[1] NEOGI T, ZHANG Y. Epidemiology of osteoarthritis. Rheum Dis Clin North Am. 2013;39(1):1-19.
[2] 周帅琪,梁龙,于杰,等.最新膝骨关节炎循证国际指南纵览[J].海南医学院学报,2020,26(5):388-391.
[3] BIJLSMA JW, BERENBAUM F, LAFEBER FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115-2126.
[4] PALEY D, PFEIL J. Principles of deformity correction around the knee. Orthopade. 2000;29(1):18-38.
[5] ZENG YM, WANG Y, ZHU ZA, et al. Effects of sex and lower extremity alignment on orientation of the knee joint line in knee surgery. Chin Med J (Engl). 2012;125(12):2126-2131.
[6] FLOERKEMEIER S, STAUBLI AE, SCHROETER S, et al. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):170-180.
[7] 于沂阳, 常恒瑞, 张英泽. 保膝治疗的研究进展[J]. 中华关节外科杂志(电子版),2017,11(1):73-77.
[8] DA SH, ZORZI AR, DA SH, et al. Gait analysis in short-term follow-up of medial opening wedge high tibial osteotomy. Eur J Orthop Surg Traumatol. 2018;28(5):939-946.
[9] 郭浩山,田义军,安龙,等.关节镜联合腓骨近端截骨术与胫骨高位截骨术治疗膝内侧间室骨性关节炎的疗效比较[J].中国骨与关节损伤杂志,2020,35(10):1076-1078.
[10] BITO H, TAKEUCHI R, KUMAGAI K, et al. Opening wedge high tibial osteotomy affects both the lateral patellar tilt and patellar height. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):955-960.
[11] 陈百成,高石军,王晓峰,等.胫骨高位截骨术后髌骨低位[J].中华骨科杂志,2003,23(8):4-6.
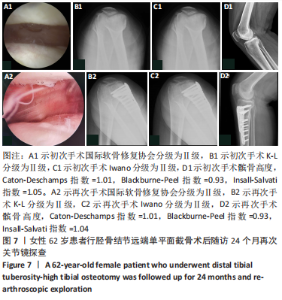
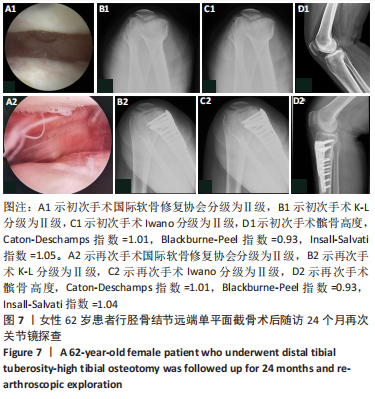
[12] 韩昶晓, 田向东, 王剑, 等. 胫骨结节远端单平面截骨术对髌骨高度的影响[J]. 中华关节外科杂志(电子版),2020,14(5):559-564.
[13] IWANO T, KUROSAWA H, TOKUYAMA H, et al. Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res. 1990(252):190-197.
[14] 张英泽, 李存祥, 李冀东, 等. 不均匀沉降在膝关节退变及内翻过程中机制的研究[J]. 河北医科大学学报,2014,35(2):218-219.
[15] 汪瑞东, 白金广, 李冬梅, 等. 胫骨高位截骨术治疗膝内侧骨性关节炎的体会[J]. 中国骨与关节损伤杂志,2021,36(10):1080-1082.
[16] JACKSON J P, WAUGH W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43-B:746-751.
[17] 许健,郭标,马炜,等.胫骨内侧高位截骨术中Miniaci法与力线杆定位法矫正下肢负重力线的精确性比较[J].中国骨与关节损伤杂志,2020,35(6):577-580.
[18] CHIEH-SZU YJ, CHEN CF, LEE OK. Benefits of opposite screw insertion technique in medial open-wedge high tibial osteotomy: A virtual biomechanical study. J Orthop Translat. 2020;20:31-36.
[19] OHSAWA S, HUKUDA K, INAMORI Y, et al. High tibial osteotomy for osteoarthritis of the knee with varus deformity utilizing the hemicallotasis method. Arch Orthop Trauma Surg. 2006;126(9):588-593.
[20] FERNER F, LUTTER C, DICKSCHAS J, et al. Medial open wedge vs. lateral closed wedge high tibial osteotomy - Indications based on the findings of patellar height, leg length, torsional correction and clinical outcome in one hundred cases. Int Orthop. 2019;43(6):1379-1386.
[21] JAVIDAN P, ADAMSON GJ, MILLER JR, et al. The effect of medial opening wedge proximal tibial osteotomy on patellofemoral contact. Am J Sports Med. 2013;41(1):80-86.
[22] YANG JH, LEE SH, NATHAWAT KS, et al. The effect of biplane medial opening wedge high tibial osteotomy on patellofemoral joint indices. Knee. 2013;20(2):128-132.
[23] BIN SI, KIM HJ, AHN HS, et al. Changes in Patellar Height After Opening Wedge and Closing Wedge High Tibial Osteotomy: A Meta-analysis. Arthroscopy. 2016;32(11):2393-2400.
[24] GOSHIMA K, SAWAGUCHI T, SHIGEMOTO K, et al. Patellofemoral Osteoarthritis Progression and Alignment Changes after Open-Wedge High Tibial Osteotomy Do Not Affect Clinical Outcomes at Mid-term Follow-up. Arthroscopy. 2017;33(10):1832-1839.
[25] 李珂,孙凤龙,王宏庆,等.改良单平面胫骨高位截骨术治疗膝关节骨关节炎的早期临床研究[J].中华骨与关节外科杂志,2020, 13(9):729-735.
[26] 周观明,刘效仿,管明强,等.改良内侧开放式胫骨高位截骨术治疗膝内侧间室骨性关节炎[J].组织工程与重建外科,2021,17(1):54-56.
[27] DENG X, CHEN W, ZHAO K, et al. Changes in patellar height and posterior tibial slope angle following uniplanar medial opening wedge high tibial osteotomy using a novel wedge-shaped spacer implanation concurrent with proximal partial fibulectomy. Int Orthop. 2021;45(1):109-115.
[28] AKIYAMA T, OSANO K, MIZU-UCHI H, et al. Distal Tibial Tuberosity Arc Osteotomy in Open-Wedge Proximal Tibial Osteotomy to Prevent Patella Infra. Arthrosc Tech. 2019;8(6):e655-e662.
[29] HAN C, LI X, TIAN X, et al. The effect of distal tibial tuberosity high tibial osteotomy on postoperative patellar height and patellofemoral joint degeneration. J Orthop Surg Res. 2020;15(1):466.
[30] 许康永,童也,赵鹏,等.两种截骨术式治疗膝关节内侧间室骨关节炎的疗效比较[J].中国修复重建外科杂志,2021,35(11):1440-1448.
|