[1] NOBORU M. A brief history of autophagy from cell biology to physiology and disease. Nat Cell Biol. 2018;20(5):521-527.
[2] DERETIC V, KLIONSKY DJ. Autophagy and inflammation: A special review issue. Autophagy. 2018;14(2):179-180.
[3] BULLON P, CORDERO MD, QUILES JL, et al. Autophagy in periodontitis patients and gingival fibroblasts: unraveling the link between chronic diseases and inflammation. BMC Med. 2012;10:122.
[4] ZHOU W, NI J, SHU R, et al. Hypoxia induces apoptosis and autophagic cell death in human periodontal ligament cells through HIF-1α pathway. Cell Proliferation. 2012;45(3):239-248.
[5] WANG Q, XUE P, ZHANG Y, et al. Increased autophagy is required to protect periodontal ligament stem cells from apoptosis in inflammatory microenvironment. J Clin Periodontol. 2016;43(7):618-625.
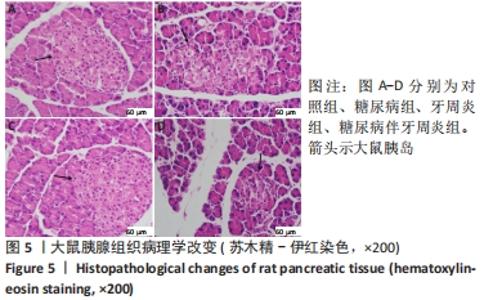
[6] 杨雯雯, 魏巍, 张丽. 自噬相关蛋白在2型糖尿病大鼠胰腺组织中的变化[J]. 新疆医科大学学报,2019,42(6):739-742,747.
[7] 刘尔黎, 钟雯怡, 刘增一, 等. 2型糖尿病伴牙周炎牙周膜干细胞成牙骨质分化能力的研究[J]. 遵义医科大学学报,2020,43(5):599-605.
[8] 夏佳佳, 王岚, 刘琪, 等. 2型糖尿病伴牙周炎患者牙周膜干细胞骨向分化研究[J]. 实用口腔医学杂志,2011,27(5):624-629.
[9] HUI F, KUN Y, PING T, et al. Glycosylation end products mediate damage and apoptosis of periodontal ligament stem cells induced by the JNK-mitochondrial pathway. Aging. 2020;12(13):12850-12868.
[10] 杨靖靖, 刘明宏, 吴迎涛. 牙周病与糖尿病关系的进展研究[J]. 中国老年学杂志,2016,36(23):6040-6042.
[11] 徐欣然, 和璐. 牙周炎对2型糖尿病发病影响的动物实验研究进展[J]. 中国糖尿病杂志,2021,29(2):145-148.
[12] 梁丽华, 唐海松, 秦明群, 等. 高脂高糖联合小剂量链尿佐菌素建立2型糖尿动物模型的研究[J]. 全科口腔医学杂志(电子版), 2019,6(20):163-165.
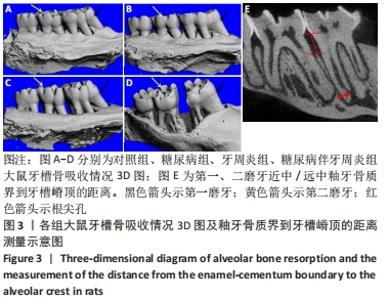
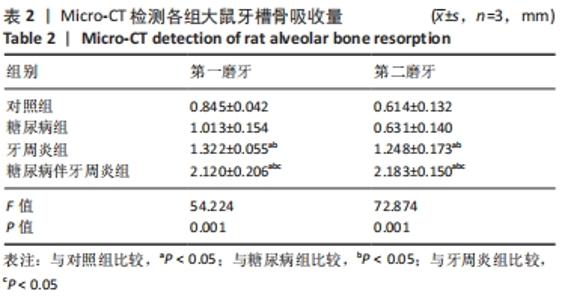
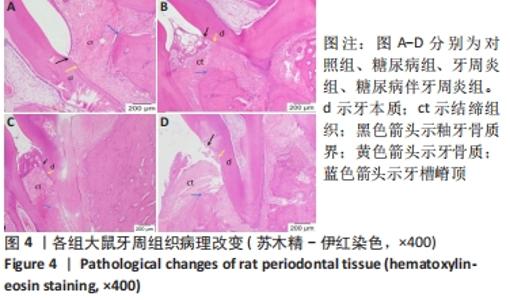
[13] 王立刚, 徐彬, 阿吉迪丽努尔, 等. 糖尿病牙周炎模型大鼠的牙槽骨丧失[J]. 中国组织工程研究,2015,19(5):710-715.
[14] 陈景宜, 张昀, 陈彩云, 等. 实验性牙周炎模型大鼠牙槽骨微结构的改变[J]. 口腔医学研究,2017,33(11):1165-1168.
[15] LEE J, KIM HS. The Role of Autophagy in Eosinophilic Airway Inflammation. Immune Network. 2019;19(1):e5.
[16] SHAO ZQ, DOU SS, ZHU JG, et al. Apelin-13 inhibits apoptosis and excessive autophagy in cerebral ischemia/reperfusion injury. Neural Regen Res. 2021;16(6):1044-1051.
[17] KRAKAUER T. Inflammasomes, Autophagy, and Cell Death: The Trinity of Innate Host Defense against Intracellular Bacteria. Mediators Inflamm. 2019;2019:1-10.
[18] MARTINE L, LETICIA FT, MAKIKO F, et al. Dysfunctional autophagy following exposure to pro-inflammatory cytokines contributes to pancreatic β-cell apoptosis. Cell Death Dis. 2018;9(2):96.
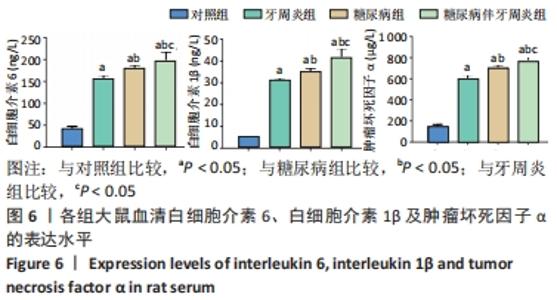
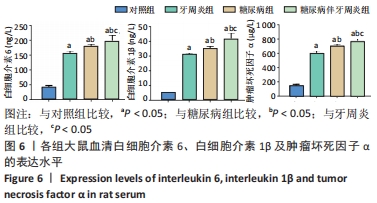
[19] 马凌云, 孙凌玉, 康静蕊, 等. 2型糖尿病与炎症因子CRP、TNF-α、IL-6的关系[J]. 临床医药文献电子杂志,2017,4(56):11052.
[20] 中国2型糖尿病防治指南(2017年版)[J]. 中国实用内科杂志, 2018,38(4):292-344.
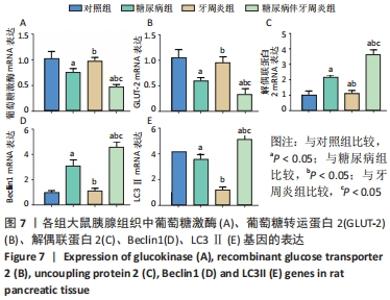
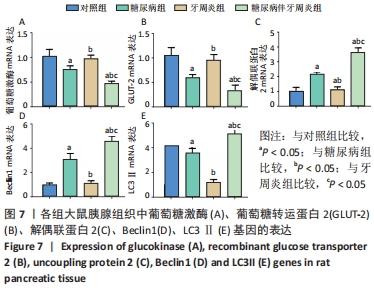
[21] BJORKHAUG L, DOSKELAND A, WIERUP N, et al. Nuclear import of glucokinase in pancreatic beta-cells is mediated by a nuclear localization signal and modulated by SUMOylation. Mol Cell Endocrinol. 2017;454:146-157.
[22] 郑宏庭, 邓华聪. 葡萄糖激酶与糖尿病的研究进展[J]. 中国临床康复,2004,8(27):5960-5961.
[23] 曹宏伟, 姬秋和. 葡萄糖激酶调控血糖稳态的主要方式——调节控糖激素分泌和肝糖原合成[J]. 中华糖尿病杂志,2020,12(7):539-542.
[24] LI D, LINGLING H, JOHN D, et al. Erratum. WASH Regulates Glucose Homeostasis by Facilitating Glut2 Receptor Recycling in Pancreatic β-Cells. Diabetes. 2019;68:377-386.
[25] 黄林晶, 杨立勇. 葡萄糖转运蛋白2与糖尿病的关系研究进展[J]. 医学综述,2009,15(23):3617-3619.
[26] 何柳, 宋岩, 胡永华. 解偶联蛋白2与2型糖尿病关系研究进展[J]. 现代预防医学,2008,35(22):4501-4503,4508.
[27] YIFEI Y, BOYANG Z, MASANORI N, et al. Islet β-cell-produced NUCB2/nesfatin-1 maintains insulin secretion and glycemia along with suppressing UCP-2 in β-cells. J Physiol Sci. 2019;69(5):733-739.
[28] Guo QY, Robson-Doucette CA, Allister EM, et al. Inducible Deletion of UCP2 in Pancreatic β-Cells Enhances Insulin Secretion. Canad J Diabetes. 2012;36(5):237-243.
[29] XU HD, QIN ZH. Beclin 1, Bcl-2 and Autophagy. Adv Exp Med Biol. 2019; 1206:109-126.
[30] KANG R, ZEH HJ, LOTZE MT, et al. The Beclin 1 network regulates autophagy and apoptosis. Cell Death Differ. 2011;18(4):571-580.
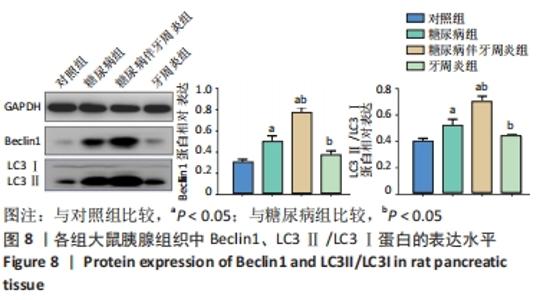
[31] LONG C, XIAOCHUAN W, XIN Z, et al. The autophagy-related genes Beclin1 and LC3 in the prognosis of pancreatic cancer. Int J Clin Exp Pathol. 2019;12(8):2989-2996.
[32] 余州, 王彤, 宋雅娟, 等. 细胞自噬的研究方法进展[J]. 细胞与分子免疫学杂志,2019,35(9):849-854.
|