Chinese Journal of Tissue Engineering Research ›› 2021, Vol. 25 ›› Issue (28): 4580-4586.doi: 10.12307/2021.076
Previous Articles Next Articles
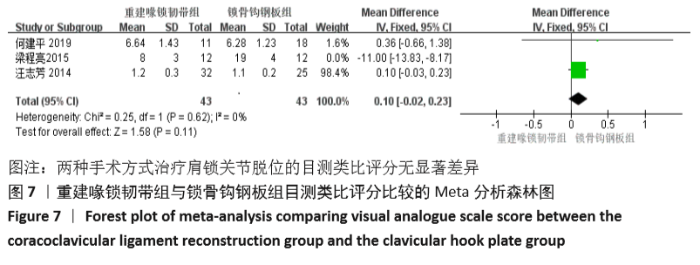
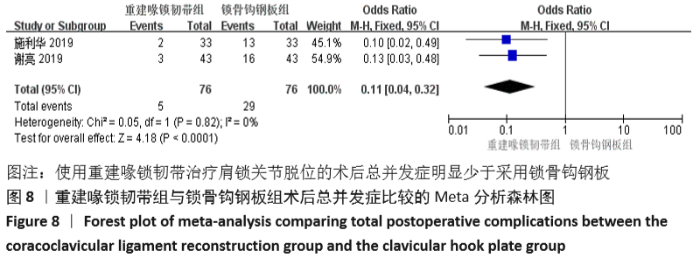
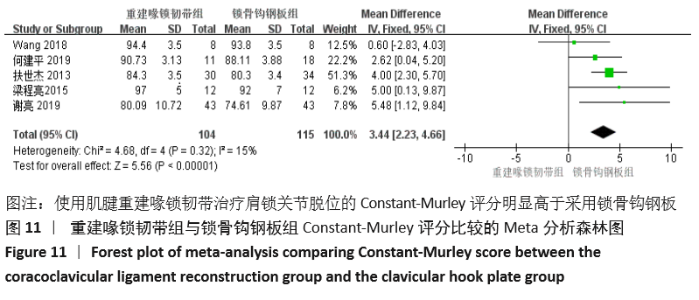
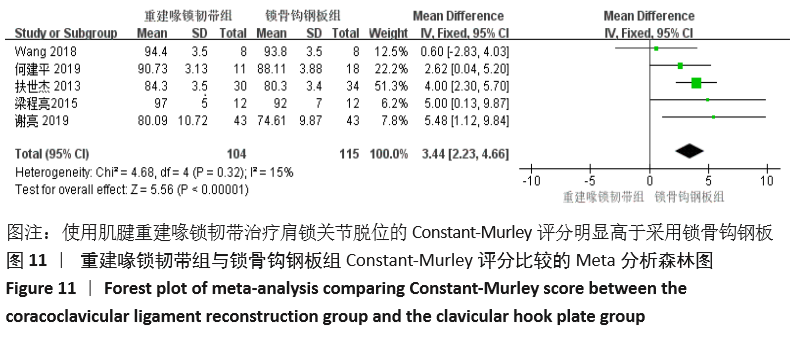
Meta-analysis of coracoclavicular ligament reconstruction with autologous or allogeneic tendon and clavicular hook plate in the treatment of acromioclavicular joint dislocation
Yang Kun1, Fei Chen1, Wang Pengfei2, Zhang Binfei2, Yang Na2, Tian Ding2, Zhuang Yan2, Zhang Kun2
- 1Graduate School of Xi’an Medical University, Xi’an 710068, Shaanxi Province, China; 2Department of Orthopedic Trauma, Xi’an Honghui Hospital Affiliated to Xi’an Jiaotong University, Xi’an 710054, Shaanxi Province, China
-
Received:2020-07-04Revised:2020-07-07Accepted:2020-08-07Online:2021-10-08Published:2021-05-22 -
Contact:Zhang Kun, Chief physician, Master’s supervisor, Department of Orthopedic Trauma, Xi’an Honghui Hospital Affiliated to Xi’an Jiaotong University, Xi’an 710054, Shaanxi Province, China -
About author:Yang Kun, Master candidate, Physician, Graduate School of Xi’an Medical University, Xi’an 710068, Shaanxi Province, China -
Supported by:the Natural Science Foundation of Shaanxi Province, No. 2017ZDXM-SF-009 (to ZK)
CLC Number:
Cite this article
Yang Kun, Fei Chen, Wang Pengfei, Zhang Binfei, Yang Na, Tian Ding, Zhuang Yan, Zhang Kun. Meta-analysis of coracoclavicular ligament reconstruction with autologous or allogeneic tendon and clavicular hook plate in the treatment of acromioclavicular joint dislocation[J]. Chinese Journal of Tissue Engineering Research, 2021, 25(28): 4580-4586.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
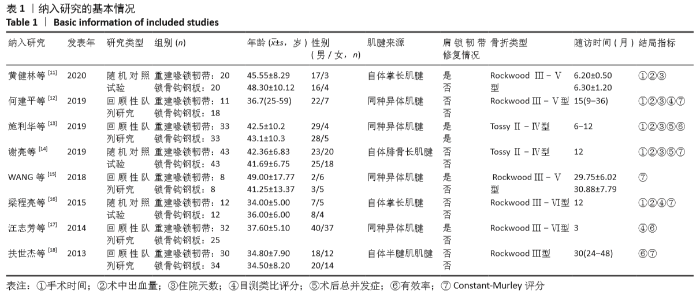
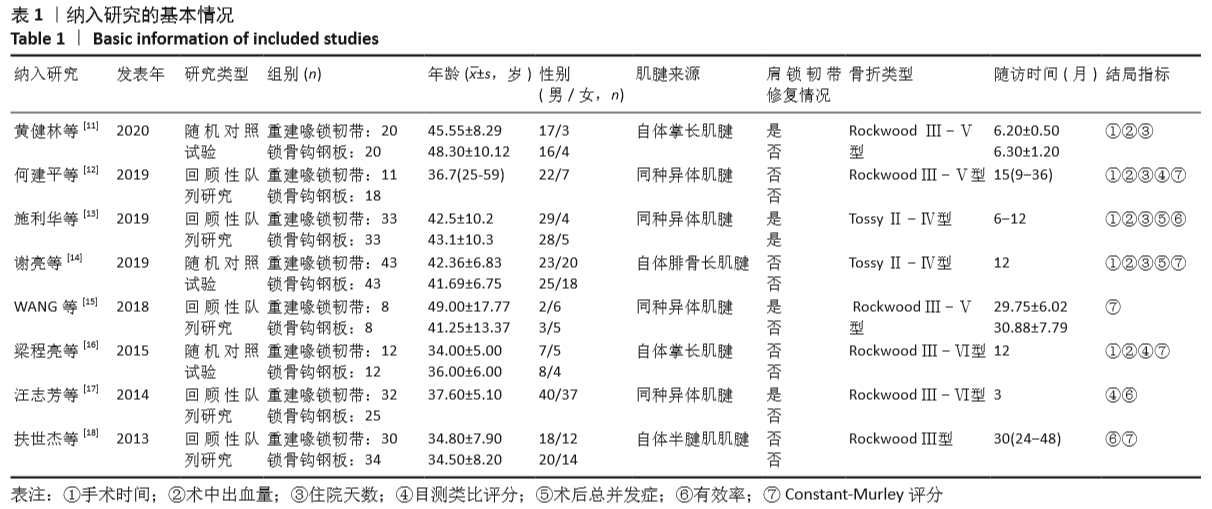
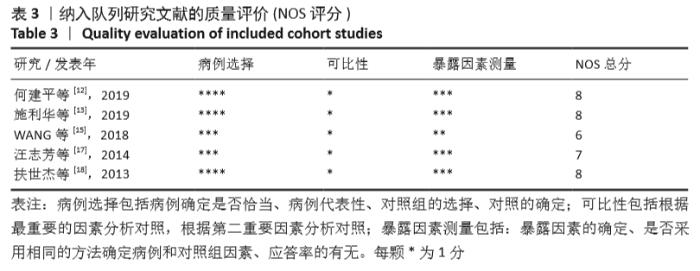
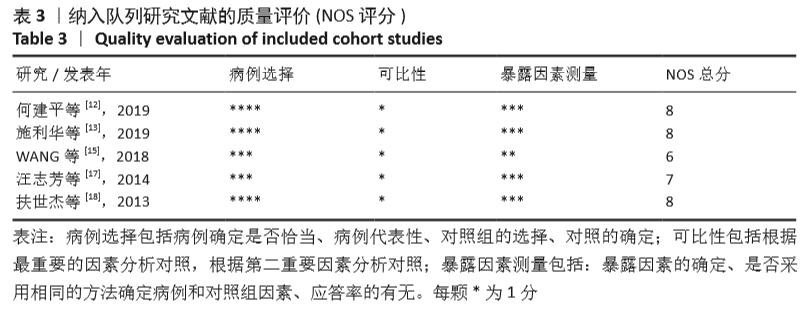
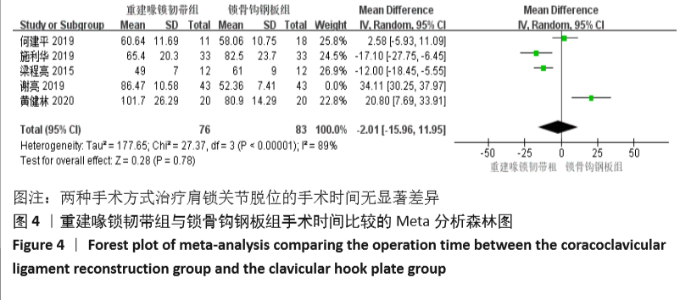
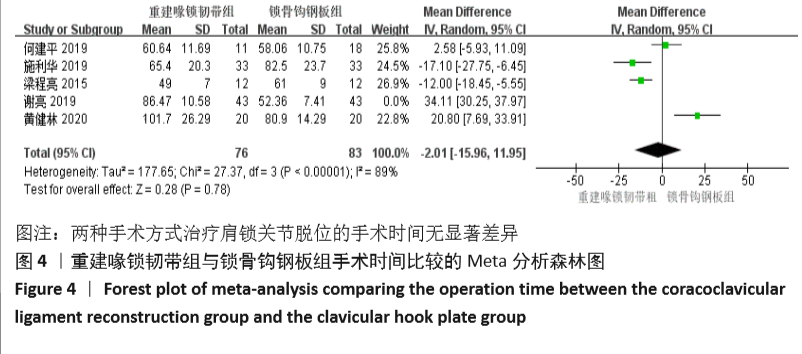
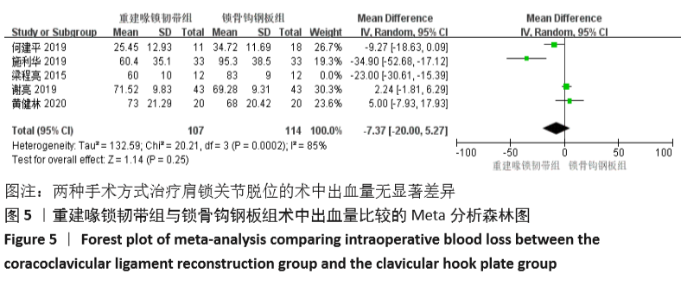
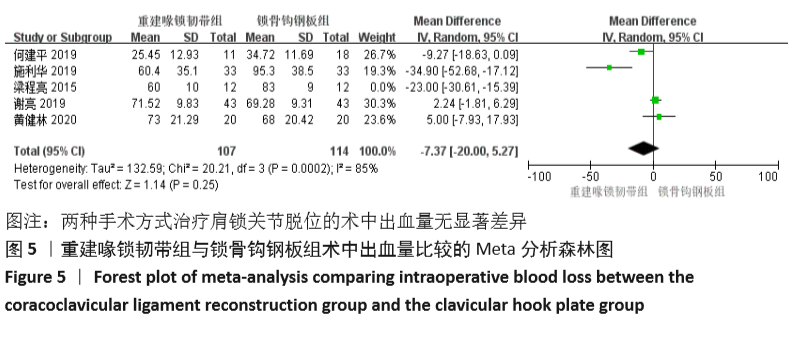
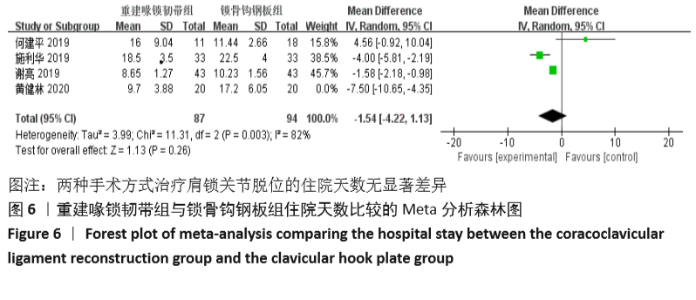
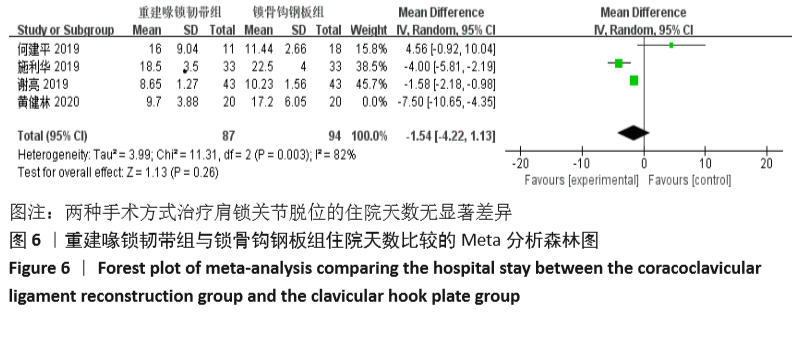
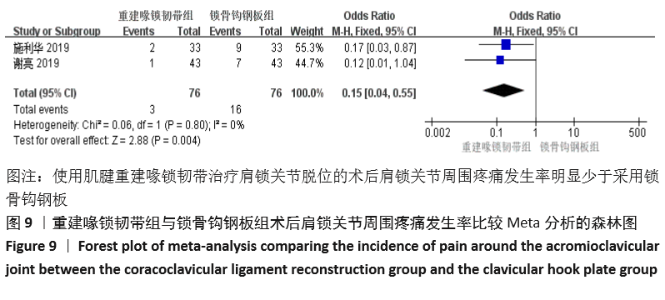
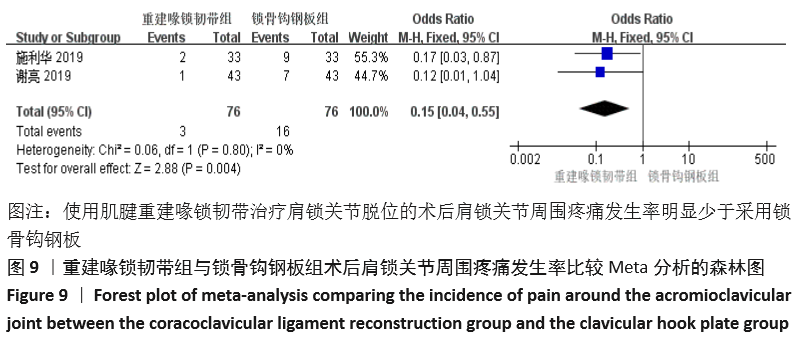
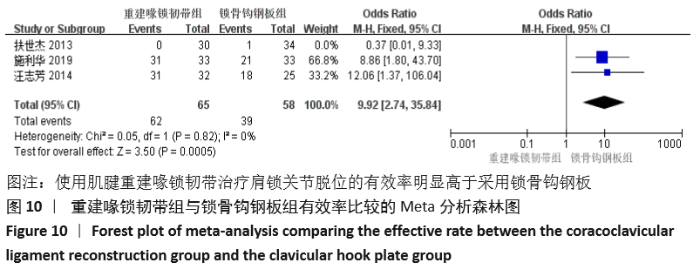
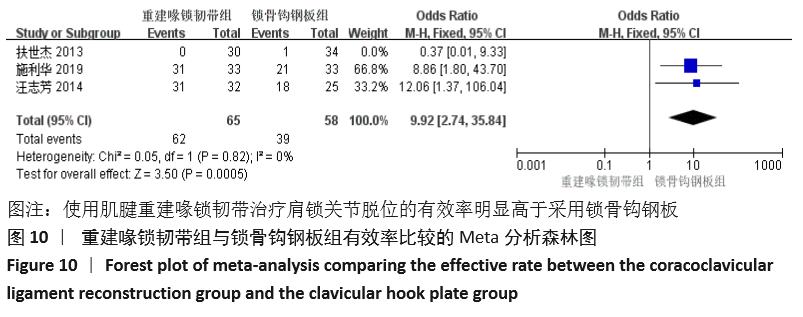
| [1] MCCREESH KM, RILEY SJ, CROTTY JM, et al. Acromio-clavicular joint cyst associated with a complete rotator cuff tear-A case report. Man Ther. 2014;19(5):490-493. [2] SHAW MBK, MCINERNEY JJ, DIAS JJ, et al. Acromioclavicular joint sprains: the post-injury recovery interval. Injury. 2003;34(6): 438-442. [3] 许福生,李桓毅,刘方刚,等.三重带袢纽扣钢板与锁骨钩钢板治疗急性肩锁关节脱位的疗效比较[J].中国矫形外科杂志,2012, 20(8):700-703. [4] FRANCESCO AD, ZOCCALI C, COLAFARINA O, et al. The use of hook plate in type III and V acromio-clavicular Rockwood dislocations: Clinical and radiological midterm results and MRI evaluation in 42 patients. Injury. 2012; 43(2):147-152. [5] 朱义用,汪建良,许科峰,等.锁骨钩钢板治疗肩锁关节脱位和锁骨远端骨折的肩痛原因分析[J].中华创伤骨科杂志,2007,9(7):692-693. [6] 傅青松,张豪,王立志,等.自体掌长肌腱与半腱肌腱重建喙锁韧带的疗效对比观察[J].实用骨科杂志,2017,23(10):930-933. [7] 赵沛,张华,张健,等.自体半腱肌肌腱重建喙锁韧带治疗肩锁关节脱位[J].中华手外科杂志,2015,31(6):427-429. [8] 王古衡,李双,陈亚兰,等.同种异体肌腱重建韧带技术与Endobutton技术治疗肩锁关节脱位的疗效比较[J].中华手外科杂志, 2020,36(2):99-102. [9] 孙伟,薛骋,李翔,等.喙锁韧带解剖重建治疗肩锁关节脱位的初步研究[J].中国矫形外科杂志,2016,24(24):2252-2256. [10] MICHLITSCH MG, ADAMSON GJ, PINK M, et al. Biomechanical comparison of a modified weaver-dunn and a free-tissue graft reconstruction of the acromioclavicular joint complex. Am J Sports Med. 2010;38(6):1196-1203. [11] 黄健林,刘文涛.掌长肌腱重建韧带与钩钢板治疗肩锁关节脱位的比较[J].实用骨科杂志,2020,26(5):447-451. [12] 何建平,朱泽兴,马东印,等.锁骨钩钢板固定与单纯同种异体肌腱重建喙锁韧带治疗肩锁关节脱位效果对比[J].实用手外科杂志,2019,33(2):199-201. [13] 施利华,李恒,郭攀,等.斜方韧带和锥状韧带走行方向对肩锁关节脱位治疗的价值[J].中国临床保健杂志,2019,22(5):660-663. [14] 谢亮,张彦祥,高博,等.自体腓骨长肌腱前侧半重建喙锁韧带与钩钢板固定治疗RockwoodⅢ-Ⅴ型肩锁关节脱位疗效观察[J].海南医学,2019,30(20):2654-2657. [15] WANG GH, XIE R, TIAN M, et al. Treatment of AC dislocation by reconstructing CC and AC ligaments with allogenic tendons compared with hook plates. J Orthop Surg Res. 2018;13(1):175. [16] 梁程亮,陈志刚,吴文健.全关节镜下自体掌长肌腱重建喙锁韧带治疗肩锁关节脱位的临床研究[J].山西医药杂志,2015,44(16): 1867-1870. [17] 汪志芳,施海伟,张黎明,等.两种不同术式治疗肩锁关节脱位的临床疗效对比研究[J].医药前沿,2014(30):18-19. [18] 扶世杰,关钛元,杨本伍,等.关节镜下自体肌腱重建与锁骨钩钢板治疗Rockwood Ⅲ型肩锁关节脱位的疗效比较[J].中华创伤骨科杂志,2013,15(10):912-914. [19] 张建华,聂宇,周永焕,等.锁骨钩钢板置入治疗Rockwood Ⅲ型肩锁关节脱位[J].中国组织工程研究,2012,16(30):5686-5690. [20] TOBY OS, RACHEL C, EYIYEMI OP, et al. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol. 2011;12(1): 19-27. [21] BALKE M, SCHNEIDER MM, AKOTO R, et al. Acute acromioclavicular joint injuries: changes in diagnosis and therapy over the last 10 years. Der Unfallchirurg. 2014;118(10):851. [22] THOMAS K, LITSKY A, JONES G, et al. Biomechanical comparison of coracoclavicular reconstructive techniques. Am J Sports Med. 2011;39(4):804. [23] COSTIC RS, LABRIOLA JE, RODOSKY MW, et al. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004; 32(8):1929. [24] JARI R, COSTIC RS, RODOSKY MW, et al. Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy. 2004;20(3):237-245. [25] LAWHORN KW, HOWELL SM. Scientific justification and technique for anterior cruciate ligament reconstruction using autogenous and allogeneic soft-tissue grafts. Orthop Clin North Am. 2003;34(1):19-30. [26] 常青,陈兴,关长勇,等.应用异体肌腱重建喙锁韧带治疗肩锁关节完全脱位[J].中国矫形外科杂志,2003,11(1):21-23. [27] 印飞,孙振中,韦旭明,等.自体及同种异体肌腱重建喙锁韧带结合钩钢板固定治疗肩锁关节脱位的疗效比较[J].中国修复重建外科杂志,2016,30(5):532-536. [28] 李传和,沈锐,秦春跃,等.改良可调式Rigidloop双钢板解剖重建喙锁韧带治疗肩锁关节脱位[J].临床骨科杂志,2019,22(4): 498-500. [29] 刘瀚忠,隋文渊,翟丽芹,等.锁骨钩钢板与Endobutton带袢钢板治疗肩锁关节脱位的疗效比较[J].中华创伤骨科杂志,2019, 21(8):710-713. [30] MILEWSKI MD, TOMPKINS M, GIUGALE JM, et al.Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40(7):1628-1634. [31] CAROFINO BC, MAZZOCCA AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19:37-46. [32] BEITZEL K, OBOPILWE E, APOSTOLAKOS J, et al. Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med. 2014; 42(9):2141-2148. [33] MAZZOCCA AD, SANTANGELO SA, Johnson ST, et al. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34(2): 236-246. [34] KOCADAL O, YüKSEL K, GüVEN M. Evaluation of the clavicular tunnel placement on coracoclavicular ligament reconstruction for acromioclavicular dislocations: a finite element analysis. Int Orthop. 2018;42(6):1891-1896. |
| [1] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [2] | Zhang Shangpu, Ju Xiaodong, Song Hengyi, Dong Zhi, Wang Chen, Sun Guodong. Arthroscopic suture bridge technique with suture anchor in the treatment of acromioclavicular dislocation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1417-1422. |
| [3] | Liang Yan, Zhao Yongfei, Xu Shuai, Zhu Zhenqi, Wang Kaifeng, Liu Haiying, Mao Keya. Imaging evaluation of short-segment fixation and fusion for degenerative lumbar scoliosis assisted by highly selective nerve root block [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1423-1427. |
| [4] | Yuan Jiawei, Zhang Haitao, Jie Ke, Cao Houran, Zeng Yirong. Underlying targets and mechanism of Taohong Siwu Decoction in prosthetic joint infection on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1428-1433. |
| [5] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [6] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [7] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [8] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [9] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [10] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [11] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [12] | Jiang Yong, Luo Yi, Ding Yongli, Zhou Yong, Min Li, Tang Fan, Zhang Wenli, Duan Hong, Tu Chongqi. Von Mises stress on the influence of pelvic stability by precise sacral resection and clinical validation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1318-1323. |
| [13] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [14] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [15] | Li Dadi, Zhu Liang, Zheng Li, Zhao Fengchao. Correlation of total knee arthroplasty efficacy with satisfaction and personality characteristics [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1346-1350. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||