中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (13): 2090-2097.doi: 10.12307/2024.130
• 干细胞基础实验 basic experiments of stem cells • 上一篇 下一篇
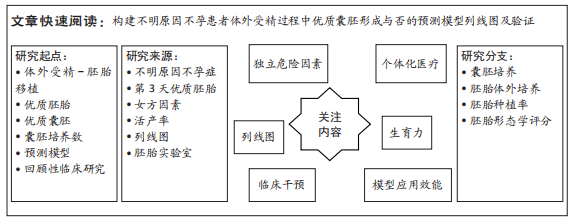
构建不明原因不孕症患者优质囊胚形成的临床预测模型列线图及验证
周 超1,蒋月园1,庾广聿1,于春梅2
- 1广西壮族自治区南溪山医院,广西壮族自治区桂林市 541000;2常州市妇幼保健院,江苏省常州市 213000
Construction of nomogram and validation of clinical prediction model for high-quality blastocyst formation in patients with unexplained infertility
Zhou Chao1, Jiang Yueyuan1, Yu Guangyu1, Yu Chunmei2
- 1Nanxishan Hospital of Guangxi Zhuang Autonomous Region, Guilin 541000, Guangxi Zhuang Autonomous Region, China; 2Changzhou Maternal and Child Health Care Hospital, Changzhou 213000, Jiangsu Province, China
摘要:
文题释义:
优质囊胚:被定义为3期及3期以上且内细胞团和滋养层评分不含C的囊胚。第3天优胚:来源于正常受精卵,且受精后第3天胚胎细胞数为7-9个、细胞大小符合发育阶段、碎片程度小于10%、无多核化的胚胎。
不明原因不孕症:是指经过排卵功能、输卵管通畅度、男方精液3个方面常规评估后并未发现病因而做出的排除性诊断。然而,实际上不明原因不孕症可能存在隐性子宫输卵管因素、潜在的卵母细胞或精子异常、受精障碍、反复胚胎种植失败等病因,但限于医疗诊断能力与医疗成本等原因而无法确诊。
背景:不明原因不孕具有较高的流产率与较低的受精率、种植率、临床妊娠率及累积活产率。临床亟待建立不明原因不孕相关临床预测模型,以解决临床预后与开展个体化医疗服务问题,并最终达到提高不明原因不孕患者累积活产率的目的。
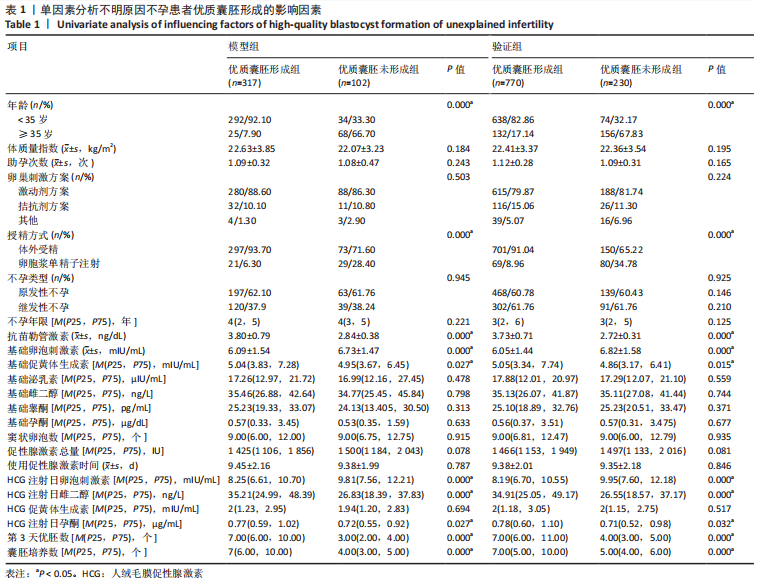
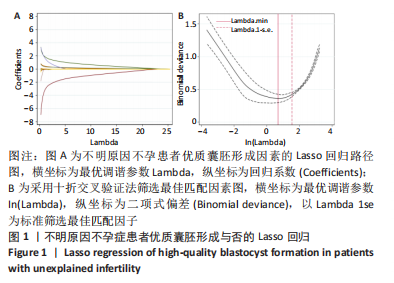
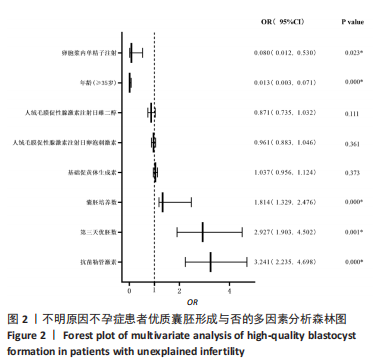
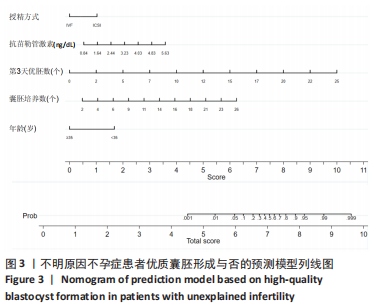
目的:构建不明原因不孕患者在体外受精过程中优质囊胚形成与否的预测模型列线图及验证。方法:回顾性分析2017年3月至2022年6月于常州妇幼保健院辅助生殖科进行体外受精的不明原因不孕患者共419例,以其中317例形成优质囊胚患者与102例未形成优质囊胚患者建立预测模型并作为模型组,通过对模型组Bootstrap法重复抽样1 000次作为验证组,首先采用单因素分析筛选不明原因不孕患者优质囊胚形成与否的影响因素,然后采用套索算法(LASSO)挑选出最佳匹配因素后,纳入多因素向前逐步Logistic回归找出其独立影响因素并绘制列线图,最后采用受试者工作曲线、校准曲线、临床决策曲线、临床影响曲线对该预测模型进行区分度与准确度及临床应用效能进行验证。
结果与结论:①单因素分析不明原因不孕患者优质囊胚形成与否的影响因素为年龄、授精方式、抗苗勒管激素水平、基础卵泡刺激素水平、基础促黄体生成素水平、人绒毛膜促性腺激素注射日卵泡刺激素水平、人绒毛膜促性腺激素注射日雌二醇水平、人绒毛膜促性腺激素注射日孕酮水平、第3天优胚数、囊胚培养数(P < 0.05);②通过LASSO回归进一步筛选出的最佳匹配因素为年龄、授精方式、抗苗勒管激素水平、基础促黄体生成素水平、人绒毛膜促性腺激素注射日卵泡刺激素水平、人绒毛膜促性腺激素注射日雌二醇水平、第3天优胚数、囊胚培养数(P < 0.05);多因素向前逐步Logistic回归结果显示年龄、授精方式、抗苗勒管激素水平、第3天优胚数、囊胚培养数为不明原因不孕患者优质囊胚形成与否的独立影响因素;③受试者工作曲线显示,模型组曲线下面积为0.880(0.834,0.926),验证组曲线下面积为0.889(0.859,0.918);说明该预测模型具有较好的区分度;校准曲线平均绝对误差为0.036,表示该模型具有较好的准确性;Hosmer-Lemeshow检验表明该模型预测形成优质囊胚的概率与实际优质囊胚形成的概率无统计学差异(P > 0.05);临床决策曲线与临床影响曲线显示,模型组与验证组分别在阈概率值为0.16-0.96与0.08-0.93时具有临床最大净获益,且在该阈概率范围内具有较好的临床应用效能。结果表明,年龄、授精方式、抗苗勒管激素水平、第3天优胚数、囊胚培养数为不明原因不孕症患者优质囊胚形成与否的独立影响因子,通过其构建的临床预测模型列线图具有较好的临床预测价值与临床应用效能,可为临床预后与干预及制定个体化医疗方案提供依据。
https://orcid.org/0000-0001-9843-6731 (周超)
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
中图分类号: