Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (5): 803-810.doi: 10.3969/j.issn.2095-4344.1888
Previous Articles Next Articles
Meta-analysis of bone morphogenetic protein versus autologous bone grafting for limb long bone nonunion
Xie Chengxin1, Yu Chengqiang1, Wang Wei1, Wang Chenglong2, Yin Dong2
- 1Graduate School of Guangxi University of Chinese Medicine, Nanning 530200, Guangxi Zhuang Autonomous Region, China; 2Department of Orthopedics, The People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530021, Guangxi Zhuang Autonomous Region, China
-
Received:2019-05-13Revised:2019-05-25Accepted:2019-07-05Online:2020-02-18Published:2020-01-15 -
Contact:Yin Dong, MD, Master’s supervisor, Chief physician, The People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530021, Guangxi Zhuang Autonomous Region, China Wang Chenglong, Doctoral candidate, The People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530021, Guangxi Zhuang Autonomous Region, China -
About author:Xie Chengxin, Master candidate, Graduate School of Guangxi University of Chinese Medicine, Nanning 530200, Guangxi Zhuang Autonomous Region, China
CLC Number:
Cite this article
Xie Chengxin, Yu Chengqiang, Wang Wei, Wang Chenglong, Yin Dong. Meta-analysis of bone morphogenetic protein versus autologous bone grafting for limb long bone nonunion[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(5): 803-810.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
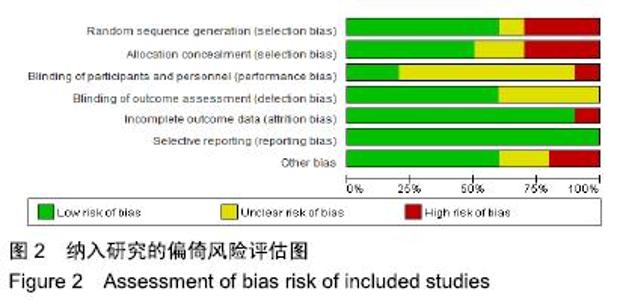
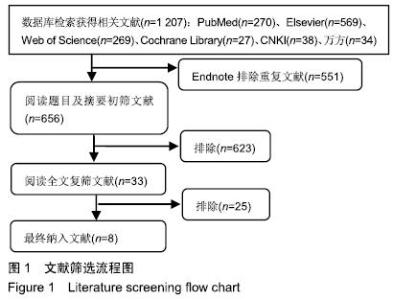
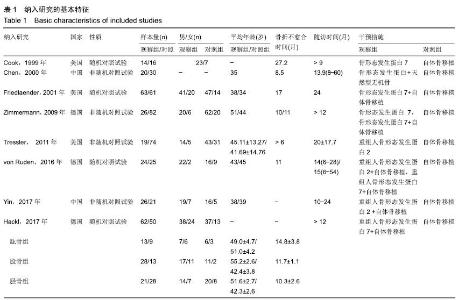
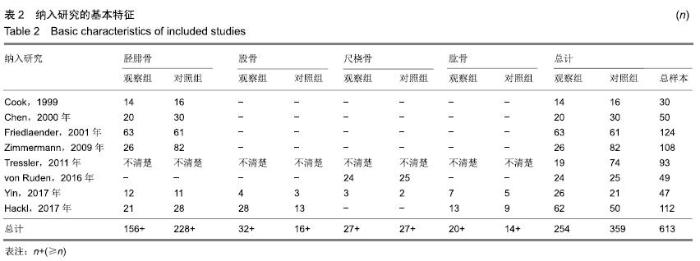
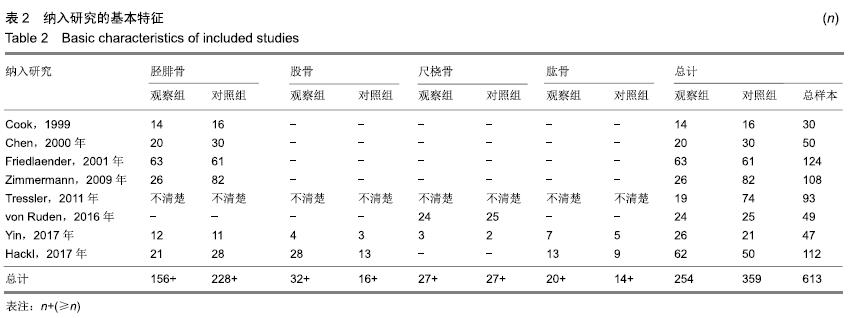
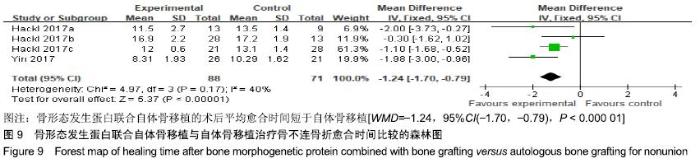
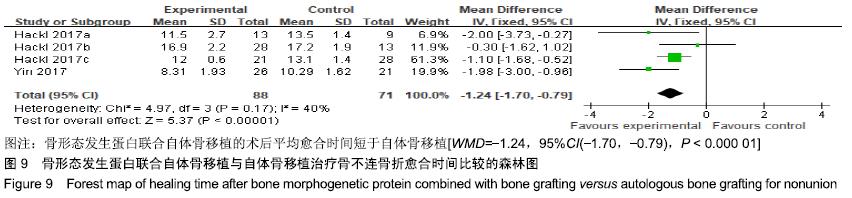
最终纳入8篇文献,共10个对照研究(“Hackl,2017年”包含3个随机对照研究)。其中,4篇为随机对照研究[15-17,19],4篇为非随机对照研究[18,20-22],多为30-124例的小样本量研究,共计613例骨不连患者;4篇研究中的观察组采用骨形态发生蛋白联合自体骨移植[16-17,19,22],2篇研究的观察组单用骨形态发生蛋白[15,18],1篇研究的观察组采用骨形态发生蛋白联合天然无机骨[21],1篇研究的观察组包含18例单用骨形态发生蛋白和8例骨形态发生蛋白联合自体骨移植的患者[20];纳入的8篇文献中所有对照组均为自体骨移植,且所有患者(包含观察组和对照组)均进行机械固定(髓内钉、钢板、螺钉、微创稳定系统、外固定等)。纳入文献质量评价及风险评估结果见图2,纳入研究的基本特征见表1,2。 "
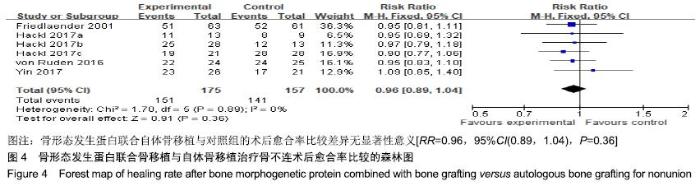
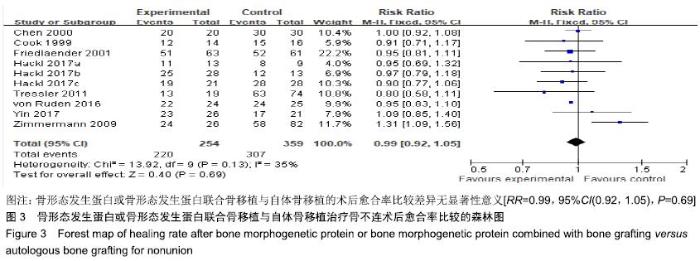
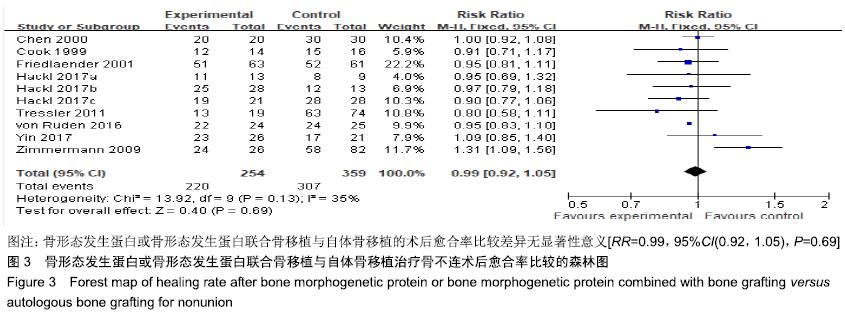
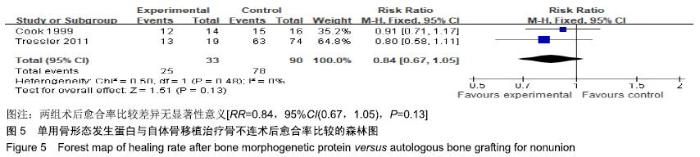
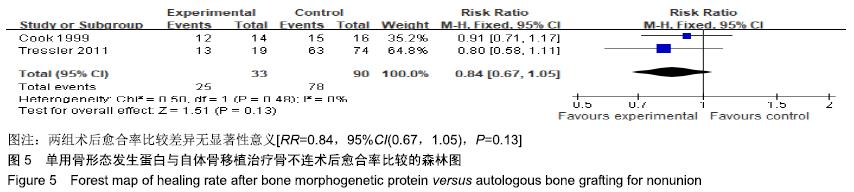
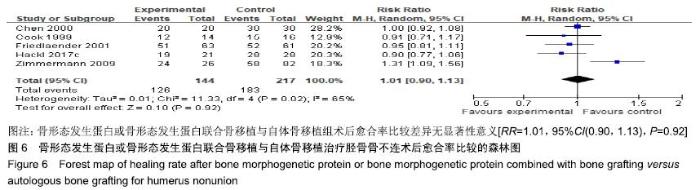
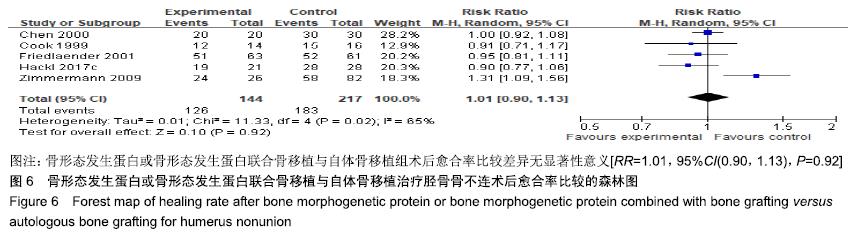
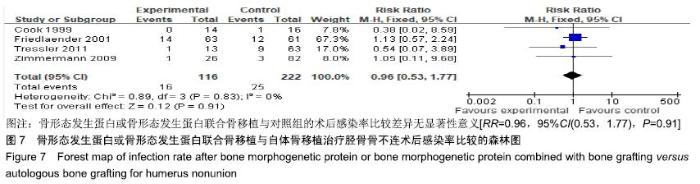
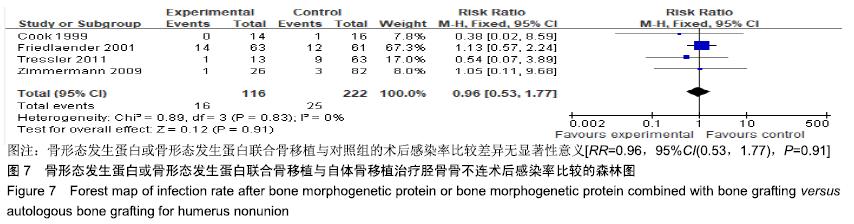
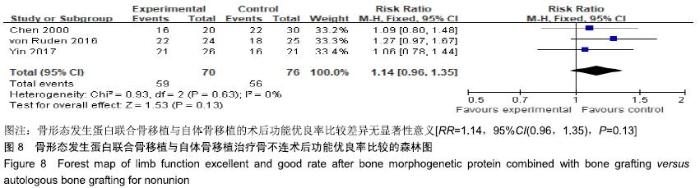
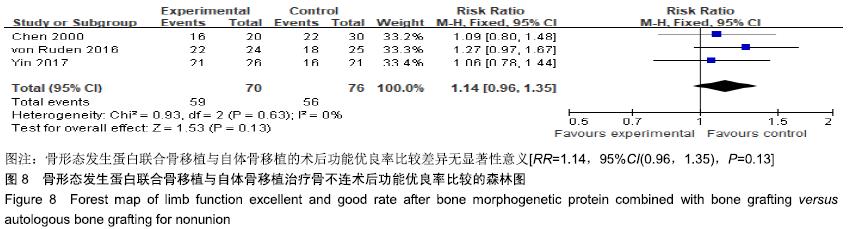
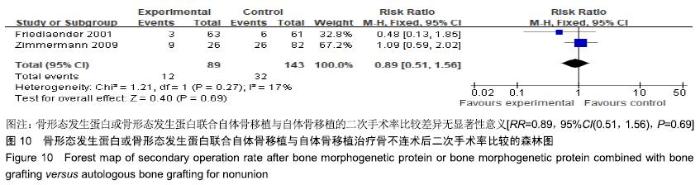
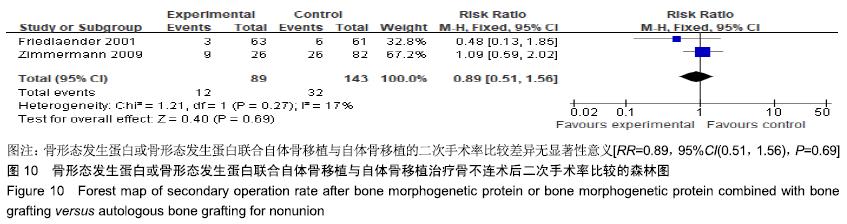
对纳入的每项研究剔除1次,剩余研究做合并分析,此敏感性分析结果显示当剔除“Zimmermann,2009年”的研究后,异质性改变明显(I2=0%,P=0.79),但对结果影响较小[RR=0.97,95%CI(0.92,1.02),P=0.22]。分析产生异质性的原因:“Zimmermann,2009年”的研究中:①所有病例均有自体骨移植修复失败的既往史,骨形态发生蛋白作为全新的局部刺激物可能对这些患者具有更好的反应性。该研究结果认为在多次手术失败的病例中,骨形态发生蛋白具有更高的功效;②骨形态发生蛋白组的病例数相比对照组较少,也可能导致异质性产生。 根据观察组干预措施,仅纳入4篇骨形态发生蛋白联合自体骨移植的研究[16-17,19,22]。各组间无统计学异质性(I2=0%,P=0.89),采用固定效应模型,结果显示骨形态发生蛋白联合自体骨移植与对照组的术后愈合率比较差异无显著性意义[RR=0.96,95%CI(0.89,1.04),P=0.36],见图4;仅纳入2篇单用骨形态发生蛋白的研究[15,18],两组研究间无统计学异质性(I2=0%,P=0.48),采用固定效应模型,结果显示单用骨形态发生蛋白与对照组的术后愈合率比较差异无显著性意义[RR=0.84,95%CI(0.67,1.05),P=0.13],见图5。 "
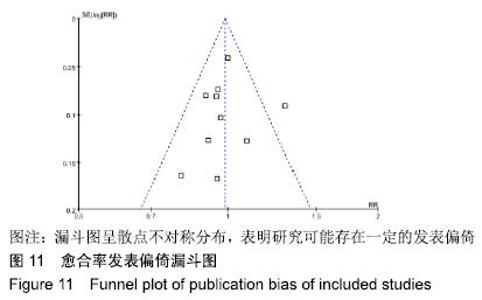
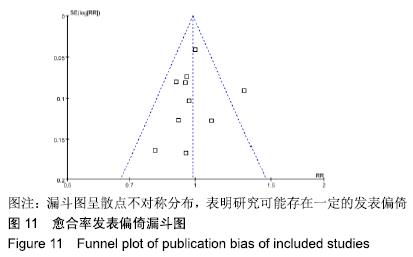
2.2.6 手术时间和出血量 2篇文献报道了手术时间[18,22]、出血量[18],但由于两研究间骨形态发生蛋白组的干预措施有差异,未采取合并分析。“Yin,2017年”的研究中报道了手术时间的比较,包括骨形态发生蛋白联合自体骨移植组26例和对照组21例,手术时间分别为(70.96±13.34) min和(101.67±12.78) min,两组比较差异有显著性意义(P < 0.01),表明骨形态发生蛋白联合自体骨移植组比对照组的手术时间更短。“Tressler,2011年”的研究报道了手术时间和术中出血量的比较,包括单用骨形态发生蛋白组19例和对照组74例,手术时间分别为(168.9±86.5),(257.9±93) min,两组比较差异有显著性意义(P < 0.01),表明单用骨形态发生蛋白组比对照组的手术时间更短;术中出血量分别为(331.6±357.2),(554.6±447.8) mL,两组比较差异有显著性意义(P=0.02),表明单用骨形态发生蛋白组比对照组的术中出血量更少。 2.2.7 住院时间和住院费用 2篇文献分别报道了住院时间[18]、住院费用情况[22]。“Tressler,2011年”的研究报道了住院时间的比较,单用骨形态发生蛋白组住院时间为(3.2±2.6) d,对照组住院时间为(3.8±2.5) d,两组住院时间的比较差异无显著性意义(P=0.37)。“Yin,2017年”的研究报道了平均住院费用的比较,骨形态发生蛋白联合自体骨移植组和对照组的住院费用分别为(2.65±0.34),(2.14±0.35)万元,两组比较差异有显著性意义(P < 0.01),表明骨形态发生蛋白联合自体骨移植组比对照组的住院费用更高。 2.3 发表偏倚分析 使用RevMan 5.1软件对文献进行发表偏倚分析。通过漏斗图进行评价发表偏倚时,原则上纳入的研究数不应少于10篇,否则会导致漏斗图的检验能力下降。此次Meta分析共纳入8篇文献,但包含了10个对照研究,因此有必要进行发表偏倚漏斗图分析。对术后愈合率进行偏倚风险评估,结果显示漏斗图呈散点不对称分布,表明研究可能存在一定的发表偏倚,见图11。 "
| [1] SEN M, MICLAU T.Autologous iliac crest bone graft: should it still be the gold standard for treating nonunions?Injury. 2007;38(1):S75-S80. [2] DIMITRIOU R, MATALIOTAKIS GI, ANGOULES AG, et al. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review.Injury.2011;42 Suppl 2: S3-15. [3] ARRINGTON ED, SMITH WJ, CHAMBERS HG, et al.Complications of iliac crest bone graft harvesting.Clin Orthop Relat Res.1996;(329): 300-309. [4] LE BARON M, VIVONA JP, MAMAN P, et al.Can the Reamer/Irrigator/ Aspirator System replace anterior iliac crest grafting when treating long bone nonunion?Orthop Traumatol Surg Res.2019;105(3):529-533. [5] NODARIAN T, SARIALI E, KHIAMI F, et al.Iliac crest bone graft harvesting complications: A case of liver herniation.Orthop Traumatol Surg Res. 2010;96(5):593-596. [6] DIMITRIOU R, KANAKARIS N, SOUCACOS PN, et al.Genetic predisposition to non-union: evidence today.Injury.2013;44:S50-S53. [7] SINGH R, BLEIBLEH S, KANAKARIS NK, et al.Upper limb non-unions treated with BMP-7: efficacy and clinical results.Injury.2016;47 Suppl 6: S33-S39. [8] HREHA J, KRELL ES, BIBBO C.Role of recombinant human bone morphogenetic Protein-2 on hindfoot arthrodesis.Foot Ankle Clin. 2016; 21(4):793-802. [9] MARUPANTHORN K, TANTRAWATPAN C, KHEOLAMAI P, et al.Bone morphogenetic protein-2 enhances the osteogenic differentiation capacity of mesenchymal stromal cells derived from human bone marrow and umbilical cord.Int J Mol Med.2017;39(3):654-662. [10] BARCAK EA, BEEBE MJ.Bone Morphogenetic Protein: Is There Still a Role in Orthopedic Trauma in 2017?Orthop Clin North Am. 2017;48(3): 301-309. [11] DIMITRIOU R, DAHABREH Z, KATSOULIS E, et al.Application of recombinant BMP-7 on persistent upper and lower limb non-unions. Injury. 2005;36(4):S51-S59. [12] HISSNAUER TN, STIEL N, BABIN K, et al.Recombinant Human Bone Morphogenetic Protein-2 (rhBMP-2) for the Treatment of Nonunion of the Femur in Children and Adolescents: A Retrospective Analysis. Biomed Res Int.2017;2017:3046842. [13] KANAKARIS NK, CALORI GM, VERDONK R, et al.Application of BMP-7 to tibial non-unions: a 3-year multicenter experience.Injury. 2008;39 Suppl 2:S83-90. [14] DAI J, LI L, JIANG C, et al.Bone morphogenetic protein for the healing of tibial fracture: a meta-analysis of randomized controlled trials.PLoS One. 2015;10(10):e0141670. [15] COOK SD.Preclinical and clinical evaluation of osteogenic protein-1 (BMP-7) in bony sites.Orthopedics.1999;22(7):669-671. [16] FRIEDLAENDER GE, PERRY CR, COLE JD, et al.Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions.J Bone Joint Surg Am.2001;83-A Suppl 1(Pt 2):S151-158. [17] HACKL S, HIERHOLZER C, FRIEDERICHS J, et al.Long-term outcome following additional rhBMP-7 application in revision surgery of aseptic humeral, femoral, and tibial shaft nonunion.BMC Musculoskelet Disord. 2017;18(1):342. [18] TRESSLER MA, RICHARDS JE, Sofianos D, et al.Bone morphogenetic protein-2 compared to autologous iliac crest bone graft in the treatment of long bone nonunion.Orthopedics. 2011;34(12):e877-e884. [19] VON RÜDEN C, MORGENSTERN M, HIERHOLZER C, et al. The missing effect of human recombinant Bone Morphogenetic Proteins BMP-2 and BMP-7 in surgical treatment of aseptic forearm nonunion. Injury. 2016;47(4):919-924. [20] ZIMMERMANN G, WAGNER C, SCHMECKENBECHER K, et al. Treatment of tibial shaft non-unions: bone morphogenetic proteins versus autologous bone graft.Injury.2009;40:50-53. [21] 陈光,杨建中,许会敏,等.NNB/BMP复合物在胫骨骨折不愈合治疗中的应用[J].中国矫形外科杂志,2000,7(8):26-29. [22] 尹化阳,王皓宇,黄明,等.重组人骨形态发生蛋白-2治疗四肢长骨骨不连临床研究[J].淮海医药,2017,35(6):668-671. [23] FLIERL MA, SMITH WR, MAUFFREY C, et al.Outcomes and complication rates of different bone grafting modalities in long bone fracture nonunions: a retrospective cohort study in 182 patients.J Orthop Surg Res.2013;8(1):33. [24] SCHOELLES K, SNYDER D, KACZMAREK J, et al.The Role of Bone Growth Stimulating Devices and Orthobiologics in Healing Nonunion Fractures[Internet].Agency for Healthcare Research and Quality, 2005. [25] GARRISON KR, SHEMILT I, DONELL S, et al.Bone morphogenetic protein (BMP) for fracture healing in adults. Cochrane Database Syst Rev. 2010; (6):CD006950. [26] KANAKARIS NK, PALIOBEIS C, MANIDAKIS N, et al.Biological enhancement of tibial diaphyseal aseptic non-unions: the efficacy of autologous bone grafting, BMPs and reaming by-products. Injury. 2007; 38:S65-S75. [27] 孙彦平,乔国勇,王玉冰,等.自体髂骨复合骨形态发生蛋白与自体髂骨移植治疗骨折不连接的比较[J].中国组织工程研究与临床康复,2009,13(33): 6465-6468. [28] TAKEMOTO R, FORMAN J, TAORMINA DP, et al.No advantage to rhBMP-2 in addition to autogenous graft for fracture nonunion. Orthopedics. 2014; 37(6):e525-e530. [29] GIORGIO CALORI M, CAPANNA R, COLOMBO M, et al.Cost effectiveness of tibial nonunion treatment: A comparison between rhBMP-7 and autologous bone graft in two Italian centres.Injury.2013; 44(12):1871-1879. [30] SCHENKER ML, YANNASCOLI SM, DONEGAN D.Bone Morphogenetic Protein and Fractures: A Meta-Analysis//ORS 2014 Annual Meeting Poster,2014:15-18. [31] PAPE HC, EVANS A, KOBBE P.Autologous bone graft: properties and techniques.J Orthop Trauma. 2010;24:S36-S40. [32] DAHABREH Z, CALORI GM, KANAKARIS NK, et al.A cost analysis of treatment of tibial fracture nonunion by bone grafting or bone morphogenetic protein-7.Int Orthop. 2009;33(5):1407. [33] HAUSMANN M, EHNERT S, HOFMANN V, et al.Use of bone morphogenetic proteins (BMPs) for the treatment of Pseudarthroses- efficiency and therapy failure.Z Orthop Unfall. 2014;152(2):144-151. [34] PAPANAGIOTOU M, DAILIANA ZH, KARACHALIOS T, et al.RhBMP-7 for the treatment of nonunion of fractures of long bones.Bone Joint J. 2015; 97(7):997-1003. |
| [1] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [4] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [5] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [6] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [7] | Yuan Xinping, Shao Yanbo, Wu Chao, Wang Jianling, Tong Liangcheng, Li Ying. Accuracy of target bone segments in personalized differential modeling and simulation of CT scanning parameters at fracture end [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 912-916. |
| [8] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [9] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [10] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [11] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [12] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [13] | Deng Zhenhan, Huang Yong, Xiao Lulu, Chen Yulin, Zhu Weimin, Lu Wei, Wang Daping. Role and application of bone morphogenetic proteins in articular cartilage regeneration [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 798-806. |
| [14] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| [15] | Li Yang, Zhang Mingyong. Meta-analysis of the effect of double Endobutton and clavicular hook plate on the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 463-470. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||