[1] LEE ZH, CRIPPS C, RODRIGUEZ ED. Current Concepts in Maxillary Reconstruction. Plast Reconstr Surg. 2022;150(1):168e-175e.
[2] 汪洋洋.单侧完全性唇腭裂患者上颌骨三维有限元模型的建立及牙槽突植骨的生物力学分析[D].南昌:南昌大学,2023.
[3] DE GROOT RJ, RIEGER JM, ROSENBERG A, et al. A pilot study of masticatory function after maxillectomy comparing rehabilitation with an obturator prosthesis and reconstruction with a digitally planned, prefabricated, free, vascularized fibula flap. J Prosthet Dent. 2020;124(5):616-622.
[4] 孙嘉怿,徐鹏,王丽珍,等.基于有限元的单侧缺损上颌骨不同修复方法的生物力学研究[J].生物医学工程学杂志,2014,31(3): 590-595+605.
[5] 毕丽霞,孙嘉怿,王燕一,等.基于有限元单侧上颌骨缺损修复材料的生物力学研究[J].医用生物力学,2014,29(1):72-77.
[6] 郑玲玲,陈丹,王涛,等.上颌骨复杂缺损3D打印精准重建支架的生物力学研究[J].医用生物力学,2022,37(6):1101-1106.
[7] HIDALGO DA. Fibula free flap: a new method of mandible reconstruction. Plastic Reconstr Surg. 1989;84(1):71-79.
[8] 王洁,王瑞霞,袁华,等.骨移植复合种植义齿进行颌骨缺损功能重建的临床研究[J].口腔医学,2013,33(12):793-795.
[9] MORRISON EJ, MATROS E. Modern Oncologic Maxillary Reconstruction. Plast Reconstr Surg. 2024;154(3):601e-618e.
[10] 李劲松,李群星.3D打印技术在颌骨精确功能性重建的应用[J].口腔疾病防治,2023,31(6):381-388.
[11] 孙坚,沈毅,李军,等.上颌骨功能性修复中骨性支柱重建的生物力学分析[J].中国口腔颌面外科杂志,2010,8(1):34-39.
[12] 陈诚,张琳梅,任文豪,等.游离腓骨瓣重建上颌骨半侧缺损数字化模拟和辅助设计[J].山西医科大学学报,2019,50(1):96-101.
[13] KHATIB B, PATEL A, DIERKS EJ, et al. The Biaxial Double-Barrel Fibula Flap-A Simplified Technique for Fibula Maxillary Reconstruction. J Oral Maxillofac Surg. 2019;77(2):412-425.
[14] 孙悦,郭蕴,李建成,等.数字化设计游离腓骨瓣重建下颌骨缺损的三维有限元分析[J].南方医科大学学报,2021,41(12):1892-1898.
[15] 热依拉·库尔班,霞黑达·依拉尔江,陈欣,等.超短种植体不同修复方式的三维有限元分析[J].中国组织工程研究,2023,27(30): 4824-4829.
[16] 李希光,郅克谦,高岭,等.基于三维有限元评价种植体不同倾斜角度在上颌后牙区骨量不足的应力分析[J].口腔医学研究,2019, 35(7):671-675.
[17] 沈毅,孙坚,李军,等.上颌骨功能性重建中用钛植入体重建颧上颌支柱的生物力学研究[J].中国口腔颌面外科杂志,2011,9(3):198-203.
[18] 焦婷,孙健,洪凌斐,等.附着体应用于单侧上颌骨缺损修复的三维有限元分析[J].上海口腔医学,2006,15(4):395-398.
[19] SUDHAN RH, CHANDER GN, ANITHA KV. Finite element stress analysis of Aramany class I maxillectomy defect with single- and two-piece closed bulb obturators. Gerodontology. 2021;38(2):209-215.
[20] 马戈.颌骨骨面植皮重建软组织种植床的可行性研究[D].西安: 第四军医大学,2011.
[21] 李兴强,李淑薇,刘长阳,等. 股前外侧皮瓣复合个性化钛网支架在上颌骨缺损修复中的应用[J]. 现代肿瘤医学,2023,31(24):4551-4554.
[22] BROWN JS, SHAW RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol. 2010;11(10):1001-1008.
[23] 吴添福,刘冰.上颌骨缺损的外科修复[J].中国实用口腔科杂志, 2021,14(5):525-530.
[24] JUNG BK, YUN IS, LEE WJ, et al. Orbital floor reconstruction using a tensor fascia lata sling after total maxillectomy. J Craniomaxillofac Surg. 2016;44(5):648-653.
[25] 赵珍珍,皇甫辉.3D打印技术在上颌骨切除术后缺损修复中的应用[J].中国眼耳鼻喉科杂志,2022,22(6):651-654.
[26] 陈健,李暐.带蒂组织瓣在头颈部肿瘤术后缺损修复重建中的应用研究进展[J].中国修复重建外科杂志,2018,32(3):369-376.
[27] 章文博,于尧,王洋,等.数字化外科技术在上颌骨缺损重建中的应用[J].北京大学学报(医学版),2017,49(1):1-5.
[28] JONES NF, SWARTZ WM, MEARS DC, et al. The “double barrel” free vascularized fibular bone graft. Plast Reconstr Surg. 1988;81(3):378-385.
[29] ANTHONY JP, FOSTER RD, SHARMA AB, et al. Reconstruction of a complex midfacialdefect with the folded fibular free flap and osseointegrated implants. Ann Plast Surg. 1996;37(2):204-210.
[30] BAJ A, YOUSSEF DA, MONTEVERDI R, et al. Reconstruction of partial maxillary defectswith the double-barrel fibula free flap. Acta Otorhinolaryngol Ital. 2010;30(6):299-302.
[31] THRESHER RW, SAITO GE. The stress analysis of human teeth. J Biomech. 1973;6(5):443-449.
[32] 许崇涛,孙庚林,周健,等.颅上颌复合体三维有限元模型的建立和初步应用[J].实用口腔医学杂志,2009,25(1):51-54.
[33] 张彤,刘洪臣,王延荣.不同功能状态下健康人上颌骨复合体应力分布的三维有限元分析[J].中华口腔医学杂志,2007,42(11):687-689.
[34] 彭歆,毛驰,俞光岩,等.游离腓骨复合组织瓣上颌骨重建的三维有限元分析[J].现代口腔医学杂志,2005,19(6):35-37.
[35] 康一帆,单小峰,张雷,等.游离腓骨瓣修复重建上颌骨术后腓骨瓣位置变化[J].北京大学学报(医学版),2020,52(5):938-942.
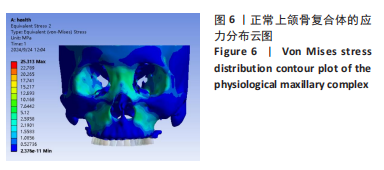
[36] 沈毅,孙坚,李军,等.正常人上颌骨的生物力学分析[J].组织工程与重建外科杂志,2009,5(1):25-28.
[37] 刘雄.下颌骨体部缺损腓骨重建小钛板固定的生物力学分析[D].广州:南方医科大学,2014.
[38] COX T, KOHN MW, IMPELLUSO T. Computerized analysis of resorbable polymer plates and screws for the rigid fixation of mandibular angle fractures. J Oral Maxillofac Surg. 2003;61(4):481-487; discussion 487-488.
[39] 刘尚萍,蔡志刚,张杰,等.下颌骨缺损重建术后钛板相关并发症97例临床回顾研究[J].中华口腔医学杂志,2013,48(10):586-590.
[40] 朱家俊.采用不同腓骨折叠及内固定方式重建下颌骨H型缺损的有限元分析[D].昆明:昆明医科大学,2023.
[41] ARBAG H, KORKMAZ HH, OZTURK K, et al. Comparative evaluation of different miniplates for internal fixation of mandible fractures using finite element analysis. J Oral Maxillofac Surg. 2008;66(6):1225-1232.
[42] 林野,王兴,毛驰,等.功能性颌骨重建61例临床分析[J].中国口腔颌面外科杂志,2006,4(1):14-19.
[43] ACAR G, ARI I, TOSUN E. Biomechanical evaluation of implant options for unilateral maxillary defects: a finite element analysis. BMC Oral Health. 2024;24(1):1338.
[44] 甄恩明,吴昌敬,邵军.双侧上颌骨缺损颧种植体修复的有限元探讨[J].中国口腔种植学杂志,2016,21(3):107-110.
[45] 李露露,孙顺涛,严洪海.种植体支持的上颌前牙两种固定修复方式在不同咬合关系下的三维有限元分析[J].口腔颌面修复学杂志,2025,26(1):14-18.
[46] 木志翔,刘婷,陈陶,等.两种上颌无牙颌种植固定修复方案的有限元分析[J].口腔医学研究,2019,35(10):931-935.
[47] BRUNSKI JB. Avoid pitfalls of overloading and micromotion of intraosseous implants. Dent Implantol Update. 1993;4(10):77-81.
[48] 李璐丽.牙种植体植入扭矩与骨结合失效分析[D].济南:山东大学,2019.
[49] 徐大鹏,景捷,马璐,等.基于种植牙愈合过程模拟上颌后牙种植体选择的生物力学分析[J]. 中国组织工程研究,2023,27(25):3942-3948.
[50] ELSAYYAD AA, ABBAS NA, ABDELNABI NM, et al. Biomechanics of 3-implant-supported and 4-implant-supported mandibular screw-retained prostheses: A 3D finite element analysis study. J Prosthet Dent. 2020;124(1):68.e1-68.e10.
[51] CENKOGLU BG, BALCIOGLU NB, OZDEMIR T, et al. The Effect of the Length and Distribution of Implants for Fixed Prosthetic Reconstructions in the Atrophic Posterior Maxilla: A Finite Element Analysis. Materials (Basel). 2019;12(16):2556.
[52] TONIOLLO MB, VIEIRA LJP, DOS SANTOS SÁ M, et al. Stress distribution of three-unit fixed partial prostheses (conventional and pontic) supported by three or two implants: 3D finite element analysis of ductile materials. Comput Methods Biomech Biomed Engin. 2019; 22(7):706-712.
[53] MEIMANDI M, TALEBI ARDAKANI MR, AMID R, et al. Comparison of Stress and Strain Distribution Around Splinted and Nonsplinted 6-mm Short Implants in Posterior Mandible: A Finite Element Analysis Study. Implant Dent. 2018;27(1):74-80.
|