Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (2): 231-236.doi: 10.12307/2023.859
Previous Articles Next Articles
Effects of treadmill exercise on osteoporosis and wnt/beta-catenin signal pathway in aged rats
Yin Linwei1, 2, 3, Huang Xiarong1, 2, 3, Qu Mengjian1, 2, 3, Yang Lu1, 2, 3, Wang Jinling1, 2, 3, Jia Feiyang1, 2, 3, Liao Yang1, 2, 3, Zhou Jun1, 2, 3, 4
- 1Department of Rehabilitation, 2Rehabilitation Medicine Center, 3Rehabilitation Laboratory, the First Affiliated Hospital of Hengyang Medical School, University of South China, Hengyang 421001, Hunan Province, China; 4Key Laboratory of Rehabilitation Medicine, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China
-
Received:2022-10-09Accepted:2022-12-15Online:2024-01-18Published:2023-06-30 -
Contact:Zhou Jun, MD, Chief physician, Department of Rehabilitation, Rehabilitation Medicine Center, Rehabilitation Laboratory, the First Affiliated Hospital of Hengyang Medical School, University of South China, Hengyang 421001, Hunan Province, China; Key Laboratory of Rehabilitation Medicine, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China -
About author:Yin Linwei, Therapist in charge, Department of Rehabilitation, Rehabilitation Medicine Center, Rehabilitation Laboratory, the First Affiliated Hospital of Hengyang Medical School, University of South China, Hengyang 421001, Hunan Province, China -
Supported by:National Natural Science Foundation of China (General Program), No. 81973917 (to ZJ); Hunan Provincial Health Commission Key Project, No. 202103060198 (to ZJ); School-level Key Project of the University of South China, No. USCKF201902K02 (to ZJ)
CLC Number:
Cite this article
Yin Linwei, Huang Xiarong, Qu Mengjian, Yang Lu, Wang Jinling, Jia Feiyang, Liao Yang, Zhou Jun. Effects of treadmill exercise on osteoporosis and wnt/beta-catenin signal pathway in aged rats[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 231-236.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
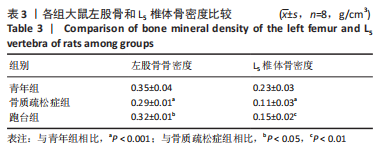
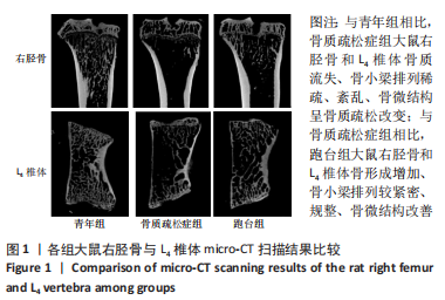
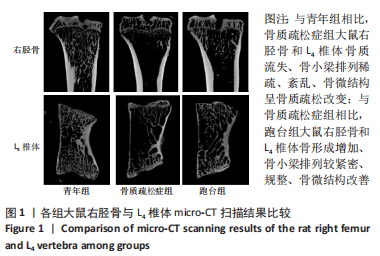
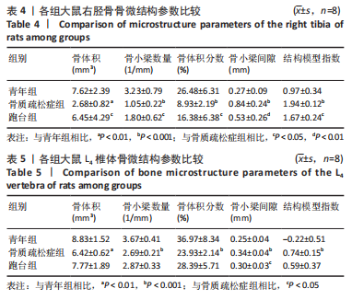
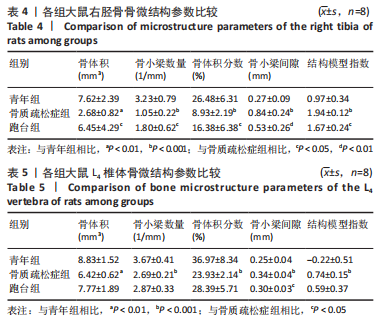
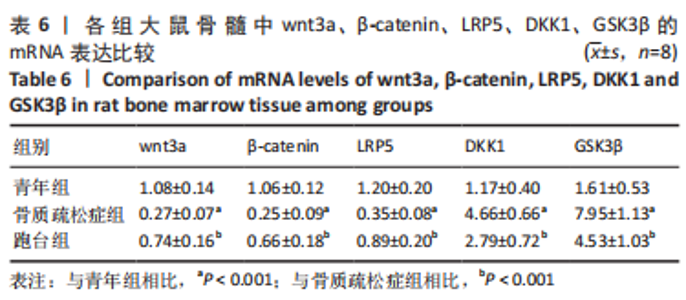
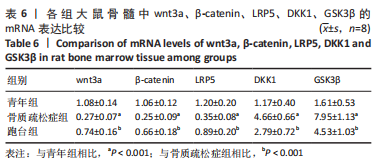
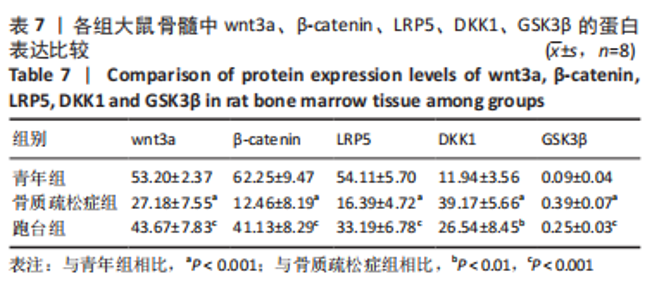
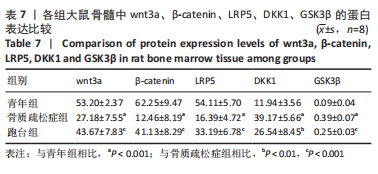
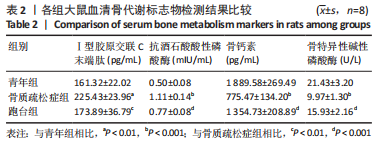
2.1 实验动物数量分析 24只大鼠全部进入结果分析。 2.2 各组大鼠血清骨代谢标志物水平的比较 血清骨形成与骨吸收标志物检测结果显示,老年大鼠骨形成减少、骨吸收增加,打破了骨形成与骨吸收之间的平衡,而跑台运动可以通过增加骨形成、减少骨吸收,调节骨失衡。 与青年组相比,骨质疏松症组大鼠血清Ⅰ型胶原交联C末端肽、抗酒石酸酸性磷酸酶水平显著升高(P < 0.01,P < 0.001),骨钙素、骨特异性碱性磷酸酶水平显著降低(P < 0.001)。与骨质疏松症组相比,跑台组大鼠血清Ⅰ型胶原交联C末端肽、抗酒石酸酸性磷酸酶水平显著降低(P < 0.01,P < 0.001),骨钙素、骨特异性碱性磷酸酶水平显著升高(P < 0.001),见表2。"
| [1] 章振林,金小岚,夏维波.原发性骨质疏松症诊疗指南(2017版)要点解读[J].中华骨质疏松和骨矿盐疾病杂志,2017,10(5):411-412. [2] 赵宗权,吴贻红,汤振源,等.老年骨质疏松症流行病学调查及预防措施研究[J].中国骨质疏松杂志,2019,25(7):994-997. [3] 中华医学会骨质疏松和骨矿盐疾病分会.中国骨质疏松症流行病学调查及“健康骨骼”专项行动结果发布[J].中华骨质疏松和骨矿盐疾病杂志,2019, 12(4):317-318. [4] 朱洁云,高敏,宋秋韵,等.中国老年人骨质疏松症患病率的 Meta 分析[J].中国全科医学,2022,25(3):346-353. [5] 谈志龙,任海龙,白人骁,等.骨质疏松症与骨代谢生化测定指标[J].中国骨质疏松杂志,2006,12(1):89-93. [6] DENG Q, LI P, CHE M, et al. Activation of hedgehog signaling in mesenchymal stem cells induces cartilage and bone tumor formation via Wnt/β-Catenin. Elife. 2019;8:e50208. [7] 郭强,于冬冬.基于代谢组学技术探讨中医药防治骨质疏松症的研究进展[J].广西中医药,2022,45(5):67-70. [8] 谢宝辉,罗礼亮,巫远华.阿仑膦酸钠联合中药及理疗治疗骨质疏松症的临床效果[J].中国当代医药,2020,27(15):100-102. [9] 佟喆,张振南,于潼.运动疗法防治骨质疏松症机制的研究进展[J].中国骨质疏松杂志,2022,28(10):1556-1560. [10] CHEN X, LI L, GUO J, et al. Treadmill running exercise prevents senile osteoporosis and upregulates the Wnt signaling pathway in SAMP6 mice. Oncotarget. 2016; 7(44):71072-71086. [11] LIU DB, SUI C, WU TT, et al. Association of Bone Morphogenetic Protein (BMP)/Smad Signaling Pathway with Fracture Healing and Osteogenic Ability in Senile Osteoporotic Fracture in Humans and Rats. Med Sci Monit. 2018;24:4363-4371. [12] XUN J, LI C, LIU M, et al. Serum exosomes from young rats improve the reduced osteogenic differentiation of BMSCs in aged rats with osteoporosis after fatigue loading in vivo. Stem Cell Res Ther. 2021;12(1):424. [13] MA S, QIN J, HAO Y, et al. Association of gut microbiota composition and function with an aged rat model of senile osteoporosis using 16S rRNA and metagenomic sequencing analysis. Aging. 2020;12(11):10795-10808. [14] DURDAN MM, AZARIA RD, WEIVODA MM. Novel insights into the coupling of osteoclasts and resorption to bone formation. Semin Cell Dev Biol. 2022;123:4-13. [15] WALKER EC, MCGREGOR NE, POULTON IJ, et al. Oncostatin M promotes bone formation independently of resorption when signaling through leukemia inhibitory factor receptor in mice. J Clin Invest. 2010;120(2):582-592. [16] CHANDRA A, RAJAWAT J. Skeletal Aging and Osteoporosis: Mechanisms and Therapeutics. Int J Mol Sci. 2021;22(7):3553. [17] KHOSLA S, FARR JN, MONROE DG. Cellular senescence and the skeleton: pathophysiology and therapeutic implications. J Clin Invest. 2022;132(3):e154888. [18] IVASKA KK, MCGUIGAN FE, MALMGREN L, et al. Bone Turnover Marker Profiling and Fracture Risk in Older Women: Fracture Risk from Age 75 to 90. Calcif Tissue Int. 2022. doi:10.1007/s00223-022-00996-8. [19] NIIMI R, CHIBA K, OKAZAKI N, et al. Relationships between QUS and HR-pQCT, DXA, and bone turnover markers. J Bone Miner Metab, 2022.doi:10.1007/s00774-022-01346-2. [20] ATALAY S, ELCI A, KAYADIBI H, et al. Diagnostic utility of osteocalcin, undercarboxylated osteocalcin, and alkaline phosphatase for osteoporosis in premenopausal and postmenopausal women. Ann Lab Med. 2012;32(1):23-30. [21] REMPE J, ROSENGREN BE, JEHPSSON L, et al. Physical Activity in Late Prepuberty and Early Puberty Is Associated With High Bone Formation and Low Bone Resorption. Front Physiol. 2022;13:828508. [22] BUCK DW 2ND, DUMANIAN GA. Bone biology and physiology: Part II. Clinical correlates. Plast Reconstr Surg. 2012;129(6):950e-956e. [23] COOPER LF, MASUDA T, YLIHEIKKILÄ PK, et al. Generalizations regarding the process and phenomenon of osseointegration. Part II. In vitro studies. Int J Oral Maxillofac Implants. 1998;13(2):163-174. [24] BUCK DW 2ND, DUMANIAN GA. Bone biology and physiology: Part I. The fundamentals. Plast Reconstr Surg. 2012;129(6):1314-1320. [25] VASIKARAN SD, MIURA M, PIKNER R, et al. Practical Considerations for the Clinical Application of Bone Turnover Markers in Osteoporosis. Calcif Tissue Int. 2023;112(2):148-157. [26] ANAM AK, INSOGNA K. Update on Osteoporosis Screening and Management. Med Clin North Am. 2021;105(6):1117-1134. [27] SHEVROJA E, CAFARELLI FP, GUGLIELMI G, et al. DXA parameters, Trabecular Bone Score (TBS) and Bone Mineral Density (BMD), in fracture risk prediction in endocrine-mediated secondary osteoporosis. Endocrine. 2021;74(1):20-28. [28] KANAZAWA M, MATSUMOTO Y, TAKAHASHI K, et al. Treadmill exercise prevents reduction of bone mineral density after myocardial infarction in apolipoprotein E-deficient mice. Eur J Prev Cardiol. 2020;27(1):28-35. [29] GAO L, LI Y, YANG YJ, et al. The Effect of Moderate-Intensity Treadmill Exercise on Bone Mass and the Transcription of Peripheral Blood Mononuclear Cells in Ovariectomized Rats. Front Physiol. 2021;12:729910. [30] LIU J, XIAO Q, XIAO J, et al. Wnt/β-catenin signalling: function, biological mechanisms, and therapeutic opportunities. Signal Transduct Target Ther. 2022;7(1):3. [31] YUAN X, LIU H, HUANG H, et al. The Key Role of Canonical Wnt/β-catenin Signaling in Cartilage Chondrocytes. Curr Drug Targets. 2016;17(4):475-484. [32] BARTOLETTI G, DONG C, UMAR M, et al. Pdgfra regulates multipotent cell differentiation towards chondrocytes via inhibiting Wnt9a/beta-catenin pathway during chondrocranial cartilage development. Dev Biol. 2020;466(1-2):36-46. [33] JING Y, JING J, WANG K, et al. Vital Roles of β-catenin in Trans-differentiation of Chondrocytes to Bone Cells. Int J Biol Sci. 2018;14(1):1-9. [34] CHAN BY, LITTLE CB. The interaction of canonical bone morphogenetic protein- and Wnt-signaling pathways may play an important role in regulating cartilage degradation in osteoarthritis. Arthritis Res Ther. 2012;14(3):119. [35] SPENCER GJ, UTTING JC, ETHERIDGE SL, et al. Wnt signalling in osteoblasts regulates expression of the receptor activator of NFkappaB ligand and inhibits osteoclastogenesis in vitro. J Cell Sci. 2006;119(Pt 7):1283-1296. [36] ROSSINI M, GATTI D, ADAMI S. Involvement of WNT/β-catenin signaling in the treatment of osteoporosis. Calcif Tissue Int. 2013;93(2):121-132. [37] LETTINI G, CONDELLI V, PIETRAFESA M, et al. TRAP1 Regulates Wnt/β-Catenin Pathway through LRP5/6 Receptors Expression Modulation. Int J Mol Sci. 2020;21(20):7526. [38] HUANG Y, LIU L, LIU A. Dickkopf-1: Current knowledge and related diseases. Life Sci. 2018;209:249-254. [39] CHIARITO M, PIACENTE L, CHAOUL N, et al. Role of Wnt-signaling inhibitors DKK-1 and sclerostin in bone fragility associated with Turner syndrome. J Endocrinol Invest. 2022;45(6):1255-1263. [40] ZHANG Y, SHI T, HE Y. GPR35 regulates osteogenesis via the Wnt/GSK3β/β-catenin signaling pathway. Biochem Biophys Res Commun. 2021;556:171-178. [41] KARIM K, GIRIBABU N, SALLEH N. Marantodes pumilum (blume) Kuntze (Kacip Fatimah) leaves aqueous extract prevents downregulation of Wnt/β-catenin pathway and upregulation of apoptosis in osteoblasts of estrogen-deficient, diabetes-induced rats. J Ethnopharmacol. 2021;280:114236. [42] LIANG L, TU Y, LU J, et al. Dkk1 exacerbates doxorubicin-induced cardiotoxicity by inhibiting the Wnt/β-catenin signaling pathway. J Cell Sci. 2019;132(10):jcs228478. [43] LAW SM, ZHENG JJ. Premise and peril of Wnt signaling activation through GSK-3β inhibition. iScience. 2022;25(4):104159. [44] MAROSI M, ARMAN P, ACETO G, et al. Glycogen Synthase Kinase 3: Ion Channels, Plasticity, and Diseases. Int J Mol Sci. 2022;23(8):4413. [45] BARON R, KNEISSEL M. WNT signaling in bone homeostasis and disease: from human mutations to treatments. Nat Med. 2013;19(2):179-192. [46] ZHAO SJ, KONG Q, JIE J, et al. Macrophage MSR1 promotes BMSC osteogenic differentiation and M2-like polarization by activating PI3K/AKT/GSK3β/β-catenin pathway. Theranostics. 2020;10(1):17-35. [47] LARA-CASTILLO N, JOHNSON ML. LRP receptor family member associated bone disease. Rev Endocr Metab Disord. 2015;16(2):141-148. [48] SANTOS L, UGUN-KLUSEK A, COVENEY C, et al. Multiomic analysis of stretched osteocytes reveals processes and signalling linked to bone regeneration and cancer. NPJ Regen Med. 2021;6(1):32. [49] MOVéRARE-SKRTIC S, HENNING P, LIU X, et al. Osteoblast-derived WNT16 represses osteoclastogenesis and prevents cortical bone fragility fractures. Nat Med. 2014;20(11):1279-1288. [50] TONG X, CHEN X, ZHANG S, et al. The Effect of Exercise on the Prevention of Osteoporosis and Bone Angiogenesis. Biomed Res Int. 2019;2019:8171897. |
| [1] | He Lijun, Qi Xiaojuan. Adipose-derived mesenchymal stem cells overexpressing bone morphogenetic protein 2 promote alveolar bone defect repair in osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(1): 32-37. |
| [2] | Li Xiaomin, Tian Xiangdong, Tan Yetong, Zhu Guangyu, Wang Rongtian, Wang Jian, Xue Zhipeng, Ma Sheng, Hu Yuanyi, Huang Ye, Ding Tiansong. Changes of lower limb force line and knee function after high tibial osteotomy in osteoporotic medial ventricular knee osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1325-1329. |
| [3] | Jiang Xiaocheng, Shi Lu, Wang Yinbin, Li Qiujiang, Xi Chuangzhen, Ma Zefeng, Cai Lijun. Systematical evaluation of bone fusion rate after interbody fusion in patients with osteoporosis and lumbar degenerative disease treated with teriparatide [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1427-1433. |
| [4] | Sun Jiajia, Zhu Haidi, Lu Yun, Zhang Kai. Comparison of bone metabolism markers between type 2 diabetes mellitus and non-type 2 diabetes mellitus patients with hip fracture [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1156-1160. |
| [5] | Huang Linke, Wei Linhua, Jiang Jie, Liu Qian, Chen Weiwei. Effects of estrogen combined with treadmill exercise on bone mass and articular cartilage in ovariectomized mice [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1166-1171. |
| [6] | Long Yanming, Xie Mengsheng, Huang Jiajie, Xue Wenli, Rong Hui, Li Xiaojie. Casein kinase 2-interaction protein-1 regulates the osteogenic ability of bone marrow mesenchymal stem cells in osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 878-882. |
| [7] | Zhang Min, Zhang Xiaoming, Liu Tongbin. Application potential of naringin in bone tissue regeneration [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 787-792. |
| [8] | Wang Jinling, Huang Xiarong, Qu Mengjian, Huang Fujin, Yin Lingwei, Zhong Peirui, Liu Jin, Sun Guanghua, Liao Yang, Zhou Jun. Effects of exercise training on bone mass and bone microstructure in aged osteoporotic rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(5): 676-682. |
| [9] | Cheng Yunzhong, Liu Yuzeng, Hai Yong, Guan Li, Pan Aixing, Zhang Xinuo, Tao Luming, Li Yue. Bibliometric and visual analysis of the research status and development trend of cortical bone trajectory screws [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 513-519. |
| [10] | Liu Hao, Yang Hongsheng, Zeng Zhimou, Wang Liping, Yang Kunhai, Hu Yongrong, Qu Bo. Lumbar MRI vertebral bone quality score to evaluate the severity of osteoporosis in postmenopausal women [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 606-611. |
| [11] | Wu Minhui, Tang Changye, Dai Yuexing, Zheng Liqin, Li Zhihong, Li Shaobin, Lin Ziling. Difference in mechanical properties of osteoporotic bone trabecular 3D models with different gray thresholds [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(36): 5766-5770. |
| [12] | Qian Guang, Yu Yueming, Dong Youhai, Hong Yang, Wang Minghai. Serum pentosidine level and trabecular bone score affect the severity of vertebral fractures in type 2 diabetes patients [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(36): 5870-5874. |
| [13] | Zhang Chi, Zhang Xiaoyun, Chai Yuan, Chen Feng. Proteomic study of Jintiange capsule in the treatment of retinoic acid-induced osteoporosis rats [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(35): 5634-5641. |
| [14] | Liu Jin, Xia Bin, Cai Peng, Gu Zuchao, Yang Haosen, Tang Jing. Effect of vertebral augmentation using quantitative computed tomography-based finite element analysis on biomechanical parameters of non-enhanced vertebrae in different locations [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(34): 5436-5440. |
| [15] | Li Jiarui, Yan Yang, Wu Xiaogang, Feng Haoyu, He Liming. Biomechanical analysis of unilateral biportal endoscopic lumbar interbody fusion [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(34): 5523-5529. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||