Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (28): 4584-4592.doi: 10.3969/j.issn.2095-4344.1268
postoperative blood loss of intertrochanteric fracture: a meta-analysis
Zhong Yanchun, Liu Lulin, Xiao Jianhua, Ouyang Xunyan, Huang Weimin, Liu Wuyang
- Department of Orthopedics, the First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China
-
Online:2019-10-08Published:2019-10-08 -
Contact:Liu Wuyang, Master, Professor, Chief physician, Department of Orthopedics, the First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China -
About author:Zhong Yanchun, Master, Attending physician, Department of Orthopedics, the First Affiliated Hospital of Gannan Medical University, Ganzhou 341000, Jiangxi Province, China -
Supported by:the Project of Science and Technology Department of Jiangxi Province, No. 2012BBG70108 (to LWY)| the Youth Program of Education Department of Jiangxi Province, No. GJJ170883 (to ZYC)| the Science and Technology Program of Education Department of Jiangxi Province, No. GJJ14678 (to LWY)
CLC Number:
Cite this article
Zhong Yanchun, Liu Lulin, Xiao Jianhua, Ouyang Xunyan, Huang Weimin, Liu Wuyang. postoperative blood loss of intertrochanteric fracture: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(28): 4584-4592.
share this article
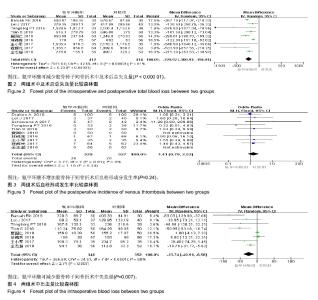
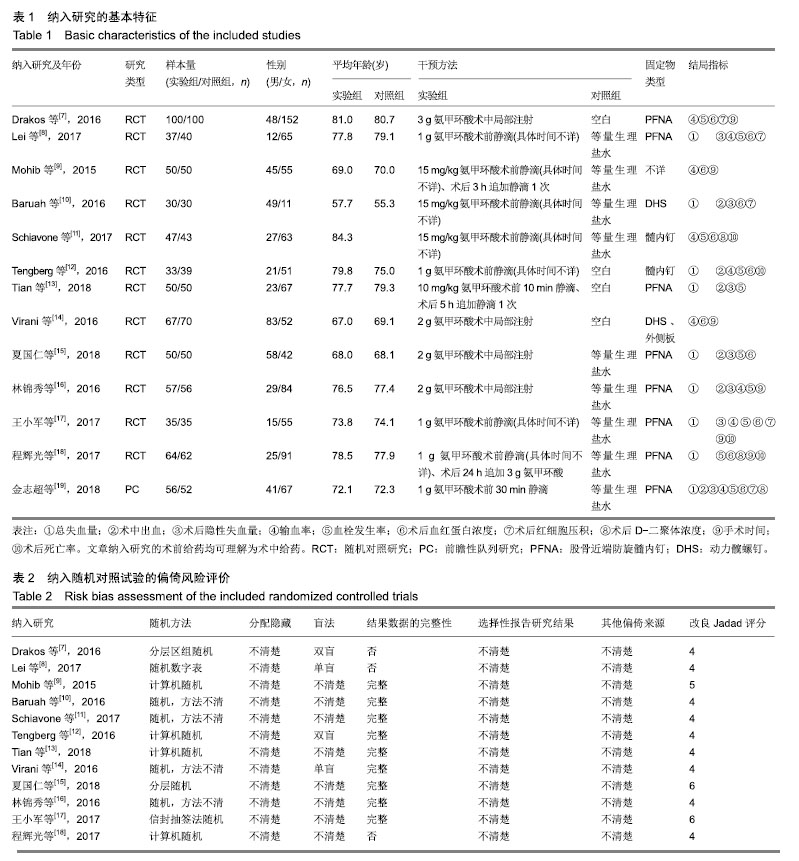
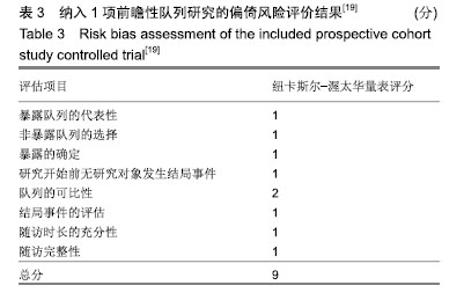
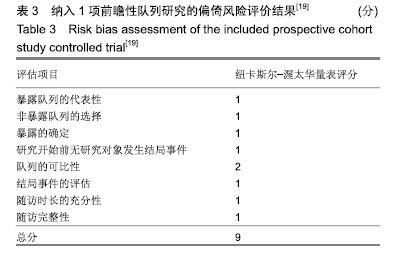
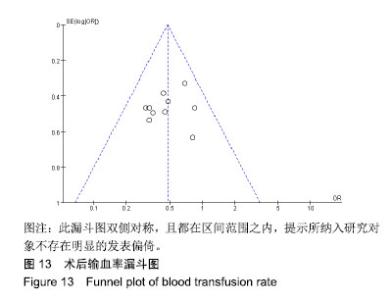
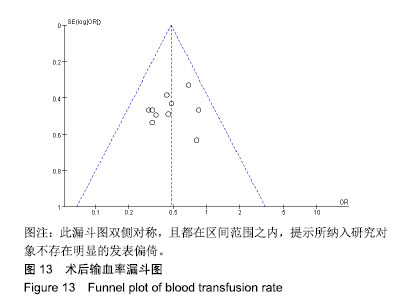
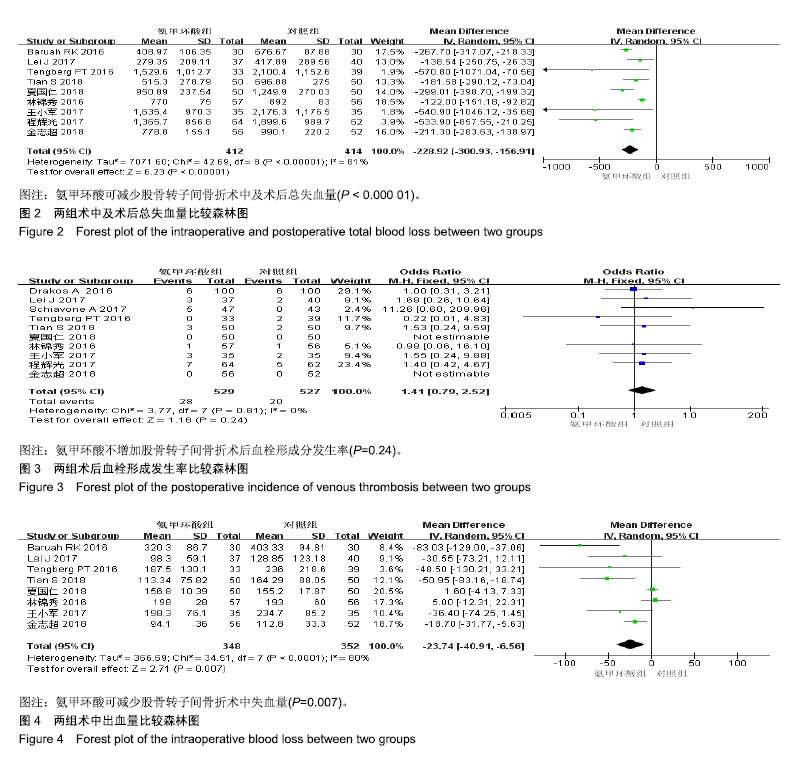
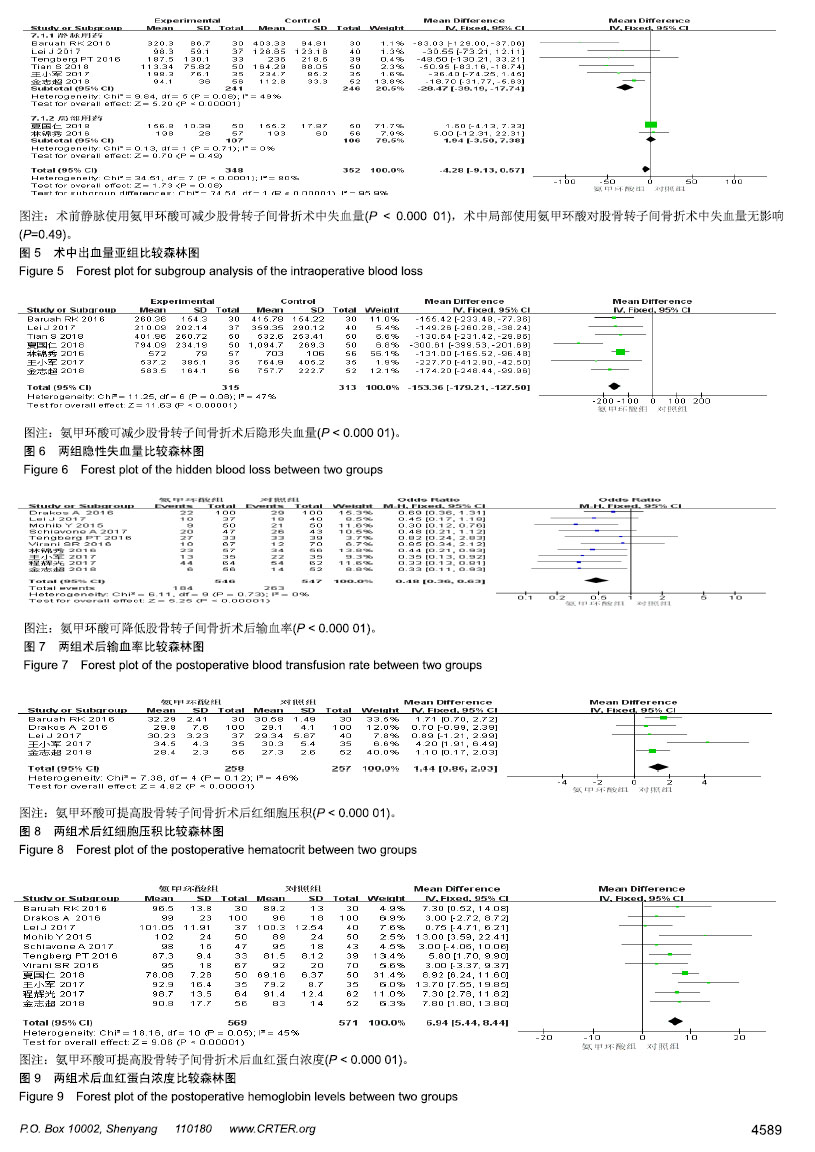
2.3 Meta分析结果 2.3.1 术中及术后总失血量 共纳入9个研究[8,10. 12-13,15-19],包含氨甲环酸组患者412例,对照组414例。异质性检验结果显示,存在明显异质性(P < 0.000 01,I2=81%),故采用随机效应模型进行合并。结果显示,氨甲环酸组总失血量少于对照组(MD=-228.92,95%CI:-300.93至-156.91,P < 0.000 01),见图2。考虑到异质性明显,进行文献逐一剔除进行敏感性分析,结果显示剔除林锦秀2016年的研究文献时,异质性检验结果为(P < 0.06,I2=47%),Meta分析结果为(MD=-243.86,95%CI:-302.12至-185.6,P < 0.000 01)。重新检查该研究的对象、干预措施、对照措施和研究结果等,未发现其他临床异质性。考虑到剔除该文献前后,Meta分析结果比较稳定,因此采用不剔除随机效应模型检验结果。 2.3.2 血栓形成发生率 共纳入10个研究[7-8,11-13,15-19],包含氨甲环酸组患者529例,发生血栓形成28例;对照组527例,发生血栓形成20例。异质性检验结果显示,无异质性(P=0.81,I2=0%),故采用固定效应模型进行合并。结果显示,两组术后血栓形成无差异(OR=1.41,95%CI:0.79-2.52,P=0.24),见图3。 2.3.3 术中出血量 有8个研究报道了术中出血量指 标[8、10、12、13、15-17、19],氨甲环酸组患者348例,对照组352例。异质性检验结果显示,存在明显异质性(P < 0.000 1,I2=80%),故采用随机效应模型进行合并。结果显示,氨甲环酸组术中出血量少于对照组(MD=-23.74,95%CI:-40.91至-6.56,P=0.007) ,见图4。 考虑异质性较大,根据氨甲环酸给药途径不同进行亚组分析,结果显示,各小组异质性明显缩小,术前静脉给药组减少术中出血量疗效更佳(MD=-28.47,95%CI:-39.19至-17.74,P < 0.000 01),术中局部给药组出血与对照组无显著差异(MD=1.94,95%CI:-3.50-7.38,P=0.49),见图5。 2.3.4 隐性失血量 共纳入7个研究[8,10,13,15-17,19],包含氨甲环酸组患者315例,对照组313例。异质性检验结果显示,研究不存在明显异质性(P=0.08,I2=47%),故采用固定效应模型进行合并。结果显示,氨甲环酸组术后隐性失血量少于对照组(MD=-153.36,95%CI:-179.21至-127.50,P < 0.000 01),见图6。 2.3.5 输血率 共纳入10个研究[7-8,11-13,15-19],包含氨甲环酸组患者546例,对照组547例。异质性检验结果显示,无异质性(P=0.73,I2=0%),故采用固定效应模型进行合并。结果显示,氨甲环酸组的输血率少于对照组(OR=0.48,95%CI:0.36-0.63,P < 0.000 01),见图7。"

2.3.6 术后红细胞压积 共纳入5个研究[7-8,10,17,19],包含氨甲环酸组患者258例,对照组257例。异质性检验结果显示无异质性(P=0.12,I2=46%),故采用固定效应模型进行合并。结果显示,氨甲环酸组术后红细胞压积高于对照组(MD=1.44,95% CI:0.86-2.03,P < 0.000 01),见图8。 2.3.7 术后血红蛋白浓度 纳入11个研究[7-12,14-15, 17-19],包含氨甲环酸组患者569例,对照组571例。异质性检验结果显示无异质性(P=0.05,I2=45%),故采用固定效应模型进行合并。结果显示,氨甲环酸组术后血红蛋白浓度高于对照组(MD=6.94,95% CI:5.44-8.44,P < 0.000 01),见图9。"
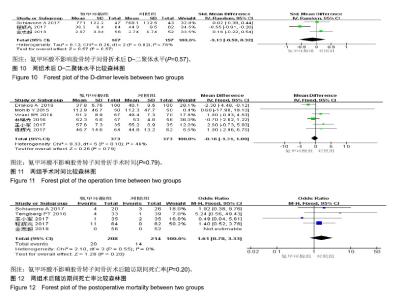
2.3.8 术后D-二聚体浓度 共纳入3个研究[11,18-19],包含氨甲环酸组患者167例,对照组157例。因不同研究数值差别大,采用标准化均数差评估。异质性检验结果显示,异质性明显(P=0.02,I2=76%),因纳入研究较少,通过逐一剔除方法,进行敏感性分析结果显示,剔除程辉光等[18]研究文献时,异质性检验结果为P=0.62,I2=0%,Meta分析结果为(SMD=-0.1,95%CI:-0.18-0.38,P=0.49)。重新检查该研究的对象、干预措施、对照措施和研究结果等,未能找出异质性来源,故未剔除,故采用随机效应模型进行合并。结果显示,氨甲环酸组和对照组D二聚体浓度无显著差异(SMD=-0.13,95%CI:-0.58-0.32,P=0.57),见图10。 2.3.9 手术时间 共纳入6个研究[7,9,14,16-18],包含氨甲环酸组患者373例,对照组373例。异质性检验结果显示,无明显异质性(P=0.1,I2=46%),故采用固定效应模型进行合并。结果显示,两组手术时间无差显著异(MD=-0.16,95%CI:-1.31-1.00,P=0.79),见图11。 2.3.10 随访期间死亡率 有5个研究报道了术后死亡例数指标[11-12,17-19],包含氨甲环酸组患者208例,死亡20例;对照组214例,死亡14例。异质性检验结果显示,无异质性(P=0.55,I2=0%),故采用固定效应模型进行合并。结果显示,两组术后死亡率无显著差异(OR=1.61,95%CI:0.78-3.33,P=0.2),见图12。"
| [1]Du Y, Feng C. The efficacy of tranexamic acid on blood loss from lumbar spinal fusion surgery: a meta-analysis of randomized controlled trials. World Neurosurg. 2018;119: e228-e234. [2]Wang F, Zhao KC, Zhao MM, et al. The efficacy of oral versus intravenous tranexamic acid in reducing blood loss after primary total knee and hip arthroplasty: a meta-analysis. Medicine (Baltimore). 2018;97(36):e12270.[3]Sun H, Deng J, Ning X, et al. Letter to the Editor Regarding "The Efficacy of Tranexamic Acid on Blood Loss of Lumbar Spinal Fusion Surgery: A Meta-Analysis of Randomized Controlled Trials". World Neurosurg. 2019;122:708.[4]王谦,黄国鑫,陈磊,等.髓芯减压联合自体骨髓间充质干细胞移植治疗股骨头坏死:安全和有效性的Meta分析[J].中国组织工程研究,2018,22(17):2733-2739.[5]Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials.1996;17:1-12. [6]Zeng X, Zhang Y, Kwong JS, et al. The ethodological quality assessment tools for preclinical and clinical studies,systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2-10. [7]Drakos A, Raoulis V, Karatzios K, et al. Efficacy of Local Administration of Tranexamic Acid for Blood Salvage in Patients Undergoing Intertrochanteric Fracture Surgery. J Orthop Trauma. 2016;30(8):409-414.[8]Lei J, Zhang B, Cong Y, et al. Tranexamic acid reduces hidden blood loss in the treatment of intertrochanteric fractures with PFNA: a single-center randomized controlled trial. J Orthop Surg Res. 2017;12(1):124. [9]Mohib Y, Rashid RH, Ali M, et al. Does tranexamic acid reduce blood transfusion following surgery for inter-trochanteric fracture? A randomized control trial. J Pak Med Assoc. 2015; 65(11 Suppl 3):S17-20.[10]Baruah RK, Borah PJ, Haque R. Use of tranexamic acid in dynamic hip screw plate fixation for trochanteric fractures. J Orthop Surg (Hong Kong). 2016;24(3):379-382. [11]Schiavone A, Bisaccia M, Inkov I, et al. Tranexamic Acid in Pertrochanteric Femoral Fracture: Is it a Safe Drug or Not? Folia Med (Plovdiv). 2018;60(1):67-78. [12]Tengberg PT, Foss NB, Palm H, et al. Tranexamic acid reduces blood loss in patients with extracapsular fractures of the hip: results of a randomised controlled trial. Bone Joint J. 2016; 98-B(6): 747-753.[13]Tian S, Shen Z, Liu Y, et al. The effect of tranexamic acid on hidden bleeding in older intertrochanteric fracture patients treated with PFNA. Injury. 2018;49(3):680-684.[14]Virani SR, Dahapute AA, Panda I, et al. Role of local infiltration of tranexamic acid in reducing blood loss in peritrochanteric fracture surgery in the elderly population. Malays Orthop J. 2016;10(3): 26-30. [15]夏国仁,李业海,刘庆.氨甲环酸腔内注射对股骨粗隆间骨折闭合髓内钉内固定潜在失血量的影响[J].安徽医药,2018,22(6): 1148-1151. [16]林锦秀,孙东升,郑潇,等.局部应用氨甲环酸干预股骨粗隆间骨折 PFNA内固定术后隐性失血的临床分析[J].山东大学学报(医学版), 2016,54(1):67-70.[17]王小军,陈永华,程昊,等.氨甲环酸应用于股骨转子间骨折的有效性和安全性分析[J].浙江医学,2017,39(16):1373-1375. [18]程辉光,段宁,马涛,等.老年不稳定性股骨转子间骨折使用氨甲环酸的有效性和安全性[J].实用骨科杂志,2017,23(12):1138-1140.[19]金志超,郑晓辉,余翔, 等.氨甲环酸降低转子间骨折围术期失血的有效性及安全性[J].中国组织工程研究,2018,22(15):2361-2366.[20]Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporos Int. 2013;24(10):2725-2728. [21]Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br. 2006;88:1053-1059. [22]Yang X, Wu Q, Wang X. Investigation of perioperative hidden blood loss of unstable intertrochanteric fracture in the elderly treated with different intramedullary fixations. Injury. 2017;48(8): 1848-1852. [23]Hunt BJ. The current place of tranexamic acid in the management of bleeding. Anaesthesia. 2015;70 Suppl 1:50-53. [24]El-Menyar A, Sathian B, Asim M, et al. Efficacy of prehospital administration of tranexamic acid in trauma patients: a meta-analysis of the randomized controlled trials. Am J Emerg Med. 2018;36(6):1079-1087. [25]Wang W, Yu J. Tranexamic acid reduces blood loss in intertrochanteric fractures: a meta-analysis from randomized controlled trials. Medicine (Baltimore). 2017;96(52):e9396.[26]Zhu Q, Yu C, Chen X, et al. Efficacy and safety of tranexamic acid for blood salvage in intertrochanteric fracture surgery: a meta-analysis. Clin Appl Thromb Hemost. 2018;24(8):1189-1198.[27]Yerneni K, Burke JF, Tuchman A, et al. Topical tranexamic acid in spinal surgery: A systematic review and meta-analysis. J Clin Neurosci. 2018. doi: 10.1016/j.jocn.2018.10.121.[28]侯靖钊,包洪卫,徐鹏程,等.股骨转子间骨折术中局部和静脉应用氨甲环酸的疗效比较[J].临床骨科杂志,2017,20(6):733-735.[29]Fillingham YA, Ramkumar DB, Jevsevar DS, et al. The efficacy of tranexamic acid in total hip arthroplasty: a network meta-analysis. J Arthroplasty. 2018;33(10):3083-3089. [30]Lu VM, Ho YT, Nambiar M, et al. The perioperative efficacy and safety of antifibrinolytics in adult spinal fusion surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976). 2018;43(16):E949-E958. [31]陆芸,马宝通,郭若霖,等.骨科创伤患者深静脉血栓危险因素的研究[J].中华骨科杂志,2007,27(9):693-698.[32]Weitz JI, Fredenburgh JC, Eikelboom JW. A test in context: d-dimer. J Am Coll Cardiol. 2017;70(19):2411-2420. [33]Olson JD. D-dimer: an overview of hemostasis and fibrinolysis, assays, and clinical applications. Adv Clin Chem. 2015;69:1-46. [34]Pong RP, Leveque JA, Edwards A, et al. Effect of tranexamic acid on blood loss, d-dimer, and fibrinogen kinetics in adult spinal deformity surgery. J Bone Joint Surg Am. 2018;100(9): 758-764. [35]Lewis PM, Waddell JP. When is the ideal time to operate on a patient with a fracture of the hip? A review of the available literature. Bone Joint J. 2016;98-B (12):1573-1581. [36]高化,王宝军,赵亮,等.股骨转子间骨折围术期的并发症及死亡原因分析[J].中华骨科杂志,2015,35(8):819-824.[37]Parker MJ, Handoll HH. Conservative versus operative treatment for extracapsular hip fractures. Cochrane Database Syst Rev. 2000;(2):CD000337. [38]袁志,毕龙.老年股骨转子间骨折的治疗趋势[J].中华骨科志, 2017, 37(17):1057-1060. |
| [1] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [2] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [3] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [4] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [5] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [6] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [7] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [8] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [9] | Cai Qunbin, Zou Xia, Hu Jiantao, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei. Relationship between tip-apex distance and stability of intertrochanteric femoral fractures with proximal femoral anti-rotation nail: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 831-836. |
| [10] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [11] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [12] | Li Yan, Wang Pei, Deng Donghuan, Yan Wei, Li Lei, Jiang Hongjiang. Electroacupuncture for pain control after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 957-963. |
| [13] | He Xiangzhong, Chen Haiyun, Liu Jun, Lü Yang, Pan Jianke, Yang Wenbin, He Jingwen, Huang Junhan. Platelet-rich plasma combined with microfracture versus microfracture in the treatment of knee cartilage lesions: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 964-969. |
| [14] | Hua Haotian, Zhao Wenyu, Zhang Lei, Bai Wenbo, Wang Xinwei. Meta-analysis of clinical efficacy and safety of antibiotic artificial bone in the treatment of chronic osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 970-976. |
| [15] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||