中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (24): 3903-3909.doi: 10.12307/2024.610
• 骨科植入物相关临床实践 Clinical practice of orthopedic implant • 上一篇 下一篇
内侧开放楔形胫骨高位截骨后遗忘关节的预测因素
黄艺伟1,彭 波1,张 辰1,葛 昊1,黎嘉澔1,李宜金1,陈锦伦2,冯文俊2,曾意荣2
- 1广州中医药大学第一临床医学院,广东省广州市 510000;2广州中医药大学第一附属医院关节骨科,广东省广州市 510000
Predictors of a forgotten joint after medial open wedge high tibial osteotomy
Huang Yiwei1, Peng Bo1, Zhang Chen1, Ge Hao1, Li Jiahao1, Li Yijin1, Chen Jinlun2, Feng Wenjun2, Zeng Yirong2
- 1First Clinical Medical School, Guangzhou University of Chinese Medicine, Guangzhou 510000, Guangdong Province, China; 2Department of Joint Surgery, First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510000, Guangdong Province, China
摘要:
文题释义:
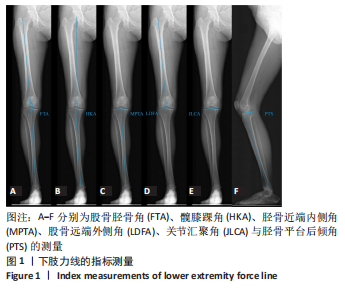
内侧开放楔形胫骨高位截骨:是治疗膝关节内侧间室骨关节炎一种有效的手术选择,通过矫正下肢力线、纠正膝关节内翻畸形使内侧间室的力线集中转移到外侧间室,可以有效改善膝关节疼痛、提高膝关节功能,最终推迟全膝关节置换手术的时间,是一种有效的保膝手术方式。遗忘关节评分:是以患者为中心,侧重于患者在日常活动和娱乐活动中对其关节置换的意识,由12个问题组成,反映了各种变量如疼痛、僵硬、日常活动及患者的术后期望。
背景:内侧开放楔形胫骨高位截骨是治疗膝关节内侧间室骨关节炎的有效保膝手段,相关研究证明相对于传统评价工具,遗忘关节评分应用于评价内侧开放楔形胫骨高位截骨具有更低的天花板效应和一致性。
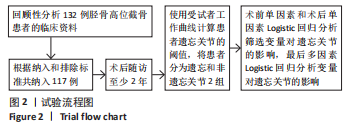
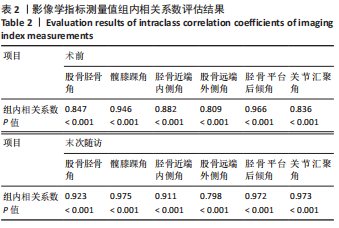
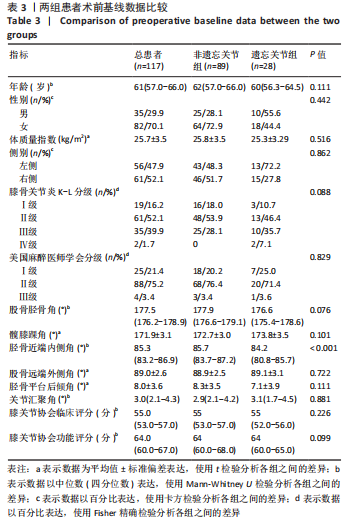
目的:探讨内侧开放楔形胫骨高位截骨后遗忘关节的预测因素。方法:选择在广州中医药大学第一附属医院进行内侧开放楔形胫骨高位截骨手术治疗的患者117例,男35例,女82例,平均年龄61岁,术后获得了至少2年的随访。通过评价患者术后是否达到遗忘关节分为遗忘关节组(n=28)和非遗忘关节组(n=89),以术前患者特征和手术相关因素为潜在预测因素,进行单变量和多变量逻辑回归分析。
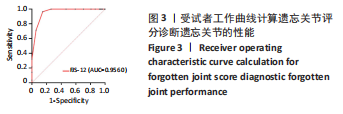
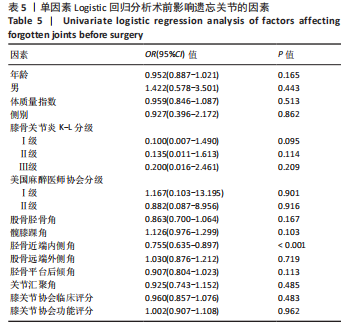
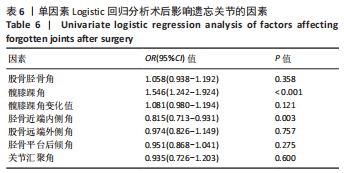
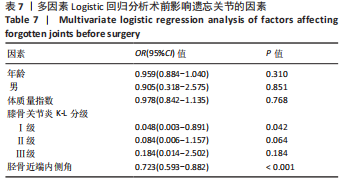
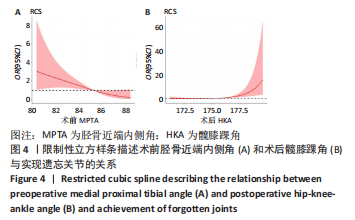
结果与结论:①两组患者术前的胫骨近端内侧角比较差异有显著性意义(P < 0.05),术后遗忘关节评分(FJS)、膝关节损伤和骨关节炎评分(KOOS)、膝关节协会功能评分和关节感知问题(PJP)比较差异均有显著性意义(P < 0.05),术后髋膝踝角和胫骨近端内侧角比较差异有显著性意义(P < 0.05);②单因素Logistic回归分析显示,术前胫骨近端内侧角对遗忘关节存在显著影响[OR=0.755,95%CI(0.635-0.897),P < 0.001],术后髋膝踝角和术后胫骨近端内侧角对遗忘关节存在显著影响[OR=1.546,95%CI(1.242-1.924),P < 0.001;OR=0.815,95%CI(0.713-0.931),P=0.003];③多因素Logistic回归分析显示,术前膝骨关节炎K-L分级为1级是获得遗忘关节的有利因素,术前胫骨近端内侧角和术后髋膝踝角是遗忘关节的独立预测因素,两者与实现遗忘关节概率呈曲线关系;当术前胫骨近端内侧角每增加1°,实现遗忘关节的概率就会减少27.7%[OR=0.723,95%CI(0.593-0.882),P < 0.001];当术后髋膝踝角每增加1°,实现遗忘关节的概率就会增加46.4%[OR=1.464,95%CI(1.153-1.860),P=0.002];④结果显示,术前膝骨关节炎K-L分级为1级、胫骨近端内侧角较小(< 85.5°)和术后髋膝踝角较大(> 176.0°)是患者实现遗忘关节的预测因素。
https://orcid.org/0000-0002-0696-0331 (黄艺伟)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: