[1] ARDA O, GÖKSÜGÜR N, TÜZÜN Y. Basic histological structure and functions of facial skin. Clin Dermatol. 2014;32(1):3-13.
[2] CHEN J, FAN Y, DONG G, et al. Designing biomimetic scaffolds for skin tissue engineering. Biomater Sci. 2023;11(9):3051-3076.
[3] YU JR, NAVARRO J, COBURN JC, et al. Current and Future Perspectives on Skin Tissue Engineering: Key Features of Biomedical Research, Translational Assessment, and Clinical Application. Adv Healthc Mater. 2019;8(5):e1801471.
[4] WEI Q, AN Y, ZHAO X, et al. Three-dimensional bioprinting of tissue-engineered skin: Biomaterials, fabrication techniques, challenging difficulties, and future directions: A review. Int J Biol Macromol. 2024; 266(Pt 1):131281.
[5] SHARMA Y, GHATAK S, SEN CK, et al. Emerging technologies in regenerative medicine: The future of wound care and therapy. J Mol Med. 2024;102(12):1425-1450.
[6] COSTELLO L, DICOLANDREA T, TASSEFF R, et al. Tissue engineering strategies to bioengineer the ageing skin phenotype in vitro. Aging Cell. 2022;21(2):e13550.
[7] GODOI MM, REIS EM, KOEPP J, et al. Perspective from developers: Tissue-engineered products for skin wound healing. Int J Pharm. 2024;660:124319.
[8] KANG MS, JANG J, JO HJ, et al. Advances and Innovations of 3D Bioprinting Skin. Biomolecules. 2022;13(1):55.
[9] GAO C, LU C, JIAN Z, et al. 3D bioprinting for fabricating artificial skin tissue. Colloids Surf B Biointerfaces. 2021;208:112041.
[10] KIM BS, KWON YW, KONG JS, et al. 3D cell printing of in vitro stabilized skin model and in vivo pre-vascularized skin patch using tissue-specific extracellular matrix bioink: A step towards advanced skin tissue engineering. Biomaterials. 2018;168:38-53.
[11] ZHOU F, HONG Y, LIANG R, et al. Rapid printing of bio-inspired 3D tissue constructs for skin regeneration. Biomaterials. 2020;258:120287.
[12] WU L, SONG Y. Recent innovations in interfacial strategies for DLP 3D printing process optimizatio. Mater Horiz. 2024. doi: 10.1039/d4mh01160k.
[13] ZHANG X, CHEN X, HONG H, et al. Decellularized extracellular matrix scaffolds: Recent trends and emerging strategies in tissue engineering. Bioact Mater. 2022;10:15-31.
[14] POTEKAEV NN, BORZYKH OB, MEDVEDEV GV, et al. The Role of Extracellular Matrix in Skin Wound Healing. J Clin Med. 2021;10(24): 5947.
[15] YU Y, XIAO H, TANG G, et al. Biomimetic hydrogel derived from decellularized dermal matrix facilitates skin wounds healing. Mater Today Bio. 2023;21:100725.
[16] GRANDOCH M, BOLLYKY PL, FISCHER JW. Hyaluronan: A Master Switch Between Vascular Homeostasis and Inflammation. Circ Res. 2018;122(10):1341-1343.
[17] LI J, GUAN S, SU J, et al. The Development of Hyaluronic Acids Used for Skin Tissue Regeneration. Curr Drug Deliv. 2021;18(7):836-846.
[18] PATI F, JANG J, HA DH, et al. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat Commun. 2014;5:3935.
[19] JORGENSEN AM, GORKUN A, MAHAJAN N, et al. Multicellular bioprinted skin facilitates human-like skin architecture in vivo. Sci Transl Med. 2023;15(716):eadf7547.
[21] JORGENSEN AM, MAHAJAN N, ATALA A, et al. Advances in Skin Tissue Engineering and Regenerative Medicine. J Burn Care Res. 2023; 44(Suppl_1):S33-S41.
[20] KABASHIMA K, HONDA T, GINHOUX F, et al. The immunological anatomy of the skin. Nat Rev Immunol. 2019;19(1):19-30.
[22] DERR K, ZOU J, LUO K, et al. Fully Three-Dimensional Bioprinted Skin Equivalent Constructs with Validated Morphology and Barrier Function. Tissue Eng Part C Methods. 2019;25(6):334-343.
[23] CHOGAN F, CHEN Y, WOOD F, et al. Skin Tissue Engineering Advances in Burns: A Brief Introduction to the Past, the Present, and the Future Potential. J Burn Care Res. 2023;44(Suppl_1): S1-S4.
[24] SHI Y, XING TL, ZHANG HB, et al. Tyrosinase-doped bioink for 3D bioprinting of living skin constructs. Biomed Mater. 2018;13(3):035008.
[25] DE MELO BAG, JODAT YA, CRUZ EM, et al. Strategies to use fibrinogen as bioink for 3D bioprinting fibrin-based soft and hard tissues. Acta Biomater. 2020;117:60-76.
[26] LÓPEZ DE ANDRÉS J, RODRÍGUEZ-SANTANA C, DE LARA-PEÑA L, et al.
Biofabrication of a tri-layered 3D-bioprinted CSC-based malignant melanoma model for personalized cancer treatment. Biofabrication. 2023;15(3):035016.
[27] KALOGEROPOULOU M, KRACHER A, FUCILE P, et al. Blueprints of Architected Materials: A Guide to Metamaterial Design for Tissue Engineering. Adv Mater. 2024;36(47):e2408082.
[28] FANI N, MORADI M, ZAVARI R, et al. Current Advances in Wound Healing and Regenerative Medicine. Curr Stem Cell Res Ther. 2024; 19(3):277-291.
[29] IQBAL MZ, RIAZ M, BIEDERMANN T, et al. Breathing new life into tissue engineering: exploring cutting-edge vascularization strategies for skin substitutes. Angiogenesis. 2024;27(4):587-621.
[30] LUNEVA O, OLEKHNOVICH R, USPENSKAYA M. Bilayer Hydrogels for Wound Dressing and Tissue Engineering. Polymers (Basel). 2022; 14(15):3135.
[31] ARABPOUR Z, ABEDI F, SALEHI M, et al. Hydrogel-Based Skin Regeneration. Int J Mol Sci. 2024;25(4):1982.
[32] YING H, ZHOU J, WANG M, et al. In situ formed collagen-hyaluronic acid hydrogel as biomimetic dressing for promoting spontaneous wound healing. Mater Sci Eng C Mater Biol Appl. 2019;101:487-498.
[33] HU D, WEN J, ZHAO X, et al. A wound-friendly antibacterial hyaluronic acid dressing with on-demand removability for infected wound healing. Biomater Res. 2023;27(1):38.
[34] ZHA XJ, WEN C, HUANG X, et al. Digital light processing 3D printing of high-fidelity and versatile hydrogels via in situ phase separation. J Mater Chem B. 2025;13(15):4630-4640.
[35] AJITERU O, CHOI KY, LIM TH, et al. A digital light processing 3D printed magnetic bioreactor system using silk magnetic bioink. Biofabrication. 2021;13(3):034102.
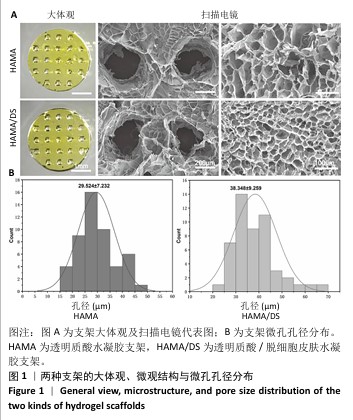
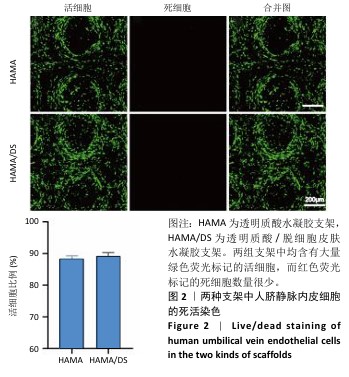
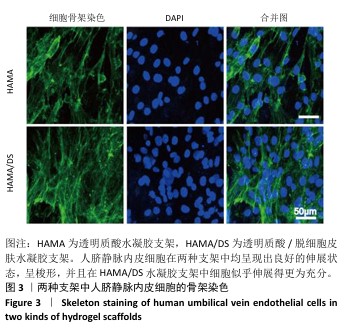
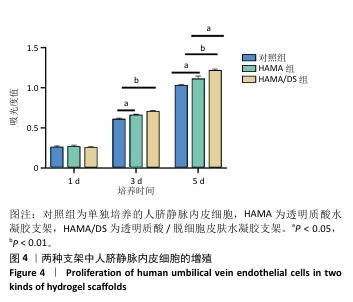
[36] 袁勋,丁振罡,付力伟,等.甲基丙烯酰化透明质酸/脱细胞华通胶水凝胶支架的制备与表征[J].中国组织工程研究,2024,28(22): 3517-3523.
[37] MCCLAIN KL, BIGENWALD C, COLLIN M, et al. Histiocytic disorders. Nat Rev Dis Primers. 2021;7(1):73.
[38] KO HC, MILTHORPE BK, MCFARLAND CD. Engineering thick tissues--the vascularisation problem. Eur Cell Mater. 2007;14:1-18;discussion 18.
[39] CHOI KY, AJITERU O, HONG H, et al. A digital light processing 3D-printed artificial skin model and full-thickness wound models using silk fibroin bioink. Acta Biomater. 2023;164:159-174.
[40] HULL SM, BRUNEL LG, HEILSHORN SC. 3D Bioprinting of Cell‐Laden Hydrogels for Improved Biological Functionality. Adv Mater. 2022;34(2): e2103691.
[41] MA N, CHEN D, LEE JH, et al. Piezo1 regulates the regenerative capacity of skeletal muscles via orchestration of stem cell morphological states. Sci Adv. 2022;8(11):eabn0485.
[42] PEÑA OA, MARTIN P. Cellular and molecular mechanisms of skin wound healing. Nat Rev Mol Cell Biol. 2024;25(8):599-616.
[43] WENG T, ZHANG W, XIA Y, et al. 3D bioprinting for skin tissue engineering: Current status and perspectives. J Tissue Eng. 2021;12: 20417314211028574.
[44] WON JY, LEE MH, KIM MJ, et al. A potential dermal substitute using decellularized dermis extracellular matrix derived bio-ink. Artif Cells Nanomed Biotechnol. 2019;47(1):644-649. |