Chinese Journal of Tissue Engineering Research ›› 2022, Vol. 26 ›› Issue (13): 1979-1984.doi: 10.12307/2022.321
Previous Articles Next Articles
Wnt/beta-catenin signaling pathway in the treatment of chronic obstructive pulmonary disease with bone marrow mesenchymal stem cells
Zhong Yulan1, Zhou Xiangxiang1, Gan Xin2
- 1Jiangxi Provincial Chest Hospital, Nanchang 330006, Jiangxi Province, China; 2Department of Respiratory and Critical Care Medicine, First Affiliated Hospital of Nanchang University, Nanchang 330006, Jiangxi Province, China
-
Received:2020-10-19Revised:2020-10-22Accepted:2020-12-14Online:2022-05-08Published:2021-12-18 -
Contact:Gan Xin, MD, Chief physician, Department of Respiratory and Critical Care Medicine, First Affiliated Hospital of Nanchang University, Nanchang 330006, Jiangxi Province, China -
About author:Zhong Yulan, Master, Physician, Jiangxi Provincial Chest Hospital, Nanchang 330006, Jiangxi Province, China -
Supported by:National Natural Science Foundation of China, No. 81660009, 81260004 (to GX); Natural Science Foundation of Jiangxi Province, No. 20192BAB215002 (to GX)
CLC Number:
Cite this article
Zhong Yulan, Zhou Xiangxiang, Gan Xin. Wnt/beta-catenin signaling pathway in the treatment of chronic obstructive pulmonary disease with bone marrow mesenchymal stem cells[J]. Chinese Journal of Tissue Engineering Research, 2022, 26(13): 1979-1984.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
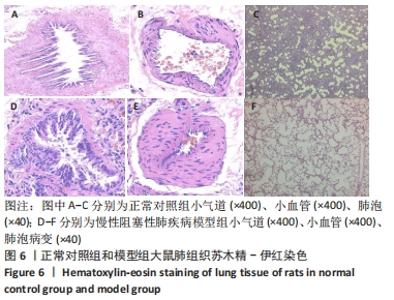
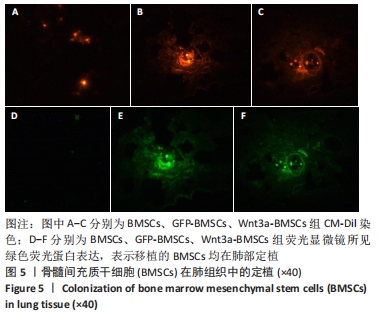
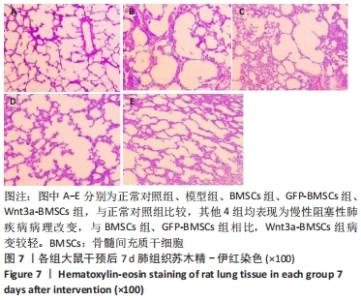
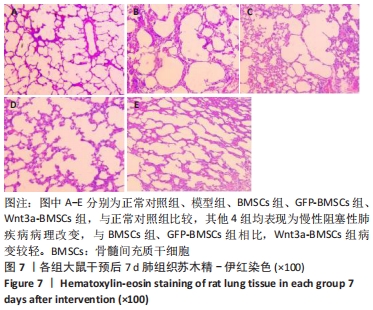
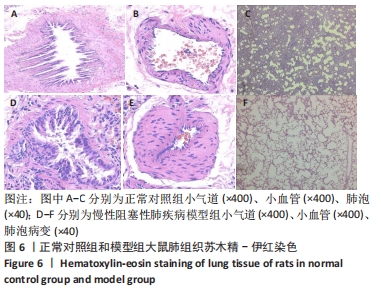
2.4 慢性阻塞性肺疾病造模结果及BMSCs移植后肺组织病理学改变 正常对照组:肺泡大小均匀,肺泡壁无明显增厚,肺泡腔干净、匀称,周围未见明显炎细胞浸润及部分肺间隔断裂;模型组:肺泡间隔可见炎细胞浸润及部分肺间隔断裂,肺泡腔扩大且大小不一,相同视野内肺泡数目减少,小血管管壁增厚,见图6,说明造模成功;BMSCs组、GFP-BMSCs组、Wnt3a-BMSCs组:相同视野下,各组肺泡腔不规则扩大,仍有部分肺泡间隔断裂伴肺大疱形成,肺间质血管管壁及气管管壁仍有少数炎性细胞浸润。BMSCs组、GFP-BMSCs组之间无明显差异;与BMSCs组、GFP-BMSCs组比较,Wnt3a-BMSCs组病变较轻,见图7。"

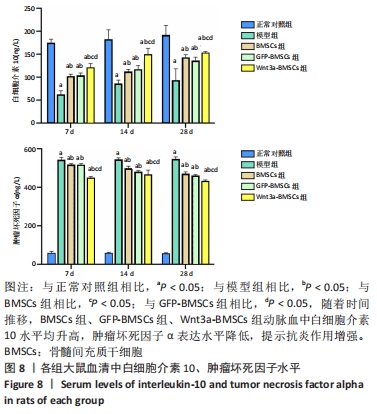
2.5 各组大鼠血清中肿瘤坏死因子α、白细胞介素10水平 在相同时间点,BMSCs组、GFP-BMSCs组、Wnt3a-BMSCs组动脉血中白细胞介素10水平高于模型组,肿瘤坏死因子α水平低于模型组(均P < 0.05);BMSCs组、GFP-BMSCs组动脉血中白细胞介素10、肿瘤坏死因子α水平差别不大,但Wnt3a-BMSCs组白细胞介素10水平高于BMSCs组、GFP-BMSCs组,肿瘤坏死因子α水平低于BMSCs组、GFP-BMSCs组,差异有显著性意义(均P < 0.05);随着时间推移,BMSCs组、GFP-BMSCs组、Wnt3a-BMSCs组动脉血中白细胞介素10水平均升高,肿瘤坏死因子α表达水平降低,提示抗炎作用增强,见图8。"
| [1] REGAN EA, LYNCH DA, CURRAN-EVERETT D, et al. Clinical and Radiologic Disease in Smokers With Normal Spirometry. JAMA Intern Med. 2015;175(9):1539-1549. [2] PIERÓG J, FYTIANOS K, TAMÒ L, et al. Stem cell secretome attenuates acute rejection in rat lung allotransplant. Interact Cardiovasc Thorac Surg. 2019;28(5):812-818. [3] CAHILL EF, TOBIN LM, CARTY F, et al. Jagged-1 is required for the expansion of CD4+ CD25+ FoxP3+ regulatory T cells and tolerogenic dendritic cells by murine mesenchymal stromal cells. Stem Cell Res Ther. 2015;6(1):19. [4] WANG K, LI Y, ZHU T, et al. Overexpression of c-Met in bone marrow mesenchymal stem cells improves their effectiveness in homing and repair of acute liver failure. Stem Cell Res Ther. 2017;8(1):162. [5] CHEN X, ZHANG Y, WANG W, et al. Mesenchymal Stem Cells Modified with Heme Oxygenase-1 Have Enhanced Paracrine Function and Attenuate Lipopolysaccharide-Induced Inflammatory and Oxidative Damage in Pulmonary Microvascular Endothelial Cells. Cell Physiol Biochem. 2018;49(1):101-122. [6] PIERÓG J, TAMO L, FAKIN R, et al. Bone marrow stem cells modified with human interleukin 10 attenuate acute rejection in rat lung allotransplantation. Eur J Cardiothorac Surg. 2018;53(1):194-200. [7] KENNELLY H, MAHON BP, ENGLISH K. Human mesenchymal stromal cells exert HGF dependent cytoprotective effects in a human relevant pre-clinical model of COPD. Sci Rep. 2016;6:38207. [8] CURLEY GF, HAYES M, ANSARI B, et al. Mesenchymal stem cells enhance recovery and repair following ventilator-induced lung injury in the rat. Thorax. 2012;67(6): 496-501. [9] SHI Y, HU G, SU J, et al. Mesenchymal stem cells: a new strategy for immunosuppression and tissue repair. Cell Res. 2010;20(5):510-518. [10] YANG J, JIA Z. Cell-based therapy in lung regenerative medicine. Regen Med Res. 2014;2(1):7. [11] LIU AR, LIU L, CHEN S, et al. Activation of canonical wnt pathway promotes differentiation of mouse bone marrow-derived MSCs into type II alveolar epithelial cells, confers resistance to oxidative stress, and promotes their migration to injured lung tissue in vitro. J Cell Physiol. 2013;228(6):1270-1283. [12] HOLLAND JD, KLAUS A, GARRATT AN, et al. Wnt signaling in stem and cancer stem cells. Curr Opin Cell Biol. 2013;25(2):254-264. [13] FALCONI G, FABIANI E, FIANCHI L, et al. Impairment of PI3K/AKT and WNT/β-catenin pathways in bone marrow mesenchymal stem cells isolated from patients with myelodysplastic syndromes. Exp Hematol. 2016;44(1):75-83.e1-4. [14] 吴华拉,周湘乡,钟玉兰,等. 碱性成纤维细胞生长因子转染骨髓间充质干细胞移植治疗慢性阻塞性肺疾病的作用及机制[J].中国组织工程研究,2019, 23(21):3378-3385. [15] CHANG C, GUO Z, SHEN N, et al. Dynamics of inflammation resolution and symptom recovery during AECOPD treatment. Sci Rep. 2014;4:5516. [16] RABE KF, WATZ H. Chronic obstructive pulmonary disease. Lancet. 2017;389 (10082):1931-1940. [17] CHEN M, HUANG Z, BI H, et al. Effects of bone marrow‑derived mesenchymal stem cell transplantation on chronic obstructive pulmonary disease/obstructive sleep apnea overlap syndrome in rats. Mol Med Rep. 2019;20(5):4665-4673. [18] LI X, XU J, LI P. Rat bone mesenchymal stem cells exert antiproliferative effects on nicotine‑exposed T cells via iNOS production. Mol Med Rep. 2020;21(5):2267-2275. [19] NAJAR M, BOUHTIT F, MELKI R, et al. Mesenchymal Stromal Cell-Based Therapy: New Perspectives and Challenges. J Clin Med. 2019;8(5):626. [20] BLÁZQUEZ R, SÁNCHEZ-MARGALLO FM, ÁLVAREZ V, et al. Surgical meshes coated with mesenchymal stem cells provide an anti-inflammatory environment by a M2 macrophage polarization. Acta Biomater. 2016;31:221-230. [21] LI Q, CHEN X, LI J. Marrow-derived mesenchymal stem cells regulate the inflammatory response and repair alveolar type II epithelial cells in acute lung injury of rats. J Int Med Res. 2020;48(4):300060520909027. [22] LI X, AN G, WANG Y, et al. Targeted migration of bone marrow mesenchymal stem cells inhibits silica-induced pulmonary fibrosis in rats. Stem Cell Res Ther. 2018;9(1):335. [23] TANG Y, CAI QH, WANG YJ, et al. Protective effect of autophagy on endoplasmic reticulum stress induced apoptosis of alveolar epithelial cells in rat models of COPD. Biosci Rep. 2017;37(6):BSR20170803. [24] GENG L, CHEN Z, REN H, et al. Effects of an early intervention using human amniotic epithelial cells in a COPD rat model. Pathol Res Pract. 2016;212(11): 1027-1033. [25] STEINHART Z, ANGERS S. Wnt signaling in development and tissue homeostasis. Development. 2018;145(11):dev146589. [26] CAI SX, LIU AR, HE HL, et al. Stable genetic alterations of β-catenin and ROR2 regulate the Wnt pathway, affect the fate of MSCs. J Cell Physiol. 2014;229(6): 791-800. [27] CAI SX, LIU AR, CHEN S, et al. Activation of Wnt/β-catenin signalling promotes mesenchymal stem cells to repair injured alveolar epithelium induced by lipopolysaccharide in mice. Stem Cell Res Ther. 2015;6(1):65. [28] PHINNEY DG, PITTENGER MF. Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells. 2017;35(4):851-858. [29] 钟玉兰,淦鑫.间充质干细胞源外泌体在肺部疾病中的应用与作用[J].中国组织工程研究,2019,23(13):2121-2126. [30] ALIOTTA JM, PEREIRA M, WEN S, et al. Exosomes induce and reverse monocrotaline-induced pulmonary hypertension in mice. Cardiovasc Res. 2016; 110(3):319-330. [31] MACHIN M, AMARAL AF, WIELSCHER M, et al. Systematic review of lung function and COPD with peripheral blood DNA methylation in population based studies. BMC Pulm Med. 2017;17(1):54. [32] MALAVIYA R, LASKIN JD, LASKIN DL. Anti-TNFalpha therapy in inflammatory lung diseases. Pharmacol Ther. 2017;180:90-98. [33] YAO Y, ZHOU J, DIAO X, et al. Association between tumor necrosis factor-alpha and chronic obstructive pulmonary disease: a systematic review and meta-analysis. Ther Adv Respir Dis. 2019;13:1753466619866096. [34] DOLGACHEV VA, YU B, SUN L, et al. Interleukin 10 overexpression alters survival in the setting of gram-negative pneumonia following lung contusion. Shock. 2014; 41(4):301-310. [35] YAGI H, SOTO-GUTIERREZ A, PAREKKADAN B, et al. Mesenchymal stem cells: Mechanisms of immunomodulation and homing. Cell Transplant. 2010;19(6): 667-679. [36] PEDROSA M, GOMES J, LARANJEIRA P, et al. Immunomodulatory effect of human bone marrow-derived mesenchymal stromal/stem cells on peripheral blood T cells from rheumatoid arthritis patients. J Tissue Eng Regen Med. 2020;14(1):16-28. [37] HE QQ, HE X, WANG YP, et al. Transplantation of bone marrow-derived mesenchymal stem cells (BMSCs) improves brain ischemia-induced pulmonary injury in rats associated to TNF-α expression. Behav Brain Funct. 2016;12(1):9. [38] ZHU H, XIONG Y, XIA Y, et al. Therapeutic Effects of Human Umbilical Cord-Derived Mesenchymal Stem Cells in Acute Lung Injury Mice. Sci Rep. 2017;7:39889. |
| [1] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [2] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [3] | Huang Chenwei, Fei Yankang, Zhu Mengmei, Li Penghao, Yu Bing. Important role of glutathione in stemness and regulation of stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1119-1124. |
| [4] | Hui Xiaoshan, Bai Jing, Zhou Siyuan, Wang Jie, Zhang Jinsheng, He Qingyong, Meng Peipei. Theoretical mechanism of traditional Chinese medicine theory on stem cell induced differentiation [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1125-1129. |
| [5] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [6] | Fan Yiming, Liu Fangyu, Zhang Hongyu, Li Shuai, Wang Yansong. Serial questions about endogenous neural stem cell response in the ependymal zone after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1137-1142. |
| [7] | Tian Chuan, Zhu Xiangqing, Yang Zailing, Yan Donghai, Li Ye, Wang Yanying, Yang Yukun, He Jie, Lü Guanke, Cai Xuemin, Shu Liping, He Zhixu, Pan Xinghua. Bone marrow mesenchymal stem cells regulate ovarian aging in macaques [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 985-991. |
| [8] | Hou Jingying, Guo Tianzhu, Yu Menglei, Long Huibao, Wu Hao. Hypoxia preconditioning targets and downregulates miR-195 and promotes bone marrow mesenchymal stem cell survival and pro-angiogenic potential by activating MALAT1 [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1005-1011. |
| [9] | Zhou Ying, Zhang Huan, Liao Song, Hu Fanqi, Yi Jing, Liu Yubin, Jin Jide. Immunomodulatory effects of deferoxamine and interferon gamma on human dental pulp stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1012-1019. |
| [10] | Liang Xuezhen, Yang Xi, Li Jiacheng, Luo Di, Xu Bo, Li Gang. Bushen Huoxue capsule regulates osteogenic and adipogenic differentiation of rat bone marrow mesenchymal stem cells via Hedgehog signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1020-1026. |
| [11] | Wang Jifang, Bao Zhen, Qiao Yahong. miR-206 regulates EVI1 gene expression and cell biological behavior in stem cells of small cell lung cancer [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1027-1031. |
| [12] | Liu Feng, Peng Yuhuan, Luo Liangping, Wu Benqing. Plant-derived basic fibroblast growth factor maintains the growth and differentiation of human embryonic stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1032-1037. |
| [13] | Wen Dandan, Li Qiang, Shen Caiqi, Ji Zhe, Jin Peisheng. Nocardia rubra cell wall skeleton for extemal use improves the viability of adipogenic mesenchymal stem cells and promotes diabetes wound repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1038-1044. |
| [14] | Zhu Bingbing, Deng Jianghua, Chen Jingjing, Mu Xiaoling. Interleukin-8 receptor enhances the migration and adhesion of umbilical cord mesenchymal stem cells to injured endothelium [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1045-1050. |
| [15] | Luo Xiaoling, Zhang Li, Yang Maohua, Xu Jie, Xu Xiaomei. Effect of naringenin on osteogenic differentiation of human periodontal ligament stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1051-1056. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||