Chinese Journal of Tissue Engineering Research ›› 2018, Vol. 22 ›› Issue (5): 692-697.doi: 10.3969/j.issn.2095-4344.0437
Previous Articles Next Articles
3D-cultured umbilical cord mesenchymal stem cells for treatment of type 1 diabetes: therapeutic effects and immunomodulatory mechanism
Liu Ke-na1, Li Dong2, Yang Guang-sheng1
- 1Clinical Laboratory, Binzhou City Hospital of Traditional Chinese Medicine, Binzhou 256613, Shandong Province, China; 2Cryomedicine Laboratory, Qilu Hospital of Shandong University, Jinan 250012, Shandong Province, China
-
Revised:2017-09-13Online:2018-02-18Published:2018-02-18 -
Contact:Yang Guang-sheng, Associate chief laboratorian, Clinical Laboratory, Binzhou City Hospital of Traditional Chinese Medicine, Binzhou 256613, Shandong Province, China -
About author:Liu Ke-na, Laboratorian in charge, Clinical Laboratory, Binzhou City Hospital of Traditional Chinese Medicine, Binzhou 256613, Shandong Province, China
CLC Number:
Cite this article
Liu Ke-na, Li Dong, Yang Guang-sheng. 3D-cultured umbilical cord mesenchymal stem cells for treatment of type 1 diabetes: therapeutic effects and immunomodulatory mechanism[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(5): 692-697.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

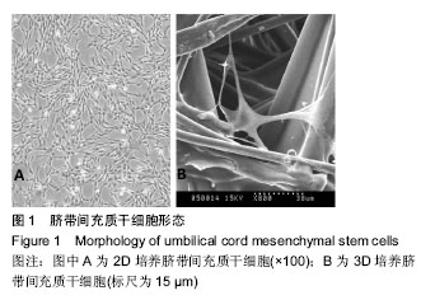
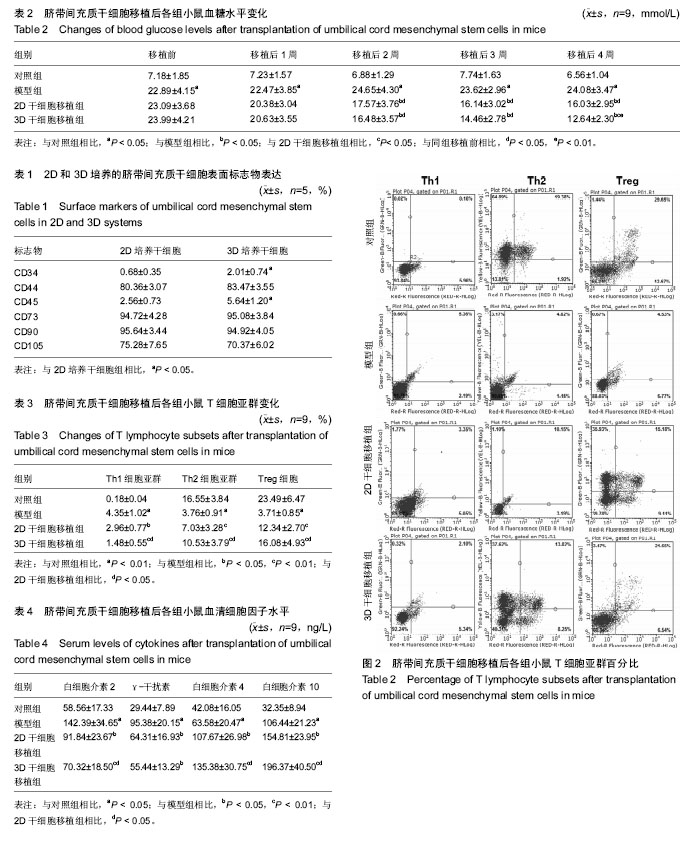
2.2 脐带间充干细胞表面标志物表达 流式细胞仪结果显示3D培养的脐带间充质干细胞表面标志物CD44、CD73、CD90和CD105呈高表达,CD34和CD45呈低表达,与2D培养的脐带间充质干细胞相比差异有显著性意义(P < 0.05),见表1。 2.3 各组小鼠血糖水平 模型组小鼠出现饮水量、尿量、进食量明显增加的现象,而且体毛无光泽,活动减少,体质量下降,说明造模成功。模型组与对照组相比,血糖明显升高,差异具有显著性意义(P < 0.05)。移植1周后,2D和3D干细胞移植组小鼠血糖与模型组相比差异不明显(P < 0.05),移植后2-4周,小鼠血糖水平下降明显,与模型组相比差异有显著性意义(P < 0.05)。3D干细胞移植组血糖水平从2周起低于2D干细胞移植组,4周出现显著性差异(P < 0.05),见表2。 2.4 各组小鼠T细胞亚群变化 流式细胞术检测各组小鼠T细胞亚群百分比,结果见表3和图2。模型组与对照组相比,Th1细胞亚群(CD4+IFNγ+)百分比明显升高(P < 0.01),Th2细胞亚群(CD4+IL-4+)和Treg细胞(CD4+CD25+)百分比均显著下降(P < 0.01)。2D和3D干细胞移植组与模型组相比,Th1细胞亚群百分比明显降低(P < 0.05),Th2细胞亚群和Treg细胞百分比均显著升高(P < 0.01),说明脐带间充质干细胞可以上调糖尿病小鼠的Treg细胞表达。3D干细胞移植组与2D干细胞移植组相比,Th1细胞亚群百分比降低,Th2细胞亚群和Treg细胞百分比明显升高(P < 0.05)。 2.5 各组小鼠血清细胞因子水平 如表4所示,模型组与对照组相比,白细胞介素2、γ-干扰素、白细胞介素4和白细胞介素10的表达水平均显著升高,差异有显著性意义(P < 0.05)。2D和3D干细胞移植组Th1型细胞因子白细胞介素2和γ-干扰素的表达水平与模型组相比显著降低,而Th2型细胞因子白细胞介素4和白细胞介素10的表达水平显著升高,差异有显著性意义(P < 0.05)。3D干细胞移植组与2D干细胞移植组相比,白细胞介素2表达水平显著降低,白细胞介素4和白细胞介素10的表达水平显著升高(P < 0.05),γ-干扰素的变化不明显。"
| [1] Handorf AM, Sollinger HW, Alam T. Insulin gene therapy for type 1 diabetes mellitus. Exp Clin Transplant. 2015;13 Suppl 1:37-45.[2] Morgan E, Halliday SR, Campbell GR, et al. Vaccinations and childhood type 1 diabetes mellitus: a meta-analysis of observational studies. Diabetologia. 2016;59(2):237-243.[3] American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27 Suppl 1:S5-S10.[4] 郝永蕾,朱旅云,王更银,等.体外诱导人脐带间充质干细胞分化为胰岛样细胞实验研究[J].临床误诊误治,2010,23(9):804-807.[5] 申义,王意忠,时瀚,等.人脐带间充质干细胞分化胰岛样细胞过程中胰岛素和巢蛋白的表达[J].中国组织工程研究, 2016,20(50): 7500-7506.[6] Aguayo-Mazzucato C, Bonner-Weir S. Stem cell therapy for type 1 diabetes mellitus. Nat Rev Endocrinol. 2010;6(3):139-148.[7] Hu J, Yu X, Wang Z, et al. Long term effects of the implantation of Wharton's jelly-derived mesenchymal stem cells from the umbilical cord for newly-onset type 1 diabetes mellitus. Endocr J. 2013;60(3):347-357.[8] 贾晓蕾,沈山梅,李莉蓉,等. 异体间充质干细胞移植治疗酮症起病1型糖尿病的临床疗效[J].中华糖尿病杂志, 2015, 7(7):425-430.[9] He B, Li X, Yu H, et al. Therapeutic potential of umbilical cord blood cells for type 1 diabetes mellitus. J Diabetes. 2015;7(6): 762-773.[10] Liu S, Yuan M, Hou K, et al. Immune characterization of mesenchymal stem cells in human umbilical cord Wharton's jelly and derived cartilage cells. Cell Immunol. 2012;278(1-2):35-44. [11] Yang H, Sun J, Li Y, et al. Human umbilical cord-derived mesenchymal stem cells suppress proliferation of PHA-activated lymphocytes in vitro by inducing CD4(+)CD25(high)CD45RA(+) regulatory T cell production and modulating cytokine secretion. Cell Immunol. 2016;302:26-31. [12] Vellasamy S, Sandrasaigaran P, Vidyadaran S, et al. Mesenchymal stem cells of human placenta and umbilical cord suppress T-cell proliferation at G0 phase of cell cycle. Cell Biol Int. 2013;37(3):250-256.[13] Braghirolli DI, Zamboni F, Acasigua GA, et al. Association of electrospinning with electrospraying: a strategy to produce 3D scaffolds with incorporated stem cells for use in tissue engineering. Int J Nanomedicine. 2015;10:5159-5169.[14] González S, Mei H, Nakatsu MN, et al. A 3D culture system enhances the ability of human bone marrow stromal cells to support the growth of limbal stem/progenitor cells. Stem Cell Res. 2016;16(2):358-364.[15] Rath SN, Nooeaid P, Arkudas A, et al. Adipose- and bone marrow-derived mesenchymal stem cells display different osteogenic differentiation patterns in 3D bioactive glass-based scaffolds. J Tissue Eng Regen Med. 2016;10(10):E497-E509.[16] Griffith LG, Swartz MA. Capturing complex 3D tissue physiology in vitro. Nat Rev Mol Cell Biol. 2006;7(3):211-224.[17] Ferlin KM, Prendergast ME, Miller ML, et al. Influence of 3D printed porous architecture on mesenchymal stem cell enrichment and differentiation. Acta Biomater. 2016;32:161-169.[18] Li SL, Liu Y, Hui L. Construction of engineering adipose-like tissue in vivo utilizing human insulin gene-modified umbilical cord mesenchymal stromal cells with silk fibroin 3D scaffolds. J Tissue Eng Regen Med. 2015;9(12):E267-275.[19] Qin Y, He YH, Hou N, et al. Sonic hedgehog improves ischemia-induced neovascularization by enhancing endothelial progenitor cell function in type 1 diabetes. Mol Cell Endocrinol. 2016;423:30-39.[20] Colomeu TC, Figueiredo D, Cazarin CB, et al. Antioxidant and anti-diabetic potential of Passiflora alata Curtis aqueous leaves extract in type 1 diabetes mellitus (NOD-mice). Int Immunopharmacol. 2014;18(1):106-115.[21] Grisé KN, Olver TD, McDonald MW, et al. High Intensity Aerobic Exercise Training Improves Deficits of Cardiovascular Autonomic Function in a Rat Model of Type 1 Diabetes Mellitus with Moderate Hyperglycemia. J Diabetes Res. 2016;2016: 8164518. [22] 付清松, 夏玉军, 张明, 等. 三维球体间充质干细胞移植对大鼠缺血再灌注损伤脑组织TNF-α及凋亡相关蛋白表达的影响[J].第二军医大学学报, 2015,36(8):845-850.[23] Antebi B, Zhang Z, Wang Y, et al. Stromal-cell-derived extracellular matrix promotes the proliferation and retains the osteogenic differentiation capacity of mesenchymal stem cells on three-dimensional scaffolds. Tissue Eng Part C Methods. 2015;21(2):171-181. [24] Occhetta P, Centola M, Tonnarelli B, et al. High-Throughput Microfluidic Platform for 3D Cultures of Mesenchymal Stem Cells, Towards Engineering Developmental Processes. Sci Rep. 2015;5:10288.[25] Papadimitropoulos A, Piccinini E, Brachat S, et al. Expansion of human mesenchymal stromal cells from fresh bone marrow in a 3D scaffold-based system under direct perfusion. PLoS One. 2014;9(7):e102359.[26] Caron I, Rossi F, Papa S, et al. A new three dimensional biomimetic hydrogel to deliver factors secreted by human mesenchymal stem cells in spinal cord injury. Biomaterials. 2016;75:135-147.[27] Li Y, Guo G, Li L, et al. Three-dimensional spheroid culture of human umbilical cord mesenchymal stem cells promotes cell yield and stemness maintenance. Cell Tissue Res. 2015; 360(2):297-307.[28] Rodina AV, Tenchurin TK, Saprykin VP, et al. Migration and Proliferative Activity of Mesenchymal Stem Cells in 3D Polylactide Scaffolds Depends on Cell Seeding Technique and Collagen Modification. Bull Exp Biol Med. 2016;162(1):120-126. [29] Zheng Z, Shen W, Le H, et al. Three-dimensional parallel collagen scaffold promotes tendon extracellular matrix formation. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2016;45(2):120-125.[30] Shami A, Gonçalves I, Hultgårdh-Nilsson A. Collagen and related extracellular matrix proteins in atherosclerotic plaque development. Curr Opin Lipidol. 2014;25(5):394-399.[31] 刘锐,刘畅,殷甜甜. 三维培养下化学方法诱导肌源性干细胞向胰岛素分泌细胞分化的研究[J]. 辽宁医学学报, 2016,37(1):4-7.[32] Zhang Y, Zhang Y, Gu W, et al. TH1/TH2 cell differentiation and molecular signals. Adv Exp Med Biol. 2014;841:15-44.[33] Perez-Mazliah D, Langhorne J. CD4 T-cell subsets in malaria: TH1/TH2 revisited. Front Immunol. 2015;5:671.[34] Matsuzaki J, Tsuji T, Imazeki I, et al. Immunosteroid as a regulator for Th1/Th2 balance: its possible role in autoimmune diseases.Autoimmunity. 2005;38(5):369-375.[35] Raz I, Eldor R, Naparstek Y. et al. Immune modulation for prevention of type 1 diabetes mellitus.Trends Biotechnol. 2005;23(3):128-134.[36] Heurtier AH, Boitard C.T-cell regulation in murine and human autoimmune diabetes: the role of TH1 and TH2 cells. Diabetes Metab. 1997;23(5):377-385.[37] Haritha C, Shankar V, Trivedi HL, et al. Mesenchymal Stem Cells Transplantation with Non-myeloablative Conditioning for Type I Diabetes Mellitus : Lab to Clinic. International Journal of Radiation Oncology Biology Physics. 2009; 75(3) :S486-S487.[38] Masteller EL, Tang Q, Bluestone JA. Antigen-specific regulatory T cells--ex vivo expansion and therapeutic potential. Semin Immunol. 2006;18(2):103-110.[39] Tan T, Xiang Y, Chang C, et al. Alteration of regulatory T cells in type 1 diabetes mellitus: a comprehensive review. Clin Rev Allergy Immunol. 2014;47(2):234-243.[40] Lee RH, Seo MJ, Reger RL, et al. Multipotent stromal cells from human marrow home to and promote repair of pancreatic islets and renal glomeruli in diabetic NOD/scid mice.Proc Natl Acad Sci U S A. 2006;103(46):17438-17443. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [3] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [4] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [5] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [6] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [7] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [8] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [9] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [10] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [11] | Gao Shan, Huang Dongjing, Hong Haiman, Jia Jingqiao, Meng Fei. Comparison on the curative effect of human placenta-derived mesenchymal stem cells and induced islet-like cells in gestational diabetes mellitus rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3981-3987. |
| [12] | Ruan Guangping, Yao Xiang, Liu-Gao Miyang, Cai Xuemin, Li Zian, Pang Rongqing, Wang Jinxiang, Pan Xinghua. Umbilical cord mesenchymal stem cell transplantation for traumatic systemic inflammatory response syndrome in tree shrews [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(25): 3994-4000. |
| [13] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [14] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| [15] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||