Chinese Journal of Tissue Engineering Research ›› 2023, Vol. 27 ›› Issue (11): 1683-1691.doi: 10.12307/2023.127
Previous Articles Next Articles
Comparison of cerebral microcirculation perfusion in rat models of middle cerebral artery occlusion prepared through common carotid artery insertion and external carotid artery insertion
Li Yong, Yuan Jianmei, Lu Danni, Ren Mihong, Deng Bowen, Wang Jiajun, Ma Rong, Xie Qian, Li Jinxiu, Xu Zhuo, Wang Jian
- School of Pharmacy, Chengdu University of Traditional Chinese Medicine, Chengdu 611137, Sichuan Province, China
-
Received:2022-02-19Accepted:2022-04-23Online:2023-04-18Published:2022-09-26 -
Contact:Wang Jian, Professor, Doctoral supervisor, School of Pharmacy, Chengdu University of Traditional Chinese Medicine, Chengdu 611137, Sichuan Province, China -
About author:Li Yong, Master candidate, School of Pharmacy, Chengdu University of Traditional Chinese Medicine, Chengdu 611137, Sichuan Province, China -
Supported by:the National Natural Science Foundation of China (General Program), No. 81873023 (to WJ); the "Nature-Effect-Utilization" of Traditional Chinese Medicine (to WJ)
CLC Number:
Cite this article
Li Yong, Yuan Jianmei, Lu Danni, Ren Mihong, Deng Bowen, Wang Jiajun, Ma Rong, Xie Qian, Li Jinxiu, Xu Zhuo, Wang Jian. Comparison of cerebral microcirculation perfusion in rat models of middle cerebral artery occlusion prepared through common carotid artery insertion and external carotid artery insertion[J]. Chinese Journal of Tissue Engineering Research, 2023, 27(11): 1683-1691.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
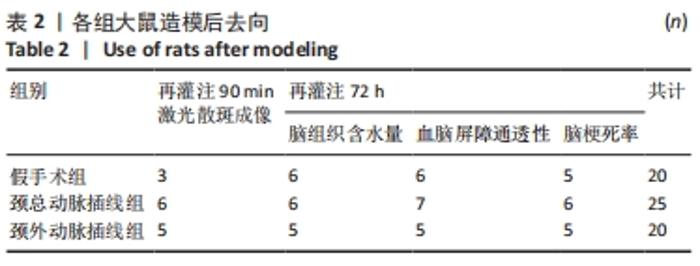
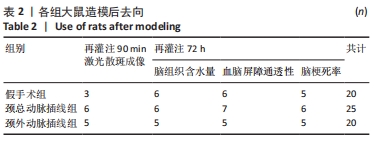
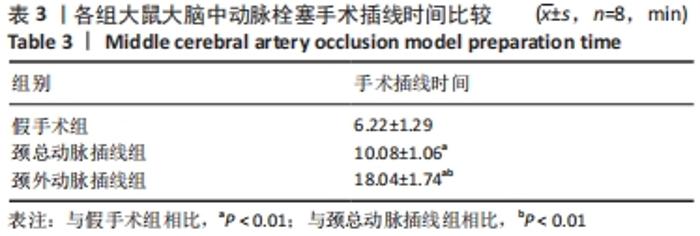
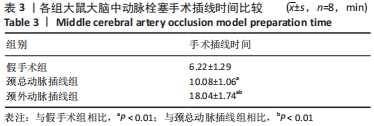
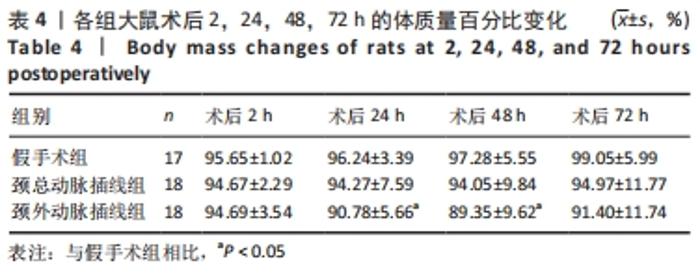
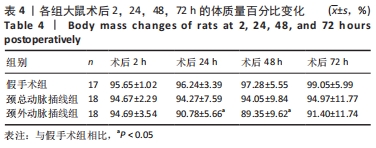
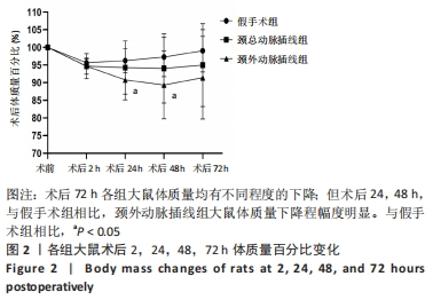
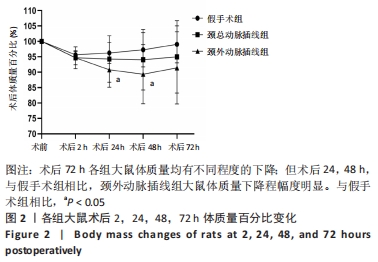
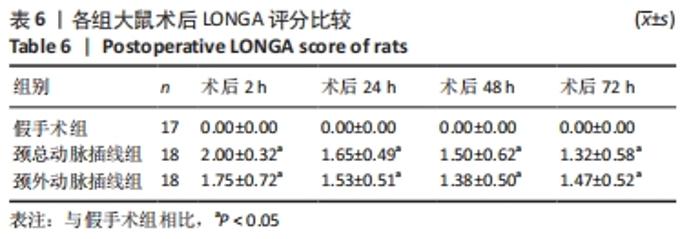
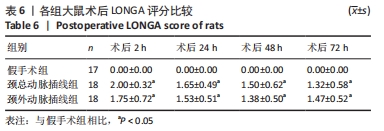
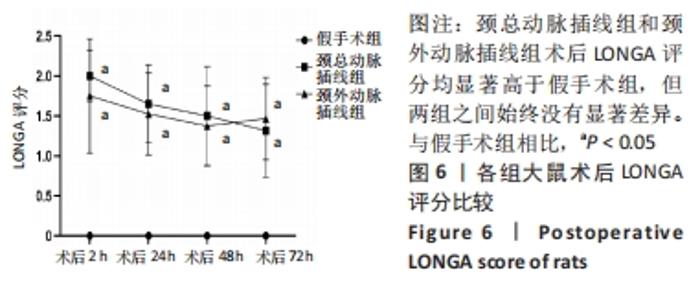
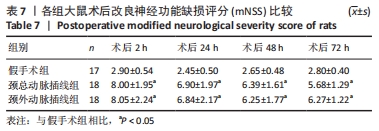
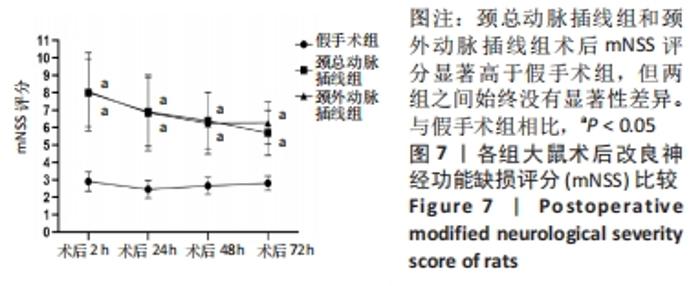
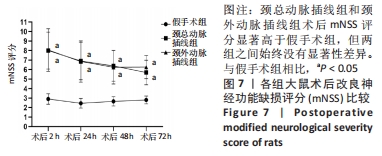
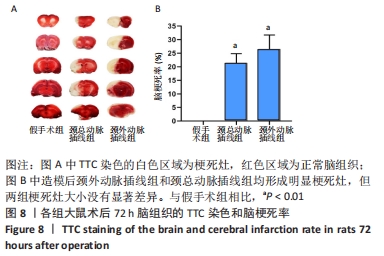
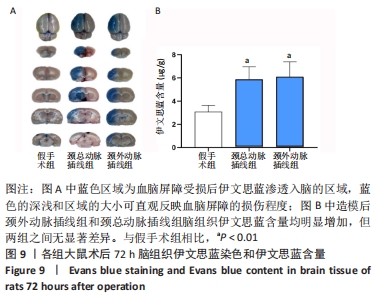
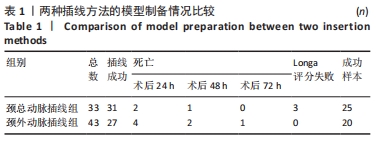
2.1 模型制备情况 颈总动脉插线组中31只大鼠插线成功,成功率为94%(31/33),颈外动脉插线组中有27只插线成功,成功率为63%(27/43),两组之间差异有显著性意义(P < 0.01)。颈总动脉插线组和颈外动脉插线组分别有3只和7只大鼠在术后72 h内由于蛛网膜下腔出血死亡,出血死亡率分别为10%(3/31)和30%(7/27),差异无显著性意义(P > 0.05)。根据Longa评分(评分为1-3分方可纳入后续实验),颈总动脉插线组和颈外动脉插线组分别有3只和0只大鼠被排除,差异无显著性意义(P > 0.05)。颈总动脉插线组和颈外动脉插线组最终成功的样本数量分别为25只和20只,模型成功率分别为76%(25/33)和46%(20/43),差异有显著性意义(P < 0.05)。各组大鼠模型制备情况见表1。"
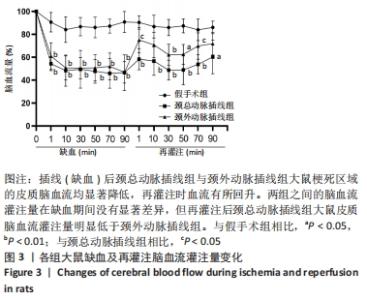
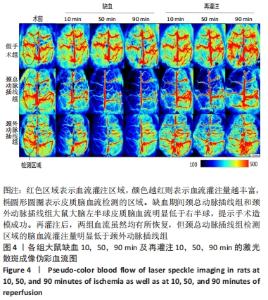
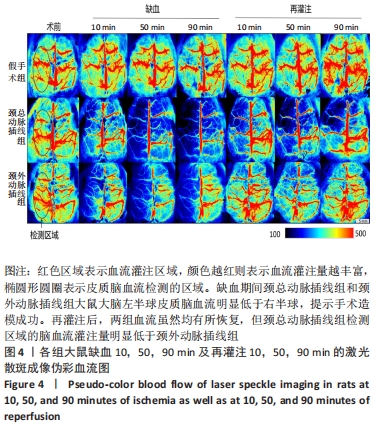
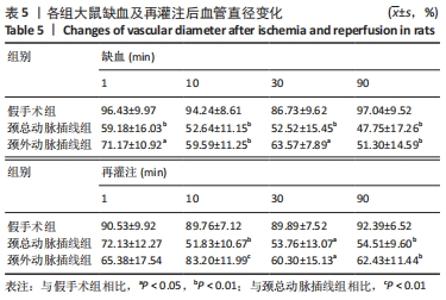
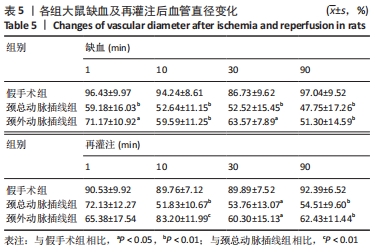
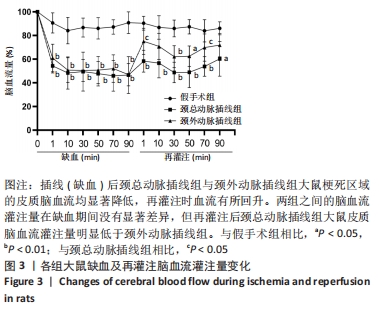
2.5 脑血流灌注量变化 栓塞10 min后,两组大鼠的脑血流灌注量均显著减小(P < 0.01);缺血30 min后颈总动脉插线组和颈外动脉插线组脑血流灌注量分别下降至基础值的49.4%和50.3%;缺血90 min 颈总动脉插线组和颈外动脉插线组脑血流灌注量分别下降至基础值的46.6%和46.8%。两组之间的脑血流灌注量在缺血期间差异无显著性(P > 0.05)。再灌注1 min,颈外动脉插线组和颈总动脉插线组脑血流灌注量回升至基值的75%和58%(P < 0.05),随后两组脑血流的灌注量均出现缓慢下降并维持在低灌注状态。颈外动脉插线组和颈总动脉插线组低灌注状态的脑血流量维持在基值的60%-70%和50%-60%,再灌注70 min差异有显著性意义 (P < 0.05),见图3,4。"
| [1] JOHNSON W, ONUMA O, OWOLABI M, et al. Stroke: a global response is needed. Bull World Health Organ. 2016;94(9):634. [2] FEIGIN VL, STARK BA, JOHNSON CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795-820. [3] HAY SI, ABAJOBIR AA, ABATE KH, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260-1344. [4] BOGOUSSLAVSKY J, Van MELLE G, REGLI F. The Lausanne Stroke Registry: analysis of 1,000 consecutive patients with first stroke. Stroke. 1988;19(9):1083-1092. [5] GEORGE MG, TONG X, BOWMAN BA. Prevalence of Cardiovascular Risk Factors and Strokes in Younger Adults. JAMA Neurol. 2017;74(6):695-703. [6] MCCABE C, ARROJA MM, REID E, et al. Animal models of ischaemic stroke and characterisation of the ischaemic penumbra. Neuropharmacology. 2018;134(Pt B):169-177. [7] HOWELLS DW, PORRITT MJ, REWELL SS, et al. Different strokes for different folks: the rich diversity of animal models of focal cerebral ischemia. J Cereb Blood Flow Metab. 2010;30(8):1412-1431. [8] KOIZUMI J, YOSHIDA Y, NAKAZAWA T, et al. Experimental studies of ischemic brain edema. 1. A new experimental model of cerebral embolism in rats in which recirculation can be introduced in the ischemic area. Nosotchu. 1986;8:1-7. [9] LONGA EZ, WEINSTEIN PR, CARLSON S, et al. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989;20(1):84-91. [10] LAING RJ, JAKUBOWSKI J, LAING RW. Middle cerebral artery occlusion without craniectomy in rats. Which method works best? Stroke. 1993; 24(2):294-297,298. [11] ULUC K, MIRANPURI A, KUJOTH GC, et al. Focal cerebral ischemia model by endovascular suture occlusion of the middle cerebral artery in the rat. J Vis Exp. 2011;(48):1978. [12] ANSARI S, AZARI H, MCCONNELL DJ, et al. Intraluminal middle cerebral artery occlusion (MCAO) model for ischemic stroke with laser doppler flowmetry guidance in mice. J Vis Exp. 2011;(51):2879. [13] LU M, CHEN J, LU D, et al. Global test statistics for treatment effect of stroke and traumatic brain injury in rats with administration of bone marrow stromal cells. J Neurosci Methods. 2003;128(1-2):183-190. [14] CHOI WJ, LI Y, WANG RK. Monitoring Acute Stroke Progression: Multi-Parametric OCT Imaging of Cortical Perfusion, Flow, and Tissue Scattering in a Mouse Model of Permanent Focal Ischemia. IEEE Trans Med Imaging. 2019;38(6):1427-1437. [15] WARNER DS, TAKAOKA S, WU B, et al. Electroencephalographic burst suppression is not required to elicit maximal neuroprotection from pentobarbital in a rat model of focal cerebral ischemia. Anesthesiology. 1996;84(6):1475-1484. [16] WANG CQ, YE Y, CHEN F, et al. Posttraumatic administration of a sub-anesthetic dose of ketamine exerts neuroprotection via attenuating inflammation and autophagy. Neuroscience. 2017;343:30-38. [17] XIONG Z, CHANG L, QU Y, et al. Neuronal brain injury after cerebral ischemic stroke is ameliorated after subsequent administration of (R)-ketamine, but not (S)-ketamine. Pharmacol. Biochem. 2020;191: 172904. [18] 董传斌. 吸入性麻醉剂与脑缺血及神经保护的研究进展[J]. 中国老年学杂志,2021,41(16):3615-3620. [19] CHI OZ, MELLENDER SJ, KISS GK, et al. Blood -brain barrier disruption was less under isoflurane than pentobarbital anesthesia via a PI3K/Akt pathway in early cerebral ischemia. Brain Res. Bull. 2017;131:1-6. [20] 孙宇, 严国锋, 姜虹, 等. 改良线栓法大鼠大脑中动脉阻塞模型的建立[J]. 中国比较医学杂志,2008,18(8):8-10. [21] CAI Q, XU G, LIU J, et al. A modification of intraluminal middle cerebral artery occlusion/reperfusion model for ischemic stroke with laser Doppler flowmetry guidance in mice. Neuropsychiatr Dis Treat. 2016; 12:2851-2858. [22] MORRIS GP, WRIGHT AL, TAN RP, et al. A Comparative Study of Variables Influencing Ischemic Injury in the Longa and Koizumi Methods of Intraluminal Filament Middle Cerebral Artery Occlusion in Mice. PLoS One. 2016;11(2):e148503. [23] LIU F, MCCULLOUGH LD. Middle cerebral artery occlusion model in rodents: methods and potential pitfalls. J Biomed Biotechnol. 2011; 2011:464701. [24] TANG Q, HAN R, XIAO H, et al. Role of suture diameter and vessel insertion position in the establishment of the middle cerebral artery occlusion rat model. Exp Ther Med. 2013;5(6):1603-1608. [25] 杨德兵, 张利宏, 马存根. 大鼠大脑中动脉缺血再灌注模型的改良[J]. 中国民族民间医药,2009,18(16):27-29. [26] LIU S, ZHEN G, MELONI BP, et al. Rodent stroke model guidelines for preclinical stroke trials (1st edition). J Exp Stroke Transl Med. 2009;2(2): 2-27. [27] SMITH HK, RUSSELL JM, GRANGER DN, et al. Critical differences between two classical surgical approaches for middle cerebral artery occlusion-induced stroke in mice. J Neurosci Methods. 2015;249:99-105. [28] 王东亮, 王冬, 何天鹏, 等. 两种线栓法制作小鼠大脑中动脉栓塞模型的比较[J]. 中华神经创伤外科电子杂志,2019,5(6):358-364. [29] 向珩. 早期电针刺激训练实验性局灶性脑缺血大鼠健侧肢体康复效果研究[D]. 天津: 天津体育学院,2008. [30] 田智慧, 廖卫国, 余健烨, 等. LSCI检测不同缺血期对大鼠缺血再灌注过程脑血流的影响[J]. 中国临床解剖学杂志,2017,35(4):409-412. [31] LIU JR, JENSEN-KONDERING UR, ZHOU JJ, et al. Transient filament occlusion of the middle cerebral artery in rats: does the reperfusion method matter 24 hours after perfusion? BMC Neurosci. 2012;13:154. [32] ZUO XL, DENG HL, WU P, et al. Do different reperfusion methods affect the outcomes of stroke induced by MCAO in adult rats? Int J Neurosci. 2016;126(9):850-855. [33] DITTMAR M, SPRUSS T, SCHUIERER G, et al. External carotid artery territory ischemia impairs outcome in the endovascular filament model of middle cerebral artery occlusion in rats. Stroke. 2003;34(9):2252-2257. [34] DITTMAR MS, VATANKHAH B, FEHM NP, et al. The role of ECA transection in the development of masticatory lesions in the MCAO filament model. Exp. Neurol. 2005;195(2):372-378. [35] De MEY JG, VANHOUTTE PM. End o’ the line revisited: moving on from nitric oxide to CGRP. Life Sci. 2014;118(2):120-128. [36] ZHAI L, SAKURAI T, KAMIYOSHI A, et al. Endogenous calcitonin gene-related peptide suppresses ischemic brain injuries and progression of cognitive decline. J Hypertens. 2018;36(4):876-891. [37] SWAN CE, BREYER RM. Prostaglandin E2 modulation of blood pressure homeostasis: studies in rodent models. Prostaglandins Other Lipid Mediat. 2011;96(1-4):10-13. [38] 党立, 王希敏, 韩利文, 等. 环磷酸腺苷的临床应用进展[J]. 山东科学,2007,20(3):61-64. [39] 高飞, 胡晓露, 陈康宁. 环磷腺苷信号通路与血管重塑关系的研究进展[J]. 中国卒中杂志,2017,12(9):863-868. [40] CHIA NH, LEYDEN JM, NEWBURY J, et al. Determining the Number of Ischemic Strokes Potentially Eligible for Endovascular Thrombectomy: A Population-Based Study. Stroke. 2016;47(5):1377-1380. [41] HENNINGER N, FISHER M. Extending the Time Window for Endovascular and Pharmacological Reperfusion. Transl Stroke Res. 2016;7(4):284-293. [42] ZHANG PL, WANG YX, CHEN Y, et al. Use of Intravenous Thrombolytic Therapy in Acute Ischemic Stroke Patients: Evaluation of Clinical Outcomes. Cell Biochem Biophys. 2015;72(1):11-17. [43] 陈琳. 急性缺血性卒中血管再通患者多模式影像的动态变化及其作用研究[D]. 杭州: 浙江大学,2020. [44] TURGAY D, ETHEM MA. Can Restoring Incomplete Microcirculatory Reperfusion Improve Stroke Outcome after Thrombolysis? J Cereb Blood Flow Metab. 2012;32(12):2091-2099. [45] BRAD AS, AIN AN, YVONNE C, et al. The transient intraluminal filament middle cerebral artery occlusion model as a model of endovascular thrombectomy in stroke. J Cereb Blood Flow Metab. 2016;36(2):363-369. [46] WANG W, JIANG B, SUN H, et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation. 2017;135(8):759-771. [47] 任北大, 程发峰, 王雪茜, 等. 雌激素对缺血性脑卒中的保护作用及相关机制研究进展[J]. 医学综述, 2019,25(2): 215-221. |
| [1] | Nie Chenchen, Su Kaiqi, Gao Jing, Fan Yongfu, Ruan Xiaodi, Yuan Jie, Duan Zhaoyuan, Feng Xiaodong. The regulatory role of circular RNAs in cerebral ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(8): 1286-1291. |
| [2] | Qin Yuxing, Ren Qiangui, Li Zilong, Quan Jiaxing, Shen Peifeng, Sun Tao, Wang Haoyu. Action mechanism and prospect of bone microvascular endothelial cells for treating femoral head necrosis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(6): 955-961. |
| [3] | Liu Gang, Deng Bowen, Jiang Shengyuan, Xu Lin, Fan Xiao, Tao Jingwei, Zhang Houjun, He Feng, Zhao Yi, Mu Xiaohong. Tetramethylpyrazine improves hemorheological indexes in rats with complete spinal cord transection: a dynamic observation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(2): 282-286. |
| [4] | Hu Fei, Wang Jie. Safety and efficacy of mesenchymal stem cells in the treatment of ischemic stroke: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(1): 76-82. |
| [5] | Gao Lei, Qin Xinyuan, Nie Xin, Wang Lei, Wang Jiangning. Extracorporeal circulation compression perfusion in the reconstruction of limb microcirculation from the mechanism of mechanical and chemical signal transduction [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1334-1340. |
| [6] | Fan Yongfu, Su Kaiqi, Yuan Jie, Nie Chenchen, Ruan Xiaodi, Duan Zhaoyuan, Feng Xiaodong. Relationship between iron metabolism and ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(32): 5223-5228. |
| [7] | Yan Nan, Wu Yanlong, Tang Xiaohui, Zhang Xiaoyan, Wang Hui, Yang Tianze, Zhou Maochun, Wang Zhengdong, Yang Xiaoxia. Bone marrow mesenchymal stem cells may alleviate brain damage caused by the microglial overactivation in the cortex around ischemic site of stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(24): 3790-3795. |
| [8] | Chen Na, Wang Xiaohan, Zhang Yunke. Effect and mechanism of mesenchymal stem cells on aging-related ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(24): 3914-3920. |
| [9] | Xu Wenshan, Jiang Pingli, Liu Yulu, Ding Yanyi, Yu Yan, Yang Minguang, Liu Weilin, Chen Lidian. Salvianolic acid A effects on hippocampal protein expression in ischemic stroke rats: a tandem mass tag-based proteomic analysis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(23): 3714-3720. |
| [10] | Xiakeerzhati•Xiaohalati, Wang Xiaobei, Wang Lin. Nanoparticles: a novel strategy for the treatment of ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3566-3572. |
| [11] | Li Shulun, Hao Peng, Hao Fei, Duan Hongmei, Zhao Wen, Gao Yudan, Yang Chaoyang, Li Xiaoguang. Pathological changes in rats with ischemic stroke induced by improved photochemical embolization [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(2): 218-224. |
| [12] | Chen Na, Fan Feiyan, Li Shuangli, Zhang Yunke. Effect and mechanism of traditional Chinese medicine regulating mesenchymal stem cell-derived exocrine for ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(13): 2081-2086. |
| [13] | Yuan Chunhua, Cui Zhenzhen, Wu De. Meta-analysis of autologous bone marrow mesenchymal stem cell transplantation in the treatment of ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(31): 5018-5024. |
| [14] | Huang Maomao, Hu Yue, Wang Binchuan, Zhang Chi, Xie Yujie, Wang Jianxiong, Wang Li, Xu Fangyuan. Bibliometric and visual analysis of international literature addressing ischemic stroke rehabilitation in recent 10 years [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3725-3733. |
| [15] | Liang Yanfeng, Hao Peng, Duan Hongmei, Zhao Wen, Gao Yudan, Li Xiaoguang, Yang Chaoyang. Pathological and behavioral changes after ischemic stroke in adult mice [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(35): 5625-5631. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||