[1] 许悦,张鹏,李建虎,等.经牙槽嵴顶上颌窦底提升术中黏骨膜穿孔后同期植入种植体的短期临床效果观察[J].中国美容医学,2024, 33(12):152-155.
[2] 何逸飞,刘静,冷丹,等.超短种植体植入结合上颌窦内提升治疗上颌后牙骨量严重不足的疗效观察[J].中南医学科学杂志,2024, 52(4):653-656.
[3] 李红艳,吴德宏,秦蓉,等.不同植骨材料在侧壁开窗上颌窦底提升术中临床疗效观察[J].中华实用诊断与治疗杂志,2024,38(2):169-173.
[4] 罗梓欣,胡丹丹,耿威.上颌窦解剖特点对穿牙槽嵴上颌窦底提升手术操作的影响[J].中国口腔种植学杂志,2024,29(2):133-137.
[5] 李效宇,于欢,孟维艳.施耐德膜增厚对穿牙槽嵴上颌窦底提升影响的研究进展[J].中国口腔种植学杂志,2024,29(2):127-132.
[6] ZHAI M, CHENG H, YUAN J, et al. Nonlinear Biomechanical Characteristics of the Schneiderian Membrane: Experimental Study and Numerical Modeling. Biomed Res Int. 2018;2018:2829163.
[7] INSUA A, MONJE-GIL F, GARCÍA-CABALLERO L, et al. Mechanical characteristics of the maxillary sinus Schneiderian membrane ex vivo. Clin Oral Investig. 2018;22(3):1139-1145.
[8] DANESH-SANI SA, LOOMER PM, WALLACE SS. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. Brit J Oral Max Surg. 2016;54(7):724-730.
[9] SUGIURA T, YAMAMOTO K, HORITA S, et al. Micromotion analysis of different implant configuration, bone density, and crestal cortical bone thickness in immediately loaded mandibular full-arch implant restorations: A nonlinear finite element study. Clin Implant Dent Relat Res. 2018;20(1):43-49.
[10] GRAZIANO A, BENEDETTI L, MASSEI G, et al. Bone production by human maxillary sinus mucosa cells. J Cell Physiol. 2012;227(9):3278-3281.
[11] 陈松龄,朱双喜.上颌窦底黏膜在上颌窦底提升术后窦底空间成骨中的作用[J].口腔疾病防治,2020,28(8):477-486.
[12] CABAN J, FERMERGÅRD R, ABTAHI J. Long-term evaluation of osteotome sinus floor elevation and simultaneous placement of implants without bone grafts: 10-Year radiographic and clinical follow-up. Clin Implant Dent Relat Res. 2017;19(6):1023-1033.
[13] LIU S, CHEN S, CHEN Z, et al. Effects of Bone Grafting and Non-Bone Grafting on Implant Stability and New Bone Formation in Patients Undergoing Maxillary Sinus Floor Elevation Combined with Bicon Short Implants. Altern Ther Health Med. 2023;29(8):240-245.
[14] 周丹红,胡玲,周国栋,等.上颌窦外侧壁来源骨块在牙槽嵴水平帐篷植骨技术中的应用[J].中国口腔种植学杂志,2024,29(5):407-412.
[15] 夏海斌,徐珺怡.上颌窦底内提升同期植入种植体的研究现状[J].中国口腔种植学杂志,2024,29(2):109-117.
[16] 解孟佳,周志霖,张雅彤,等.剩余骨高度<3 mm时联合CGF与Bio-Oss骨粉行液压法上颌窦内提升术并同期种植一例[J].海南医学,2023,34(20):3008-3011.
[17] RAGUCCI GM, ELNAYEF B, SUÁREZ-LÓPEZ DEL AMO F, et al. Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review. Int J Implant Dent. 2019;5(1):6.
[18] 邹多宏,周咏.上颌窦底提升并发症的专家共识:种植体脱入上颌窦(第一版)[J].中国口腔种植学杂志,2022,27(5):264-268.
[19] 王琦,杨波,刘璐,等.不同颌骨密度下种植体设计对其骨界面应力分布影响的有限元分析[J].中国口腔种植学杂志,2024,29(2):159-168.
[20] IVANOVA V, CHENCHEV I, ZLATEV S, et al. Association between Bone Density Values, Primary Stability and Histomorphometric Analysis of Dental Implant Osteotomy Sites on the Upper Jaw. Folia Med. 2020; 62(3):563-571.
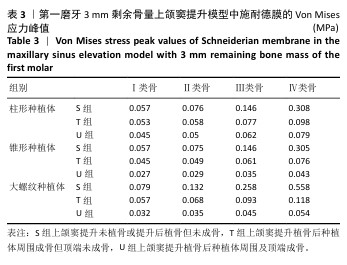
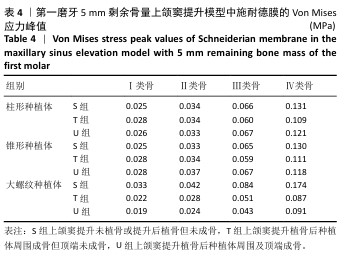
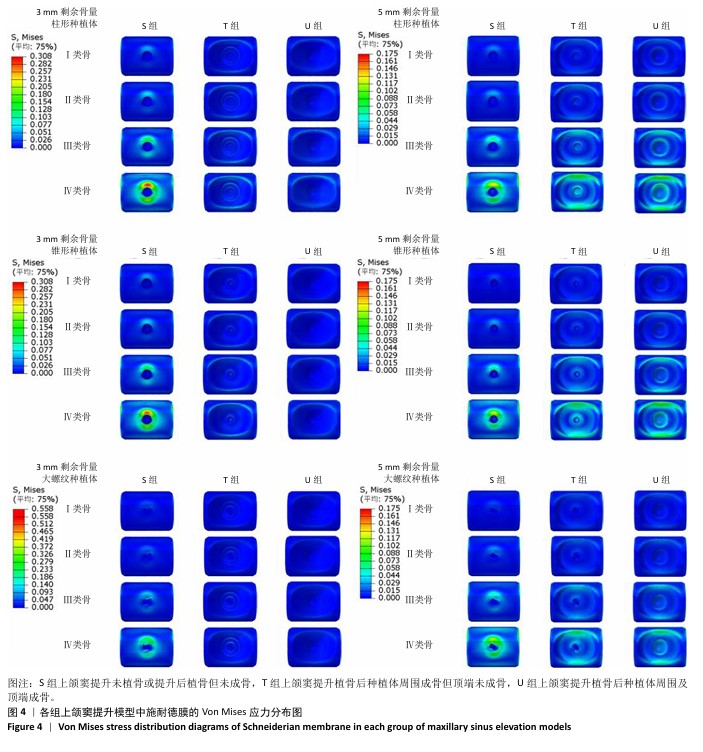
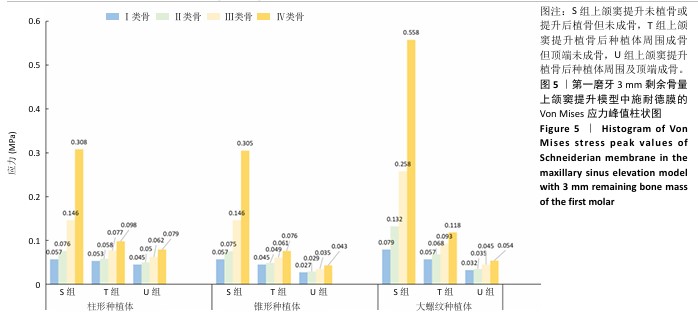
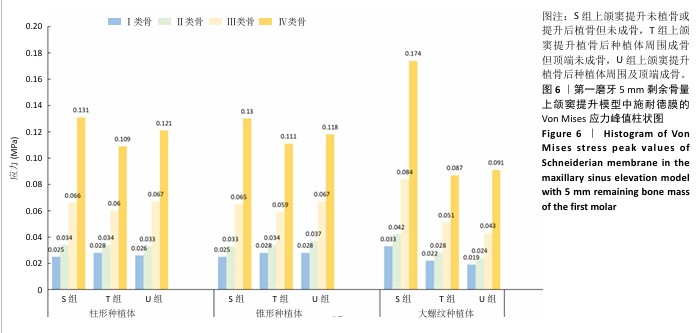
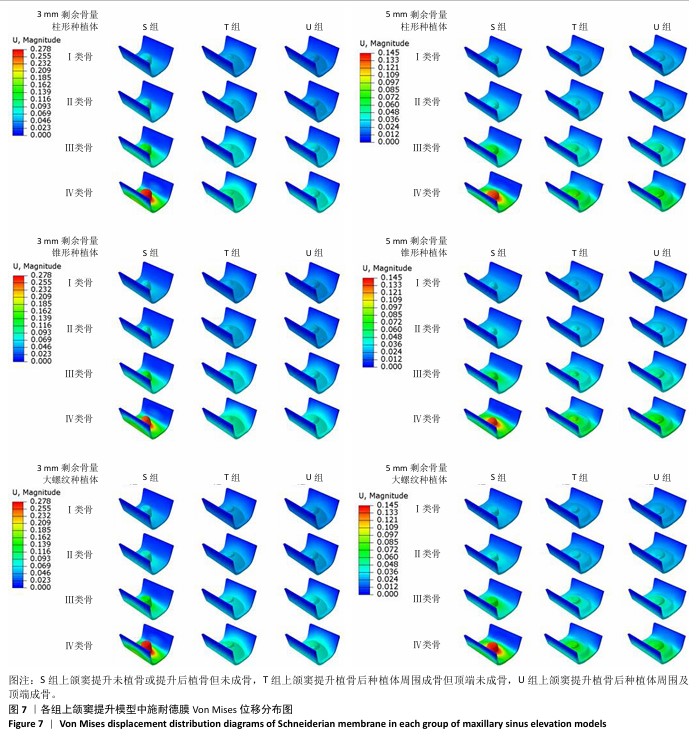
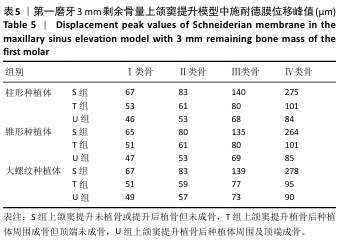
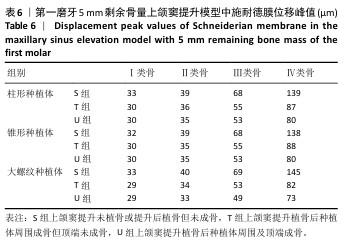
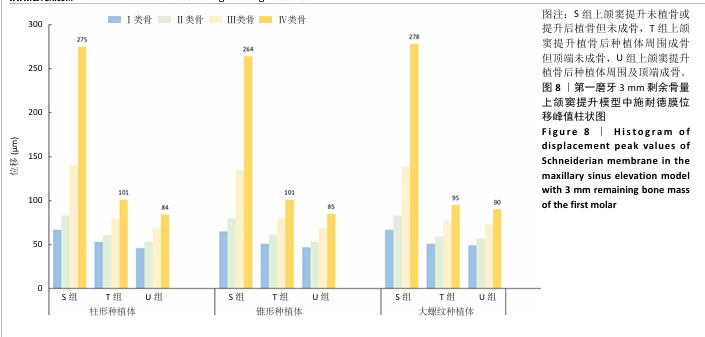
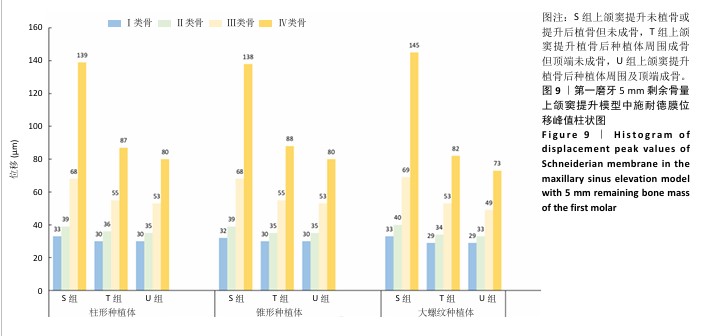
[21] 邓引昕,马攀.不同尖端形态的种植体在上颌窦底黏膜不同剥离范围时窦底黏膜的生物力学分析[J]. 口腔颌面修复学杂志,2022, 23(4):262-266,309.
[22] 徐远志,张富强,徐钦,等.上颌窦底不同位置冲顶对上颌窦内提升术影响的三维有限元分析[J].同济大学学报(医学版),2008(5):71-75.
[23] ATIF M, TEWARI N, RESHIKESH M, et al. Methods and applications of finite element analysis in dental trauma research: A scoping review. Dent Traumatol. 2024;40(4):366-388.
[24] VAIDYANATHAN AK, BANU RF. Finite element analysis - Concepts for knowledge and implementation in dental research. J Indian Prosthodont Soc. 2022;22(3): 211-214.
[25] 卓盈颖,林捷,陈睿桢,等.冠材料对种植牙应力分布影响的有限元分析[J].口腔医学,2024,44(12): 899-903.
[26] SPITZNAGEL FA, BOLDT J, GIERTHMUEHLEN PC. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J dent Res. 2018;97(10):1082-1091.
[27] MATSUURA Y, THORESON AR, ZHAO C, et al. Development of a hyperelastic material model of subsynovial connective tissue using finite element modeling. J Biomech. 2016;49(1):119-122.
[28] 侯传记,王春晔,姚健,等.糖尿病患者和非糖尿病患者上颌窦植骨6个月后成骨影像学研究[J].全科口腔医学电子杂志,2019, 6(30):22,24.
[29] 孜拉来•居来提,马吾兰江•阿不都仁木,艾克丽亚•艾尼瓦尔,等.不同骨质条件下超短种植体应用于下颌后牙区的有限元分析[J].中国组织工程研究,2025,29(22):4679-4686.
[30] OKADA D, MIURA H, SUZUKI C, et al. Stress distribution in roots restored with different types of post systems with composite resin. Dent Mater J. 2008;27(4):605-611.
[31] WALTIMO A, KÖNÖNEN M. A novel bite force recorder and maximal isometric bite force values for healthy young adults. Scand J Dent Res. 1993;101(3):171-175.
[32] 刘颜彬,罗晨晨,杨博,等.扩孔钻法经牙槽嵴顶上颌窦底提升的回顾性研究[J].北京口腔医学,2023,31(5):339-342.
[33] DENG Y, MA R, HE Y, et al. Biomechanical analysis of the maxillary sinus floor membrane during internal sinus floor elevation with implants at different angles of the maxillary sinus angles. Int J Implant Dent. 2024;10(1):11.
[34] POMMER B, UNGER E, SÜTÖ D, et al. Mechanical properties of the Schneiderian membrane in vitro. Clin Oral Implants Res. 2009;20(6): 633-637.
[35] 容明灯,周腾飞.上颌窦黏膜病变对上颌窦底提升术的影响及治疗对策[J].口腔疾病防治,2020,28(9):551-561.
[36] MERHEB J, TEMMERMAN A, RASMUSSON L, et al. Influence of Skeletal and Local Bone Density on Dental Implant Stability in Patients with Osteoporosis. Clin Implant Dent Relat Res. 2016;18(2):253-260.
[37] 蒋冰坤,宁慧影.种植区骨密度、最大扭矩值、稳定系数对牙缺失种植修复患者种植体稳定性的影响[J].临床误诊误治,2024, 37(11):95-100.
[38] 陈志敏.植骨在上颌窦内提升同期牙种植术中的临床效果观察[J].医药前沿,2023,13(5):96-98.
[39] 李敏,李大鲁.口腔种植骨增量手术中常用植骨材料的研究进展[J].山东医药,2021,61(13):100-103, 107.
[40] FENNER M, VAIRAKTARIS E, STOCKMANN P, et al. Influence of residual alveolar bone height on implant stability in the maxilla: an experimental animal study. Clin Implant Dent Relat Res. 2009;20(8):751-755.
[41] LOZANO-CARRASCAL N, SALOMÓ-COLL O, GILABERT-CERDÀ M, et al. Effect of implant macro-design on primary stability: A prospective clinical study. Med Oral Patol Oral. 2016;21(2):e214-221.
[42] HEIMES D, BECKER P, PABST A, et al. How does dental implant macrogeometry affect primary implant stability? A narrative review. Int J Implant Dent. 2023;9(1):20.
[43] BASSIR SH, EL KHOLY K, CHEN CY, et al. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. J Periodontol. 2019;90(5):493-506.
[44] POJE G, BILIĆ M, DAWIDOWSKY K, et al. Biofilm and histopathological grading of maxillary sinus mucosa in patients with antrochoanal polyps. Acta Clin Croat. 2023;62(3):406-414.
[45] WHYTE A, BOEDDINGHAUS R. The maxillary sinus: physiology, development and imaging anatomy. DEntomaxillofac Rad. 2019;48(8):20190205.
[46] TESTORI T, WEINSTEIN T, TASCHIERI S, et al. Risk factors in lateral window sinus elevation surgery. Periodontol 2000. 2019;81(1):91-123.
[47] KORESAWA K, MATSUNAGA S, HIKITA A, et al. Micro/nanostructural properties of peri-implant jaw bones: a human cadaver study. Int J Implant Dent. 2022;8:17. |