Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (3): 453-459.doi: 10.3969/j.issn.2095-4344.2419
Previous Articles Next Articles
Comparison of seven surgical interventions for lumbar disc herniation: a network meta-analysis#br#
Feng Fan1, Cai Yi1, Li Yingbo1, Dong Junli1, Wu Qun1, Fan Yongzhi1, Yan Hong2
- 1Department of Pain, 2Department of Anesthesiology, the Central Hospital of Wuhan, Huazhong University of Science and Technology, Wuhan 430014, Hubei Province, China
-
Received:2019-01-02Revised:2019-01-11Accepted:2019-03-12Online:2020-01-28Published:2019-12-27 -
Contact:Fan Yongzhi, Associate chief physician, Department of Pain, the Central Hospital of Wuhan, Huazhong University of Science and Technology, Wuhan 430014, Hubei Province, China Yan Hong, Chief physician, Department of Anesthesiology, the Central Hospital of Wuhan, Huazhong University of Science and Technology, Wuhan 430014, Hubei Province, China -
About author:Feng Fan, Master, Department of Pain, the Central Hospital of Wuhan, Huazhong University of Science and Technology, Wuhan 430014, Hubei Province, China
CLC Number:
Cite this article
Feng Fan, Cai Yi, Li Yingbo, Dong Junli, Wu Qun, Fan Yongzhi, Yan Hong. Comparison of seven surgical interventions for lumbar disc herniation: a network meta-analysis#br#[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(3): 453-459.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
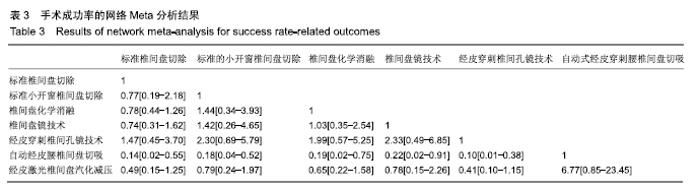
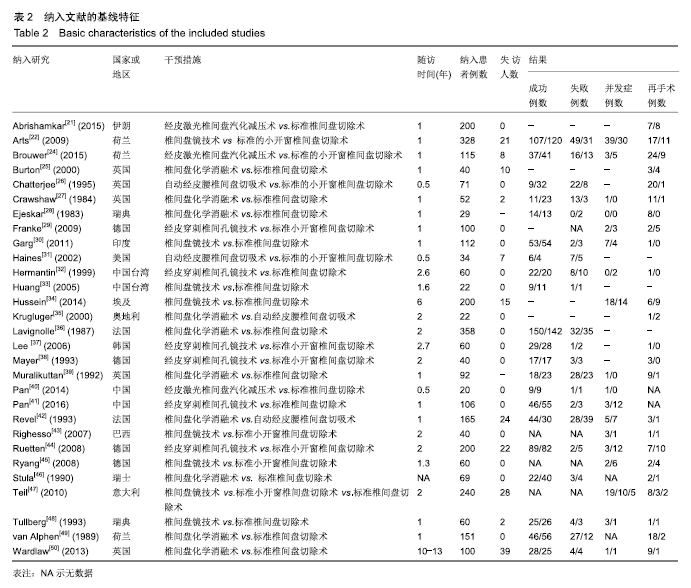
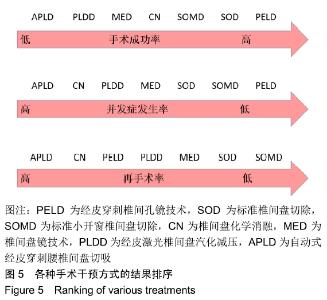
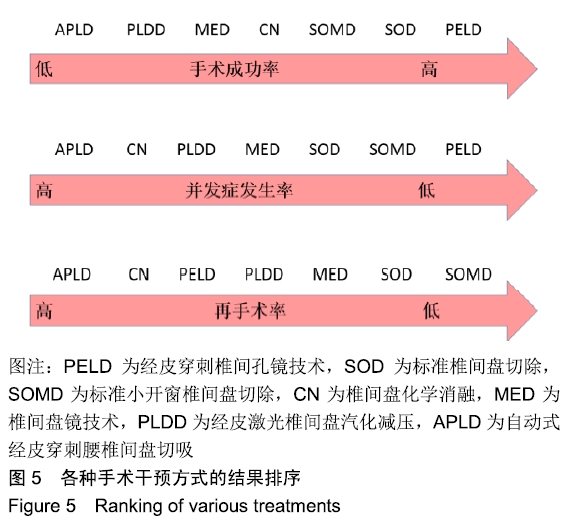
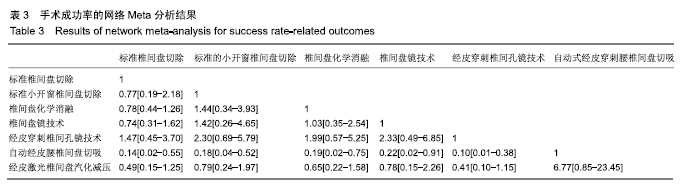
2.3 有效性结果:手术成功率 一共有762例患者接受了标准椎间盘切除术,237例接受了标准小开窗椎间盘切除术,406例接受了椎间盘化学消融术,250例接受了椎间盘镜手术,219例接受了经皮穿刺椎间孔镜手术,41例自动式经皮穿刺腰椎间盘切吸术,132例经皮激光椎间盘汽化减压术。相比于标准椎间盘切除手术,经皮穿刺椎间孔镜手术患者(OR=1.47,95%CI:0.45-3.70)的手术成功率最高。紧随其后的是椎间盘化学消融术(OR=0.78,95%CI:0.44-1.26)、标准小开窗椎间盘切除术(OR=0.77,0.19-2.18)、经皮激光椎间盘汽化减压术(OR=0.49,95%CI:0.15-1.25)以及自动式经皮穿刺腰椎间盘切吸术(OR=0.14,95%CI:0.02-0.55)。各组之间的详细对比见表3。"
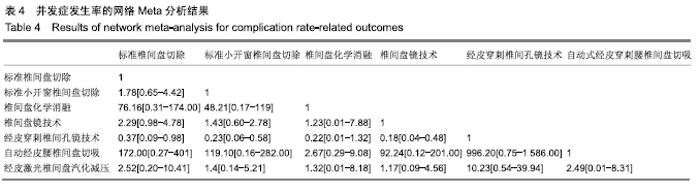
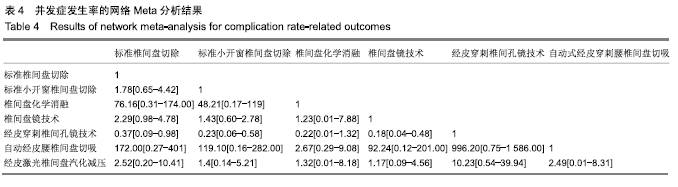
2.4 安全性结果:手术并发症风险 一共纳入460例接受标准椎间盘切除的患者,461例接受标准小开窗椎间盘切除术,188例接受椎间盘化学消融术,456例接受椎间盘镜技术,221例接受经皮穿刺椎间孔镜技术,69例接受自动式经皮穿刺腰椎间盘切吸术,63例接受经皮激光椎间盘汽化减压术。相比于标准椎间盘切除术,自动式经皮穿刺腰椎间盘切吸患者(OR=172,95%CI:0.27-401.00)的手术并发症发生率最低,随后是椎间盘化学消融术(OR=76.16,95%CI:0.31-174.00)、经皮激光椎间盘汽化减压术(OR=2.52,95%CI:0.20-10.41)、椎间盘镜技术(OR=2.29,95%CI:0.98-4.78)、标准的小开窗椎间盘切除术(OR=1.78,95%CI:0.65-4.24)和经皮穿刺椎间孔镜技术(OR=0.37,95%CI:0.09-0.98)。各组之间详细对比见表4。"
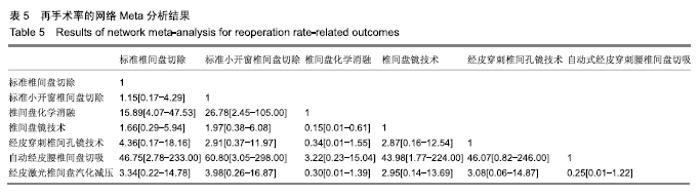
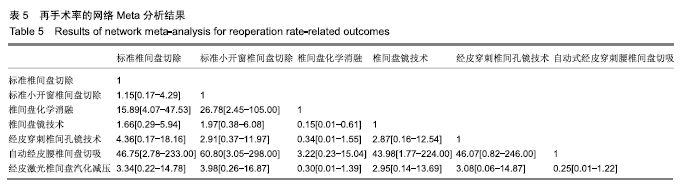
2.5 其他结果:再手术风险 一共纳入559例接受标准椎间盘切除的患者,551例接受标准小开窗椎间盘切除术,313例接受椎间盘化学消融术,456例接受椎间盘镜技术,223例接受经皮穿刺椎间孔镜技术,110例接受自动式经皮穿刺腰椎间盘切吸术,153例接受经皮激光椎间盘汽化减压术。相比于标准的标准椎间盘切除术,自动式经皮穿刺腰椎间盘切吸患者(OR=46.75,95%CI:2.78-233.00)的再手术率最低,随后是椎间盘化学消融术(OR=15.89,95%CI:4.07-47.53)、经皮穿刺椎间孔镜技术(OR=4.36,95%CI:0.17-18.16)、经皮激光椎间盘汽化减压术(OR=3.34, 95%CI:0.22-14.78)、椎间盘镜技术(OR=1.66,95%CI:0.29-5.95)和标准小开窗椎间盘切除术(OR=1.15,95%CI:0.17-4.29)。各组之间详细对比见表5。"
| [1] FRITSCH EW, HEISEL J, RUPP S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine. 1996;21:626-633. [2] GIBSON JN, COWIE JG, IPRENBURG M. Transforaminal endoscopic spinal surgery: the future 'gold standard' for discectomy? A review. Surgeon. 2012;10:290-296. [3] GIBSON JN, WADDELL G. Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine. 2007;32:1735-1747. [4] CONG L, ZHU Y, TU G. A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur Spine J. 2016; 25:134-143. [5] BLAMOUTIER A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res. 2013;99(1 Suppl):S187-196. [6] MIXTER WJ, BARR JS. Rupture of the intervertebral disc with involvement of the spinal canal. New Eng J Med. 1934;211:205-210. [7] BOKOV A, ISRELOV A, SKORODUMOV A, et al. An analysis of reasons for failed back surgery syndrome and partial results after different types of surgical lumbar nerve root decompression. Pain Physician. 2011;14:545-557. [8] YASARGIL M. Microsurgical operation of herniated lumbar disc. Adv Neurosurg.1977;4:81-82. [9] CASPAR W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. Adv Neurosurg. 1977;4:74-77. [10] VALAT JP, GENEVAY S, MARTY M, et al. Sciatica. Best Pract Res Clin Rheumatol. 2010;24(2):241-252. [11] FOLEY M. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301-307. [12] SMITH L. Enzyme dissolution of the nucleus pulposus in humans. JAMA. 1964;187:137-140. [13] ONIK G, HELMS CA, GINSBURG L, et al. Percutaneous lumbar diskectomy using a new aspiration probe. AJR Am J Roentgenol.1985;144(6): 1137-1140. [14] CHOY DS, ASCHER P, LAMMER J, et al. Percutaneous laser catheter recanalization of carotid arteries in seven cadavers and one patient. AJNR Am J Neuroradiol. 1986;7(6):1050-1052. [15] MAYER HM, BROCK M, BERLIEN HP, et al. Percutaneous endoscopic laser discectomy (PELD). A new surgical technique for non-sequestrated lumbar discs. Acta Neurochir Suppl (Wien). 1992;54:53-58. [16] LAN T, CHANG L, RAHMATHULLAH MN, et al. Comparative efficacy of interventional therapies for early-stage hepatocellular carcinoma: a prisma-compliant systematic review and network meta-analysis. Medicine. 2016;95:e3185. [17] HIGGINS J, GREEN S. Cochrane handbook for systematic reviews of interventions version 5.1.0[updated march 2011]. Cochrane Coll. 2011. [18] CHAIMANI A, HIGGINS JP, MAVRIDIS D, et al. Graphical tools for network meta-analysis in STATA. PloS One. 2013;8:e76654. [19] JANSEN JP, CRAWFORD B, BERGMAN G, et al. Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health. 2008;11:956-964. [20] SALANTI G, ADES AE, IOANNIDIS JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163-171. [21] ABRISHAMKAR S, KOUCHAKZADEH M, MIRHOSSEINI A, et al. Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J Res Med Sci. 2015;20: 1133-1137. [22] ARTS MP, BRAND R, VAN DEN AKKER ME, et al. Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA . 2009;302:149-158. [23] ARTS MP, BRAND R, VAN DEN AKKER ME, et al. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery. 2011;69:135-144; discussion 144. [24] BROUWER PA, BRAND R, VAN DEN AKKER-VAN MARLE ME, et al. Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: Two-year results of a randomised controlled trial. Int Neuroradiol. 2017;23:313-324. [25] BURTON AK, TILLOTSON KM, CLEARY J. Single-blind randomised controlled trial of chemonucleolysis and manipulation in the treatment of symptomatic lumbar disc herniation. Eur Spine J. 2000;9:202-207. [26] CHATTERJEE S, FOY PM, FINDLAY GF. Report of a controlled clinical trial comparing automated percutaneous lumbar discectomy and microdiscectomy in the treatment of contained lumbar disc herniation. Spine. 1995;20:734-738. [27] CRAWSHAW C, FRAZER AM, MERRIAM WF, et al. A comparison of surgery and chemonucleolysis in the treatment of sciatica. A prospective randomized trial. Spine. 1984;9:195-198. [28] EJESKAR A, NACHEMSON A, HERBERTS P, et al. Surgery versus chemonucleolysis for herniated lumbar discs. A prospective study with random assignment. Clin Orthop Relat Res. 1983;(174):236-242. [29] FRANKE J, GREINER-PERTH R, BOEHM H, et al. Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J. 2009;18: 992-1000. [30] GARG B, NAGRAJA UB, JAYASWAL A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong). 2011;19:30-34. [31] HAINES SJ, JORDAN N, BOEN JR, et al. Discectomy strategies for lumbar disc herniation: results of the LAPDOG trial. J Clin Neurosci.2002;9:411-417. [32] HERMANTIN FU, PETERS T, QUARTARARO L, et al. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958-965. [33] HUANG TJ, HSU RW, LI YY, et al. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res. 2005;23:406-411. [34] HUSSEIN M, ABDELDAYEM A, MATTAR MM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J. 2014;23:1992-1999. [35] KRUGLUGER J, KNAHR K. Chemonucleolysis and automated percutaneous discectomy-a prospective randomized comparison. Int Orthop. 2000;24:167-169. [36] LAVIGNOLLE B, VITAL JM, BAULNY D, et al. [Comparative study of surgery and chemonucleolysis in the treatment of sciatica caused by a herniated disk]. Acta orthopaedica Belgica. 1987;53:244-249. [37] LEE SH, CHUNG SE, AHN Y, et al. Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy: a matched cohort analysis. Mount Sinai J Med. 2006;73:795-801. [38] MAYER HM, BROCK M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216-225. [39] MURALIKUTTAN KP, HAMILTON A, KERNOHAN WG, et al A prospective randomized trial of chemonucleolysis and conventional disc surgery in single level lumbar disc herniation. Spine. 1992;17:381-387. [40] PAN L, ZHANG P, YIN Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg (London, England). 2014;12:534-537. [41] PAN Z, HA Y, YI S, et al. Efficacy of transforaminal endoscopic spine system (tessys) technique in treating lumbar disc herniation. Med Science Monit. 2016;22:530-539. [42] REVEL M, PAYAN C, VALLEE C, et al. Automated percutaneous lumbar discectomy versus chemonucleolysis in the treatment of sciatica. A randomized multicenter trial. Spine.1993;18:1-7. [43] RIGHESSO O, FALAVIGNA A, AVANZI O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery. 2007;61:545-549; discussion 549. [44] RUETTEN S, KOMP M, MERK H, et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine. 2008;33: 931-939. [45] RYANG YM, OERTEL MF, MAYFRANK L, et al. Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery. 2008;62:174-181; discussion 81-82. [46] STULA D. [Chemonucleolysis with chymopapain in lumbar disk hernia. Randomized comparative study with operated patients]. Neurochirurgia. 1990;33:169-172. [47] TELI M, LOVI A, BRAYDA-BRUNO M, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443-450. [48] TULLBERG T, ISACSON J, WEIDENHIELM L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. Spine. 1993;18:24-27. [49] VAN ALPHEN HA, BRAAKMAN R, BEZEMER PD, et al. Chemonucleolysis versus discectomy: a randomized multicenter trial. J Neurosurg. 1989;70: 869-875. [50] WARDLAW D, RITHCHIE IK, SABBOUBEH AF, et al. Prospective randomized trial of chemonucleolysis compared with surgery for soft disc herniation with 1-year, intermediate, and long-term outcome: part II: the radiological outcome. Spine. 2013;38:E1058-1064. [51] WARDLAW D, RITHCHIE IK, SABBOUBEH AF, et al. Prospective randomized trial of chemonucleolysis compared with surgery for soft disc herniation with 1-year, intermediate, and long-term outcome: part I: the clinical outcome. Spine. 2013;38:E1051-1057. [52] RASOULI MR, RAHIMI-MOVAGHAR V, SHOKRANEH F, et al. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 2014;(9):CD010328. [53] HE J, XIAO S, WU Z, et al. Microendoscopic discectomy versus open discectomy for lumbar disc herniation: a meta-analysis. Eur Spine J. 2016; 25:1373-1381. |
| [1] | Lü Zhen, Bai Jinzhu. A prospective study on the application of staged lumbar motion chain rehabilitation based on McKenzie’s technique after lumbar percutaneous transforaminal endoscopic discectomy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1398-1403. |
| [2] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [3] | Gao Yan, Zhao Licong, Zhao Hongzeng, Zhu Yuanyuan, Li Jie, Sang Deen. Alteration of low frequency fluctuation amplitude at brain-resting state in patients with chronic discogenic low back pain [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1160-1165. |
| [4] | Xie Zhifeng, Liu Qing, Liu Bing, Zhang Tao, Li Kun, Zhang Chunqiu, Sun Yanfang. Biomechanical characteristics of the lumbar disc after fatigue injury [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 339-343. |
| [5] | Xiang Feifan, Ye Junwu, Zhang Xihai, Ge Jianhua, Tang Lian, Yang Yunkang. Comparison of three different internal fixation methods in treatment of ipsilateral femoral neck and shaft fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 403-408. |
| [6] | Liu Jinyu, Ding Yiwei, Lu Zhengcao, Gao Tianjun, Cui Hongpeng, Li Wen, Du Wei, Ding Yu. Finite element biomechanical study of full endoscopic fenestration decompression for cervical spondylotic myelopathy [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(24): 3850-3854. |
| [7] | Xu Weilong, Zuo Yuan, Xin Daqi, He Chenyang, Zhao Peng, Shi Ming, Zhou Boyuan, Liu Yating, Zhao Yan. Selection of modeling methods for acute compressive spinal cord injury: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(23): 3767-3772. |
| [8] | Li Yuefei, Li Rui, Ren Jiabin, Liu Xin, Sun Ning, Liu Weike, Bi Jingwei, Sun Zhaozhong. Three-dimensional CT analysis of the treatment of thoracic disc herniation by percutaneous endoscopic posterolateral approach: establishment of a good osseous channel [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3354-3359. |
| [9] | Fu Panfeng, Shang Wei, Kang Zhe, Deng Yu, Zhu Shaobo. Efficacy of anterolateral minimally invasive approach versus traditional posterolateral approach in total hip arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3409-3415. |
| [10] | Ren Xingyu, Zhang Yi, Xu Haoran, Fan Bin, Dai Shifeng, Liang Chunyu. Meta-analysis of the postoperative effects of robot-assisted unicompartmental knee arthroplasty versus conventional surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3416-3422. |
| [11] | Zhong Yuanming, He Bingkun, Wu Zhuotan, Wu Sixian, Wan Tong, Zhong Xifeng. An exploration on the mechanism of Shaoyao Gancao Decoction in treating early pain of lumbar disc herniation based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(20): 3194-3201. |
| [12] | Song Kaikai, Du Gangqiang, Li Peng, Jiang Shengyuan, Gong Zhihao, Zhang Zhiwei, Zhang Kai . Application of head-neck ratio in the treatment of femoral neck fracture in aged patients with artificial femoral head replacement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2805-2809. |
| [13] | Li Haifeng, Liu Yu, Yin Qudong, Sun Zhenzhong, Rui Yongjun, Gu Sanjun. Risk of complications of early postoperative weight-bearing after internal fixation of intracapsular femoral neck fractures: 2-year follow-up [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2875-2880. |
| [14] | Yuan Jiaqin, Luan Fujun, Chen Yangfan, Deng Yi, Li Bo. Meta-analysis of bipolar and unipolar hemiarthroplasties for displaced femoral neck fracture in the elderly patients [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2915-2922. |
| [15] | Hou Yulong, Wang Jingshi, Wang Xukai. Potential mechanism of Achyranthes bidentata in the treatment of lumbar disc herniation based on network pharmacology [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(17): 2734-2739. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||