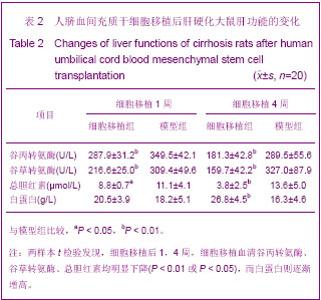
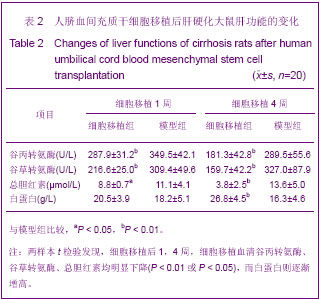
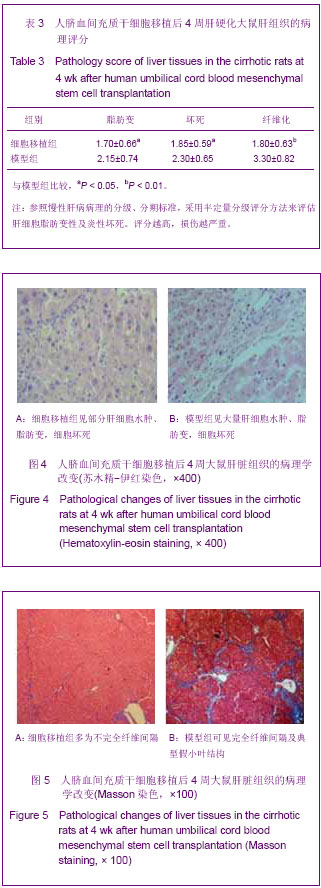
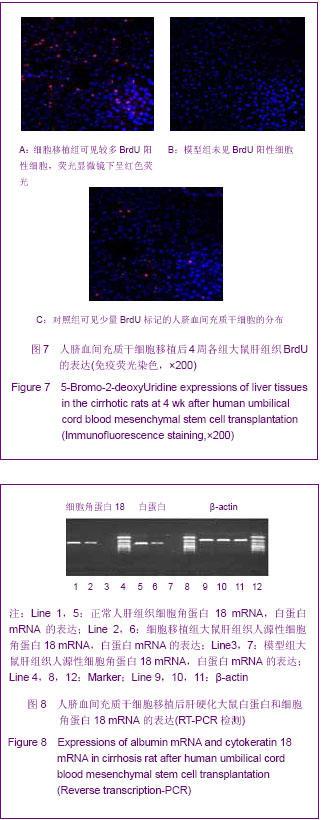
人脐血间充质干细胞移植后4周,细胞移植组大鼠仍有部分肝细胞水肿、脂肪变性、细胞坏死,汇管区炎性细胞浸润等改变;肝内纤维组织增生,可见部分不完全纤维间隔形成;但与模型组比较,细胞移植组大鼠肝细胞脂肪变性、细胞坏死等程度均减轻(P < 0.05);肝纤维化程度明显改善(P < 0.01)。 2.7 Brdu标记的人脐血间充质干细胞的肝内定植情况 免疫组化染色显示,细胞移植组大鼠肝脏中可见BrdU标记的人脐血间充质干细胞的分布,细胞核呈棕黄色,数量多少不等,呈颗粒样或弥漫性分布,且多定植于肝小叶周围门管区附近;模型组大鼠肝组织未见BrdU阳性细胞;对照组大鼠肝内可见少量BrdU标记的人脐血间充质干细胞的分布。经细胞计数,平均每100倍视野下细胞移植组大鼠肝内人脐血间充质干细胞的定植数量明显多于对照组(38.7± 9.8,12.7±4.8;P < 0.01),见图6。"

| [1] Capla JM, Grogan RH, Callaghan MJ, et al. Diabetes impairs endothelial progenitor cell-mediated blood vessel formation in response to hypoxia. Plast Reconstr Surg. 2007;119(1):59-70.[2] Danet GH, Luongo JL, Butler G, et al. C1qRp defines a new human stem cell population with hematopoietic and hepatic potential. Proc Natl Acad Sci U S A. 2002;99(16):10441- 10445.[3] Hong SH, Gang EJ, Jeong JA, et al. In vitro differentiation of human umbilical cord blood-derived mesenchymal stem cells into hepatocyte-like cells.Biochem Biophys Res Commun. 2005;330(4):1153-1161.[4] 陈海鸥,胡小宣,刘红娟,等.脐血干细胞移植治疗肝硬化的疗效观察[J].中华肝脏病杂志,2010,18(7):537-538.[5] Jung KH, Shin HP, Lee S, et al. Effect of human umbilical cord blood-derived mesenchymal stem cells in a cirrhotic rat model. Liver Int. 2009;29(6):898-909. [6] 金光鑫,吴德全.脐带血间充质干细胞研究进展[J].国际移植与血液净化杂志,2006,4(5):45-48.[7] Romanov YA, Svintsitskaya VA, Smirnov VN. Searching for alternative sources of postnatal human mesenchymal stem cells: candidate MSC-like cells from umbilical cord. Stem Cells. 2003;21(1):105-110.[8] Jonker AM, Dijkhuis FW, Boes A, et al. Immunohistochemical study of extracellular matrix in acute galactosamine hepatitis in rats. Hepatology. 1992;15(3):423-431.[9] Jonker AM, Dijkhuis FW, Kroese FG, et al. Immunopathology of acute galactosamine hepatitis in rats. Hepatology. 1990; 11(4):622-627. [10] Yan L, Xu SP, Wang SZ, et al. G-CSF mobilized PBMCs contribute to the liver function of cirrhotic rats. Excli J. 2010; 9:67-75.[11] Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells.The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315-317.[12] Jiang Y, Jahagirdar BN, Reinhardt RL, et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002;418(6893):41-49.[13] Yang CC, Shih YH, Ko MH, et al. Transplantation of human umbilical mesenchymal stem cells from Wharton's jelly after complete transection of the rat spinal cord. PLoS One. 2008; 3(10):e3336.[14] Chao KC, Chao KF, Fu YS, et al. Islet-like clusters derived from mesenchymal stem cells in Wharton's Jelly of the human umbilical cord for transplantation to control type 1 diabetes. PLoS One.2008;3(1):e1451.[15] Moodley Y, Atienza D, Manuelpillai U, et al. Human umbilical cord mesenchymal stem cells reduce fibrosis of bleomycin-induced lung injury. Am J Pathol. 2009;175(1): 303-313. [16] Prasanna SJ, Gopalakrishnan D, Shankar SR, et al. Pro-inflammatory cytokines, IFNgamma and TNFalpha, influence immune properties of human bone marrow and Wharton jelly mesenchymal stem cells differentially. PLoS One. 2010;5(2):e9016.[17] Liu Y, Mu R, Wang S, et al. Therapeutic potential of human umbilical cord mesenchymal stem cells in the treatment of rheumatoid arthritis. Arthritis Res Ther. 2010;12(6):R210.[18] Zhao L, Weir MD, Xu HH. Human umbilical cord stem cell encapsulation in calcium phosphate scaffolds for bone engineering. Biomaterials. 2010;31(14):3848-3857.[19] Struys T, Moreels M, Martens W, et al. Ultrastructural and immunocytochemical analysis of multilineage differentiated human dental pulp- and umbilical cord-derived mesenchymal stem cells. Cells Tissues Organs. 2011;193(6):366-378.[20] Chang SJ, Weng SL, Hsieh JY, et al. MicroRNA-34a modulates genes involved in cellular motility and oxidative phosphorylation in neural precursors derived from human umbilical cord mesenchymal stem cells. BMC Med Genomics. 2011;4:65.[21] Zhao Z, Chen Z, Zhao X, et al. Sphingosine-1-phosphate promotes the differentiation of human umbilical cord mesenchymal stem cells into cardiomyocytes under the designated culturing conditions. J Biomed Sci. 2011;18:37.[22] Tse W, Laughlin MJ. Umbilical cord blood transplantation: a new alternative option. Hematology Am Soc Hematol Educ Program. 2005:377-383.[23] 胡荣昕,缪伟峰.肝纤维化动物模型的研究概况[J].实用肝脏病杂志,2007,10(2):133-135.[24] Friedman SL. Mechanisms of hepatic fibrogenesis. Gastroenterology. 2008;134(6):1655-1669.[25] Serrano AL, Mann CJ, Vidal B, et al. Cellular and molecular mechanisms regulating fibrosis in skeletal muscle repair and disease. Curr Top Dev Biol. 2011;96:167-201.[26] 覃慧敏,田卫群.骨髓间充质干细胞经不同移植途径治疗终末期肝病[J].中华临床医师杂志,2011,5(21):6416-6418.[27] Kim WH, Matsumoto K, Bessho K, et al. Growth inhibition and apoptosis in liver myofibroblasts promoted by hepatocyte growth factor leads to resolution from liver cirrhosis. Am J Pathol. 2005;166(4):1017-1028.[28] Kakinuma S, Tanaka Y, Chinzei R, et al. Human umbilical cord blood as a source of transplantable hepatic progenitor cells. Stem Cells. 2003;21(2):217-227. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Zhang Xiumei, Zhai Yunkai, Zhao Jie, Zhao Meng. Research hotspots of organoid models in recent 10 years: a search in domestic and foreign databases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1249-1255. |
| [3] | Wang Zhengdong, Huang Na, Chen Jingxian, Zheng Zuobing, Hu Xinyu, Li Mei, Su Xiao, Su Xuesen, Yan Nan. Inhibitory effects of sodium butyrate on microglial activation and expression of inflammatory factors induced by fluorosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1075-1080. |
| [4] | Wang Xianyao, Guan Yalin, Liu Zhongshan. Strategies for improving the therapeutic efficacy of mesenchymal stem cells in the treatment of nonhealing wounds [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1081-1087. |
| [5] | Liao Chengcheng, An Jiaxing, Tan Zhangxue, Wang Qian, Liu Jianguo. Therapeutic target and application prospects of oral squamous cell carcinoma stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1096-1103. |
| [6] | Xie Wenjia, Xia Tianjiao, Zhou Qingyun, Liu Yujia, Gu Xiaoping. Role of microglia-mediated neuronal injury in neurodegenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1109-1115. |
| [7] | Li Shanshan, Guo Xiaoxiao, You Ran, Yang Xiufen, Zhao Lu, Chen Xi, Wang Yanling. Photoreceptor cell replacement therapy for retinal degeneration diseases [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1116-1121. |
| [8] | Jiao Hui, Zhang Yining, Song Yuqing, Lin Yu, Wang Xiuli. Advances in research and application of breast cancer organoids [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1122-1128. |
| [9] | Wang Shiqi, Zhang Jinsheng. Effects of Chinese medicine on proliferation, differentiation and aging of bone marrow mesenchymal stem cells regulating ischemia-hypoxia microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1129-1134. |
| [10] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [11] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [12] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [13] | Shi Yangyang, Qin Yingfei, Wu Fuling, He Xiao, Zhang Xuejing. Pretreatment of placental mesenchymal stem cells to prevent bronchiolitis in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 991-995. |
| [14] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [15] | Fan Quanbao, Luo Huina, Wang Bingyun, Chen Shengfeng, Cui Lianxu, Jiang Wenkang, Zhao Mingming, Wang Jingjing, Luo Dongzhang, Chen Zhisheng, Bai Yinshan, Liu Canying, Zhang Hui. Biological characteristics of canine adipose-derived mesenchymal stem cells cultured in hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1002-1007. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||