Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (3): 460-468.doi: 10.3969/j.issn.2095-4344.2420
Previous Articles Next Articles
Risk factors for proximal junctional kyphosis after spinal deformity surgery: a meta-analysis
Zhang Jian1, 2, Wang Xiaojian2, Qin Dean2, Zhao Zhongtao2, Liang Qingyuan2, An Qijun2, Song Jiefu2
- 1Shanxi Medical University, Taiyuan 030001, Shanxi Province, China; 2People’s Hospital Affiliated to Shanxi Medical University, Taiyuan 030012, Shanxi Province, China
-
Received:2019-06-19Revised:2019-06-21Accepted:2019-07-24Online:2020-01-28Published:2019-12-27 -
Contact:Song Jiefu, Chief physician, Master’s supervisor, People’s Hospital Affiliated to Shanxi Medical University, Taiyuan 030012, Shanxi Province, China -
About author:Zhang Jian, Master candidate, Shanxi Medical University, Taiyuan 030001, Shanxi Province, China; People’s Hospital Affiliated to Shanxi Medical University, Taiyuan 030012, Shanxi Province, China -
Supported by:the National Natural Science Foundation of China, No. 8157090774; the Key Research and Development Program of Shanxi Province, No. 201803D31160; the Basic Research Project of Shanxi Province, No. 2015011121
CLC Number:
Cite this article
Zhang Jian, Wang Xiaojian, Qin Dean, Zhao Zhongtao, Liang Qingyuan, An Qijun, Song Jiefu. Risk factors for proximal junctional kyphosis after spinal deformity surgery: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(3): 460-468.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
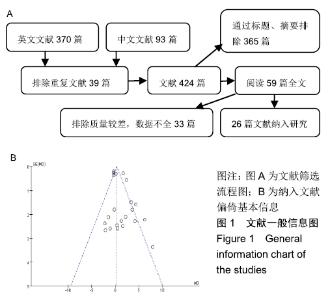
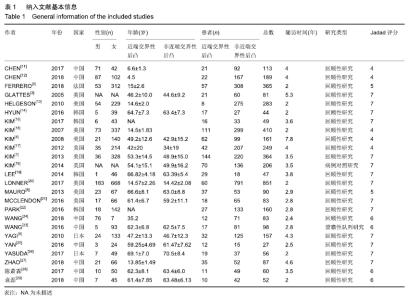
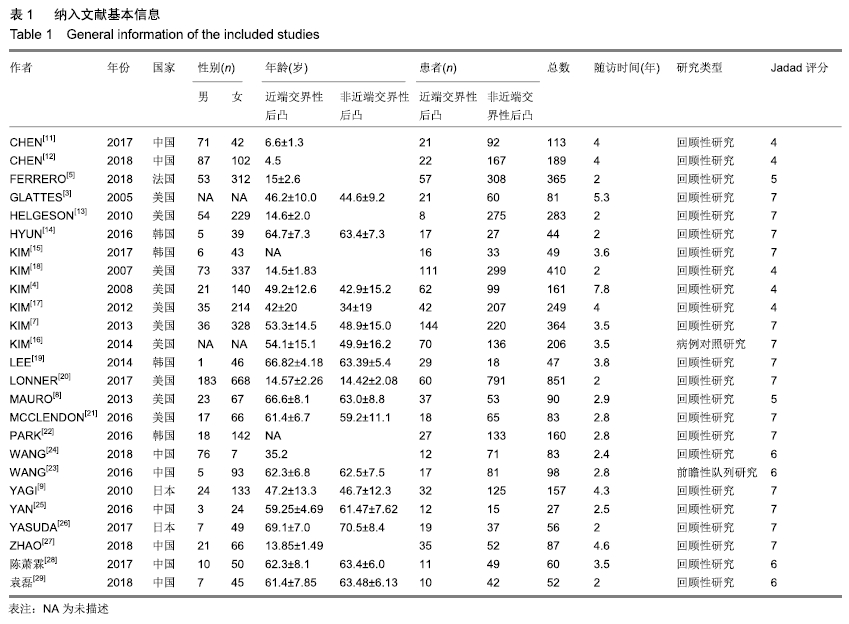
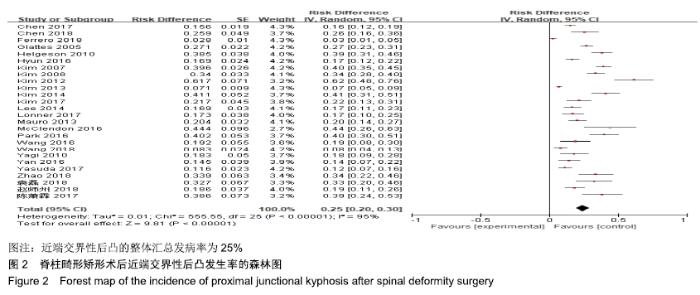
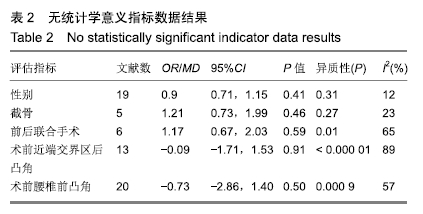
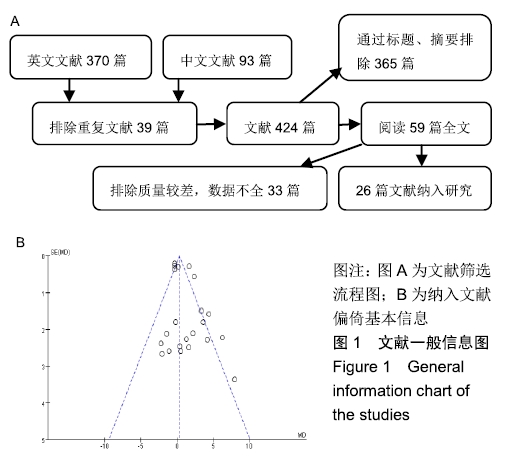
2.1 检索结果及纳入文献 2.1.1 纳入文献基本特征 根据检索词检索出英文文献共370篇,中文文献93篇。排除重复文献39篇,通过阅读标题和摘要排除338篇文献,阅读剩下的文献,排除质量较差,数据不全的文献33篇,得到26篇文献[3-5,7-9,11-30],纳入患者共计4 498例,筛选流程见图1A。评估每个纳入研究的文献质量评价为高质量文献21篇,中等质量5篇。纳入文献的基本特征见表1。 2.1.2 漏斗图偏倚分析及敏感性分析 以大部分涉及到的指标年龄为例,在近端交界性后凸组与非近端交界性后凸组的荟萃分析中,纳入的22篇文献结果大部分随机分布于漏斗图中间上部,分布基本对称,5篇研究散布在右侧95%可信区间以外,存在异质性,经过分析异质性的来源为未成年人与成年人的差异。纳入文献偏倚图见图1B,采用漏斗图评价发表偏倚。荟萃分析时,将各研究中大样本或结果差异较大的研究剔除,发现剔除后的OR值、95%CI及P值与未剔除时的结果非常接近。因此,此次荟萃分析结果基本可靠,稳定。 "
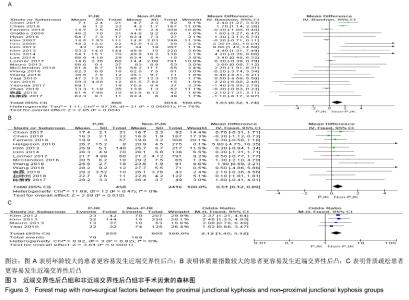
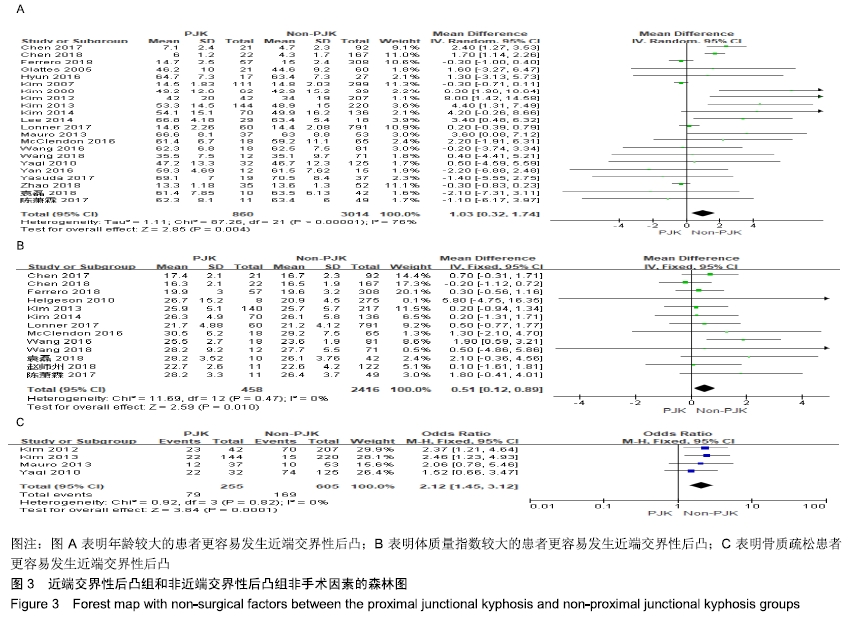
2.2.2 非手术因素 22篇研究统计了近端交界性后凸组(860例)与非近端交界性后凸组(3 014例)的年龄[3-5,7-9,11-12,14,16-21,23-29],结果显示年龄(MD=1.03,I2=76%,P < 0.1)有较大异质性,异质性来源可能为青年与成年人,但是差异有显著性意义(P < 0.05),见图3A。表明年龄较大的患者更容易发生近端交界性后凸。 13篇研究统计了近端交界性后凸组(458例)与非近端交界性后凸组(2 416例)的体质量指数[5,7,11-13,16,20-21,23-24,28-30],结果显示体质量指数(MD=0.51,I2=0%,P > 0.1)无异质性,且差异有显著性意义(P=0.01),见图3B。表明体质量指数较大的患者更容易发生近端交界性后凸。 4篇研究统计了近端交界性后凸组(255例)与非近端交界性后凸组(605例)的年龄[7-9,17],结果显示骨质疏松情况(OR=2.12,I2=0%,P > 0.1)无异质性,差异有显著性意义(P < 0.05),见图3C。表明骨质疏松患者更容易发生近端交界性后凸。 "
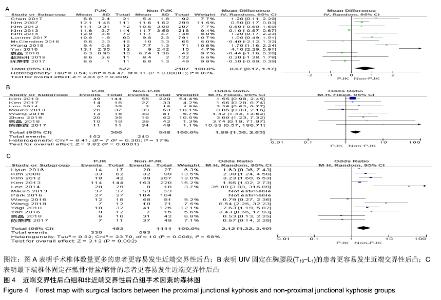
2.2.3 手术因素 12篇研究统计了近端交界性后凸组(522例)与非近端交界性后凸组(2 107例)的手术椎体数 量[7,11,16-18,20-21,24-25,28-30],结果显示手术椎体数量情况(MD=0.67,I2=80%,P < 0.1)具有较大异质性,差异有显著性意义(P=0.008),见图4A。表明长节段固定,手术椎体数量更多的患者更容易发生近端交界性后凸。 8篇研究统计了近端交界性后凸组(300例)与非近端交界性后凸组(548例)的UIV固定在胸腰段(T10-L1)的患者数量[7-8,15,19,23,27-29],结果显示数量情况(OR=1.89,I2=17%,P > 0.1)有较小异质性,差异有显著性意义(P < 0.05),见图4B。表明UIV固定在胸腰段(T10-L1)的患者更容易发生近端交界性后凸。 13篇研究统计了近端交界性后凸组(453例)与非近端交界性后凸组(1 111例)的最下端椎体固定在骶骨/骨盆/髂骨的患者数量[4,7-9,14, 16-17,19,2-25,28-29],结果显示(OR=2.12,I2=58%,P < 0.1)有较大异质性,差异有显著性意义(P=0.002),见图4C。表明最下端椎体固定在骶骨/骨盆/髂骨的患者更容易发生近端交界性后凸。 "
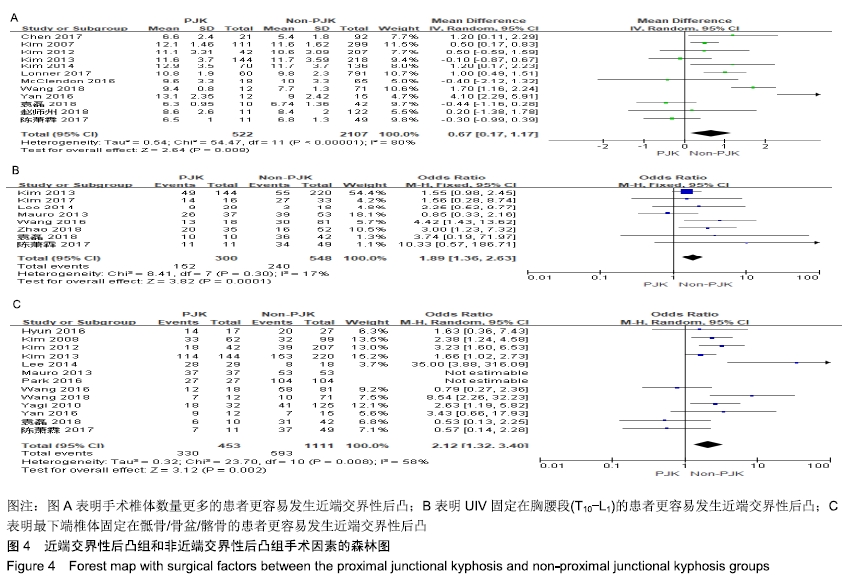

2.2.4 手术相关影像测量指标因素 13篇研究统计了近端交界性后凸组(418例)与非近端交界性后凸组(1 393例)的术后近端交界区后凸角[4,8-9,11-12,17-18,24-25, 27-30],结果显示术后近端交界区后凸角(MD=11.02,I2=89%,P < 0.1)有较大异质性,差异有显著性意义(P < 0.05),见图5A。表明术后近端交界区后凸角较大的患者更容易发生近端交界性后凸。 19篇研究统计了近端交界性后凸组(551例)与非近端交界性后凸组(2 436例)的术后腰椎前凸角[4-5,8-9,11-12,14,16,20-30],结果显示术后腰椎前凸角(MD=3.21,I2=72%,P < 0.1)有较大异质性,差异有显著性意义(P=0.003),见图5B。表明术后腰椎前凸角较大的患者更容易发生近端交界性后凸。 16篇研究统计了近端交界性后凸组(392例)与非近端交界性后凸组(1 108例)的术后矢状面垂直偏移[3-4,8-9,11-12,14,19,21-27,29],结果显示术后矢状面垂直偏移(MD=8.42,I2=51%,P < 0.1)有较大异质性,差异有显著性意义(P < 0.05),见图5C。表明术后矢状面垂直偏移较大的患者更容易发生近端交界性后凸。 "
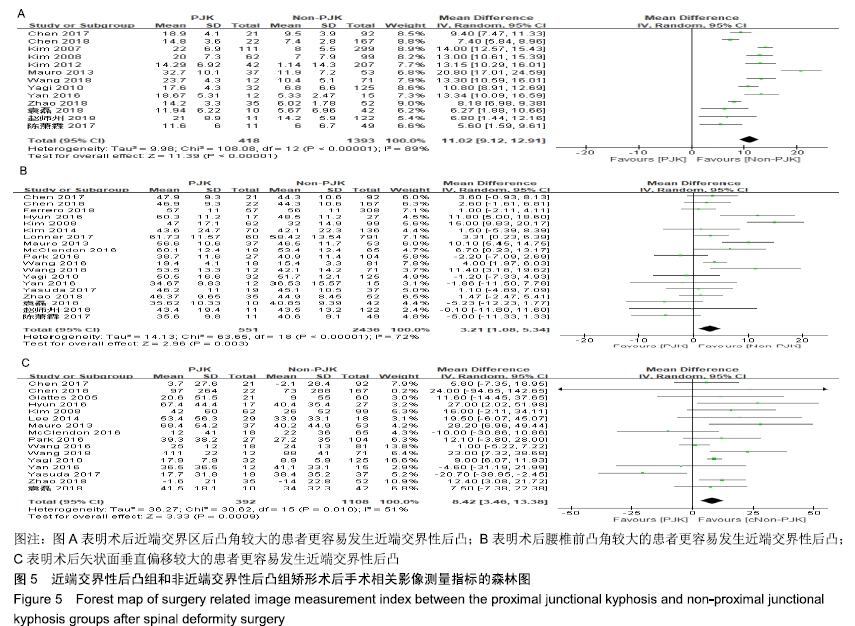
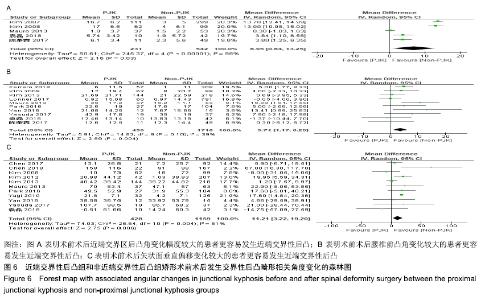
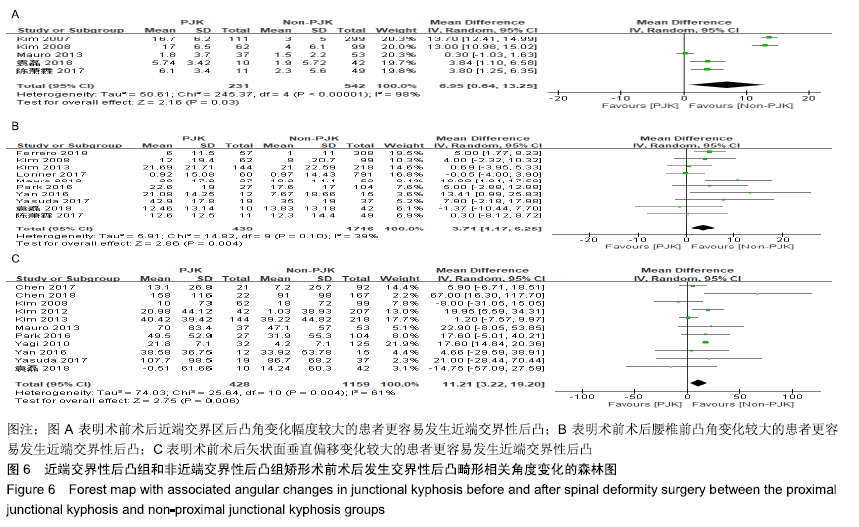
5篇研究统计了近端交界性后凸组(231例)与非近端交界性后凸组(542例)的术前术后近端交界区后凸角变化[4,8,18,28-29],结果显示术前术后近端交界区后凸角变化(MD=6.95,I2=98%,P < 0.1)有较大异质性,差异有显著性意义(P=0.03),见图6A。表明术前术后近端交界区后凸角变化幅度较大的患者更容易发生近端交界性后凸。 10篇研究统计了近端交界性后凸组(439例)与非近端交界性后凸组(1 716例)的术前术后腰椎前凸角变化[4-5,7-8,20,22,25-26,28-29],结果显示术前术后腰椎前凸角变化(MD=3.71,I2=39%,P=0.1)有较小异质性,差异有显著性意义(P=0.004),见图6B。表明术前术后腰椎前凸角变化较大的患者更容易发生近端交界性后凸。 11篇研究统计了近端交界性后凸组(428例)与非近端交界性后凸组(1 159例)的术前术后矢状面垂直偏移变化[4,7-9,11-12,17, 22,25-26,29],结果显示术前术后矢状面垂直偏移变化(MD=11.21,I2=61%,P < 0.1)有较大异质性,差异有显著性意义(P=0.006),见图6C。表明术前术后矢状面垂直偏移变化较大的患者更容易发生近端交界性后凸。 "
| [1] SCHEER JK, FAKURNEJAD S, LAU D, et al. Results of the 2014 SRS Survey on PJK/PJF: a report on variation of select srs member practice patterns, treatment indications, and opinions on classification development. Spine (Phila Pa 1976). 2015;40: 829-840. [2] CAMMARATA M, AUBIN CE, WANG X, et al. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976). 2014;39: E500-507. [3] GLATTES RC, BRIDWELL KH, LENKE LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 2005; 30: 1643-1649. [4] KIM YJ, BRIDWELL KH, LENKE LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008; 33: 2179-2184. [5] FERRERO E, BOCAHUT N, LEFEVRE Y, et al. Proximal junctional kyphosis in thoracic adolescent idiopathic scoliosis: risk factors and compensatory mechanisms in a multicenter national cohort. Eur Spine J. 2018; 27: 2241-2250. [6] LIU FY, WANG T, YANG SD, et al. Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J. 2016; 25: 2376-2383. [7] KIM HJ, BRIDWELL KH, LENKE LG, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976). 2013; 38: 896-901. [8] MARUO K, HA Y, INOUE S, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 2013;38: E1469-1476. [9] YAGI M, AKILAH KB, BOACHIE-ADJEI O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36: E60-68. [10] JADAD AR, MOORE RA, CARROLL D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17: 1-12. [11] CHEN X, CHEN ZH, QIU Y, et al. Proximal junctional kyphosis after posterior spinal instrumentation and fusion in young children with congenital scoliosis: a preliminary report on its incidence and risk factors. Spine (Phila Pa 1976). 2017;42: E1197-1203. [12] CHEN X, XU L, QIU Y, et al. Incidence, risk factors, and evolution of proximal junctional kyphosis after posterior hemivertebra resection and short fusion in young children with congenital scoliosis. Spine (Phila Pa 1976). 2018; 43: 1193-1200. [13] HELGESON MD, SHAH SA, NEWTON PO, et al. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine (Phila Pa 1976). 2010;35: 177-181. [14] HYUN SJ, KIM YJ, RHIM SC. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016;16: 1095-1101. [15] KIM DK, KIM JY, KIM DY, et al. Risk factors of proximal junctional kyphosis after multilevel fusion surgery: more than 2 years follow-up data. J Korean Neurosurg Soc. 2017;60: 174-180. [16] KIM HJ, BRIDWELL KH, LENKE LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976). 2014;39: E576-580. [17] KIM HJ, YAGI M, NYUGEN J, et al. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res. 2012;470: 1633-1639. [18] KIM YJ, LENKE LG, BRIDWELL KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976). 2007; 32: 2731-2738. [19] LEE JH, KIM JU, JANG JS, et al. Analysis of the incidence and risk factors for the progression of proximal junctional kyphosis following surgical treatment for lumbar degenerative kyphosis: minimum 2-year follow-up. Br J Neurosurg. 2014;28: 252-258. [20] LONNER BS, REN Y, NEWTON PO, et al. Risk factors of proximal junctional kyphosis in adolescent idiopathic scoliosis-the pelvis and other considerations. Spine Deform. 2017;5: 181-188. [21] MCCLENDON J JR, SMITH TR, SUGRUE PA, et al. Spinal implant density and postoperative lumbar lordosis as predictors for the development of proximal junctional kyphosis in adult spinal deformity. World Neurosurg. 2016;95: 419-424. [22] PARK SJ, LEE CS, CHUNG SS, et al. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. 2017;80: 279-286. [23] WANG H, MA L, YANG D, et al. Incidence and risk factors for the progression of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion. Medicine (Baltimore). 2016; 95: e4443. [24] WANG T, ZHAO Y, LIANG Y, et al. Risk factor analysis of proximal junctional kyphosis after posterior osteotomy in patients with ankylosing spondylitis. J Neurosurg Spine. 2018; 29: 75-80. [25] YAN P, BAO H, QIU Y, et al. Mismatch Between Proximal Rod Contouring and Proximal Junctional Angle: A Predisposed Risk Factor for Proximal Junctional Kyphosis in Degenerative Scoliosis. Spine (Phila Pa 1976). 2017; 42: E280-e287. [26] YASUDA T, HASEGAWA T, YAMATO Y, et al. Proximal junctional kyphosis in adult spinal deformity with long spinal fusion from T9/T10 to the ilium. J Spine Surg. 2017; 3: 204-211. [27] ZHAO J, YANG M, YANG Y, et al. Proximal junctional kyphosis following correction surgery in the Lenke 5 adolescent idiopathic scoliosis patient. J Orthop Sci. 2018;23: 744-749. [28] 陈萧霖,曾岩,陈仲强,等.退变性腰椎侧凸后路长节段固定融合术后近端交界性后凸的危险因素分析[J]. 中国脊柱脊髓杂志, 2017,27(7):612-621. [29] 袁磊,陈萧霖,曾岩,等.退变性腰椎侧凸患者椎旁肌退变与术后近端交界性后凸的相关性研究[J].中国脊柱脊髓杂志, 2018,28(5):425-433. [30] 赵师州,钱邦平,邱勇.强直性脊柱炎胸腰椎后凸畸形截骨矫形术后近端交界性后凸的危险因素与临床意义[J].中国脊柱脊髓杂志, 2018, 28(8): 675-681. [31] LAU D, CLARK AJ, SCHEER JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976). 2014; 39: 2093-2102. [32] O'LEARY PT, BRIDWELL KH, LENKE LG, et al. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976). 2009; 34: 2134-2139. [33] KEBAISH KM, MARTIN CT, O'BRIEN JR, et al. Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J. 2013;13: 1897-1903. [34] BRIDWELL KH, LENKE LG, CHO SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery. 2013;72: 899-906. [35] ANNIS P, LAWRENCE BD, SPIKER WR, et al. Predictive factors for acute proximal junctional failure after adult deformity surgery with upper instrumented vertebrae in the thoracolumbar spine. Evid Based Spine Care J. 2014; 5: 160-162. [36] HA Y, MARUO K, RACINE L, et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine. 2013;19: 360-369. [37] ZHU Z, TANG NL, XU L, et al. Genome-wide association study identifies new susceptibility loci for adolescent idiopathic scoliosis in Chinese girls. Nat Commun. 2015; 6: 8355. [38] HART RA, PRENDERGAST MA, ROBERTS WG, et al. Proximal junctional acute collapse cranial to multi-level lumbar fusion: a cost analysis of prophylactic vertebral augmentation. Spine J. 2008;8: 875-881. [39] 郑波,王飞,张志成,等.近端交界性后凸的危险因素分析[J].中国康复理论与实践,2017, 23(5): 607-611. [40] BRIDWELL KH, GLASSMAN S, HORTON W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976). 2009;34: 2171-2178. [41] MASEVNIN S, PTASHNIKOV D, MICHAYLOV D, et al. Risk factors for adjacent segment disease development after lumbar fusion. Asian Spine J. 2015; 9: 239-244. |
| [1] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Zhang Yu, Tian Shaoqi, Zeng Guobo, Hu Chuan. Risk factors for myocardial infarction following primary total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1340-1345. |
| [4] | Wang Haiying, Lü Bing, Li Hui, Wang Shunyi. Posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis: prediction of functional prognosis of patients based on spinopelvic parameters [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1393-1397. |
| [5] | Zhang Chao, Lü Xin. Heterotopic ossification after acetabular fracture fixation: risk factors, prevention and treatment progress [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1434-1439. |
| [6] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [7] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [8] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [9] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [10] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [11] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [12] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [13] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [14] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [15] | Huang Youyi, Yuan Wei. Application of 3D printing technology in fracture and deformity of foot and ankle [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 438-442. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||