| [1] Rozen N,Bick T,Bajayo A,et al.Transplanted blood-derived endothelial progenitor cells (EPC) enhance bridging of sheep tibia critical size defects.Bone.2009;45(5):918-924.
[2] 卢向东,郭庆华,刘强,等.转基因干细胞构建组织工程骨的初步实验研究[J].中华显微外科杂志,2010,33(2):143-145.
[3] 闫峰,杨卫良,杨威.生物材料修复股骨缺损及其性能评价[J].中国组织工程研究与临床康复,2010,14(16):2963-2966.
[4] 贾祎佳,刘强,卢向东,等.转碱性成纤维细胞生长因子基因组织工程骨修复兔骨缺损[J].中国组织工程研究与临床康复,2011, 15(8): 1365-1368.
[5] 中华人民共和国科学技术部.关于善待实验动物的指导性意见. 2006-09-30.
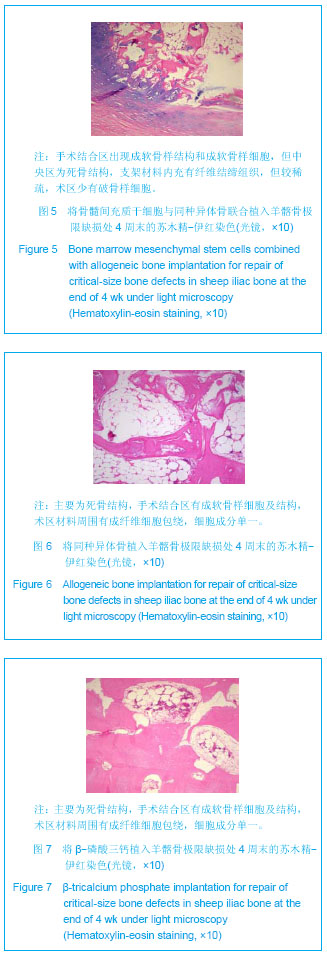
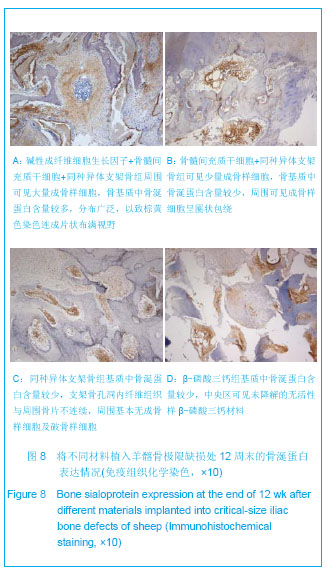
[6] 杨楠,何惠宇,胡杨,等.复合骨髓间充质干细胞同种异体支架骨修复羊髂骨极限缺损[J].中国组织工程研究,2013,17(16): 2859-2868.
[7] 胡杨,马莹,何惠宇.兔下颌骨前牙区剩余牙槽嵴模型的建立[J].中国组织工程研究与临床康复,2011,15(20):3653-3656.
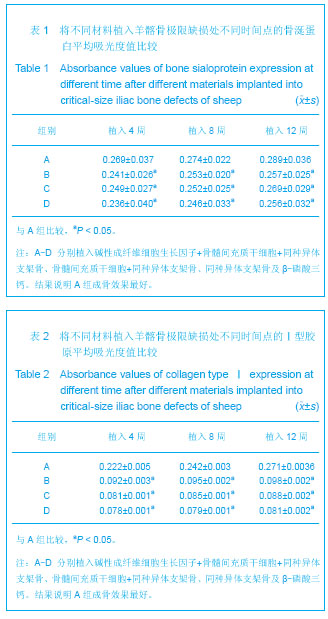
[8] 袁林,曹凯华,童心.骨涎蛋白在不同类型种植体骨界面改建中的变化[J].牙体牙髓牙周病学杂志,2012,22(6):319-322.
[9] 许慧芬,何惠宇,唐小雪.物理联合化学或化学方法处理去抗原异种松质骨支架与骨髓间充质干细胞的细胞相容性[J].中国组织工程研究,2012,16(6):958-962.
[10] Francisco JS,Moraes HP,Dias EP.Evaluation of the Image-Pro Plus 4.5 software for automatic counting of labeled nuclei by PCNA immunohistochemistry.Braz Oral Res.2004;18(2): 100-104.
[11] 徐洪,杨方,袁媛,等.免疫组织化学Image Pro Plus图像半定量分析的参数选择[J].解剖学杂志,2012,35(1):37-41.
[12] Schmitz JP,Hollinger JO.The critical size defect as an experimental model for craniomandibulofacial nonunions.Clin Orthop Relat Res.1986;(205):299-308.
[13] 陈欣,张春林.组织工程骨修复骨缺损的研究进展及临床应用[J].中国组织工程研究与临床康复,2010,14(24):4486-4490.
[14] Su X,Bao G,Kang H.Effects of basic fibroblast growth factor on bone marrow mesenchymal stem cell differentiation into temporomandibular joint disc cells.J Biomed Eng.2012; 9(4): 732-736.
[15] 王磊,章燕,游素兰,等.骨形态发生蛋白-2与碱性成纤维细胞生长因子在异位和原位成骨中的作用[J].华西口腔医学杂志,2012, 30(4):420-424.
[16] 朱国华,蔡建平,郭翠玲,等.骨形态发生蛋白与碱性成纤维细胞生长因子联合修复软骨缺损的效果评价[J].中国组织工程研究, 2012,16(11):1910-1914.
[17] 李春明,王鑫,刘宝林,等.种植体+ bFGF基因修饰骨髓基质细胞复合Bio-Oss胶原修复犬颌骨缺损的实验研究[J].实用口腔医学杂志,2009,25(1):26-30.
[18] 杨海兵,韩萱,杨琳,等.血管内皮生长因子和转化生长因子β1基因调控人根尖乳头细胞矿化相关因子的研究[J].华西口腔医学杂志,2012,30(5):468-473.
[19] 李景辉,刘大勇,张方明,等.应用人恒牙牙髓干细胞与明胶支架构建组织工程骨的研究[J].北京口腔医学,2013,21(1):21-26.
[20] Song SJ,Jeon O,Yang HS,et al.Effects of culture conditions on steogenic differentiation in human esenchymal stem cells.J icrobiol Biotechnol.2007;17 (7):1113-1119.
[21] 夏欣一,崔英霞,杨滨,等.Ⅰ型胶原基因突变与成骨不全研究进展[J].中国优生与遗传杂志,2009,17(5):12-13.
[22] 郑瑜谦,袁芳,闫福华,等.冻存骨髓基质细胞复合材料体内成骨基质的合成能力[J].中国组织工程研究与临床康复,2011,15(12): 2275-2287.
|

.jpg)
.jpg)
.jpg)
.jpg)