Chinese Journal of Tissue Engineering Research ›› 2014, Vol. 18 ›› Issue (1): 7-13.doi: 10.3969/j.issn.2095-4344.2014.01.002
Previous Articles Next Articles
Proliferation ability of bone marrow mesenchymal stem cells in corticosteroid-induced osteonecrosis of femoral head
Wang Bai-liang, Li Tie-jun, Yue De-bo, Sun Wei
- Department of Joint Surgery, China-Japan Friendship Hospital, Beijing 100029, China
-
Revised:2013-10-24Online:2014-01-01Published:2014-01-01 -
Contact:Wang Bai-liang, M.D., Associate chief physician, Department of Joint Surgery, China-Japan Friendship Hospital, Beijing 100029, China -
About author:Wang Bai-liang, M.D., Associate chief physician, Department of Joint Surgery, China-Japan Friendship Hospital, Beijing 100029, China
CLC Number:
Cite this article
Wang Bai-liang, Li Tie-jun, Yue De-bo, Sun Wei. Proliferation ability of bone marrow mesenchymal stem cells in corticosteroid-induced osteonecrosis of femoral head[J]. Chinese Journal of Tissue Engineering Research, 2014, 18(1): 7-13.
share this article
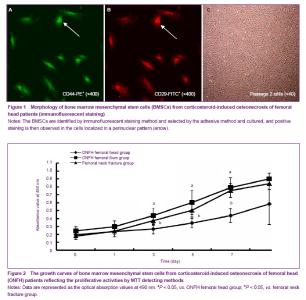
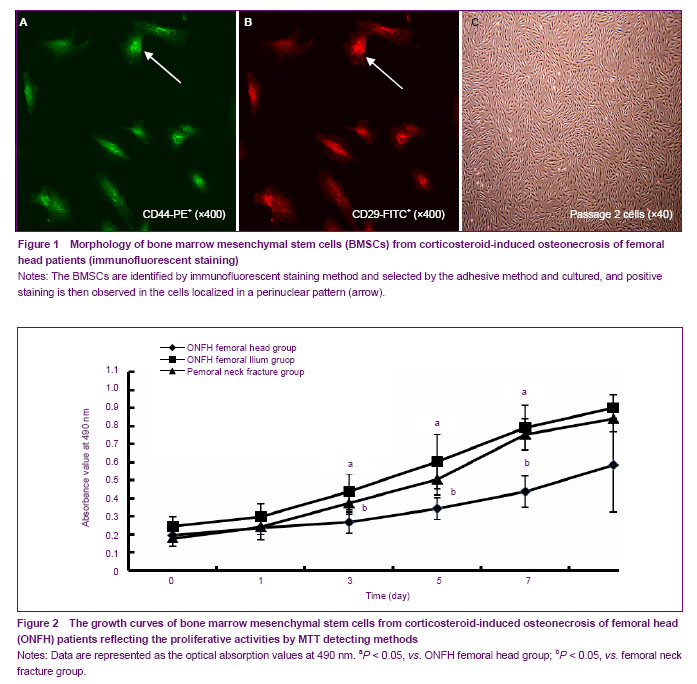
Identification of BMSCs from corticosteroid-induced ONFH patients There was marked difference in growth state of BMSCs between corticosteroid-induced ONFH femoral head group and the other two groups under an inverted microscope 24 hours after primary culture, and BMSCs from all groups adhered and extended in spindle or polygonal shape. Forty-eight hours later, the clone formed and adherent cells increased. However, the number of clones in the corticosteroid-induced ONFH femoral head group was much less than that in the other two groups. BMSCs resembled typical features of fibroblasts 3 days later in the other two groups and 5 days later in the corticosteroid-induced ONFH femoral head group. Clones enlarged and fused into monolayer 7 days later in the femoral neck fracture group and the corticosteroid-induced ONFH ilium group and 10 days later in corticosteroid-induced ONFH femoral head group. In the femoral neck fracture group and the corticosteroid-induced ONFH ilium group, BMSCs proliferated and distributed evenly after passage and adhered partially 2 hours later and completely in funicular shape 24 hours later. In contrast, BMSCs from corticosteroid-induced ONFH femoral head group proliferated very slowly and overgrew the bottle till 10-12 days later. The immunofluorescent staining showed that the cultured cells expressed typical BMSCs markers such as CD29 and CD44, but not typical haematopoietic cell markers including CD34, CD14 and CD133 (Figures 1 A-C). Proliferative activity of BMSCs from corticosteroid- induced ONFH patients The proliferative activities of BMSCs using MTT methods were obtained from the three groups and drawn into the growth curves. As shown in the figures, the proliferative activity of BMSCs in the femoral neck fracture group and the corticosteroid-induced ONFH ilium group were remarkably stronger than that in the corticosteroid-induced ONFH femoral head group. For the corticosteroid-induced ONFH femoral head group, BMSCs growth fell into the stagnant stage within 1-7 days after seeding, turned into the logarithmic stage at 8 days, and came to the plateau stage thereafter. However, the growth curve in the femoral neck fracture group and the corticosteroid-induced ONFH ilium group moved left obviously and the peak increased (Figure 2)."
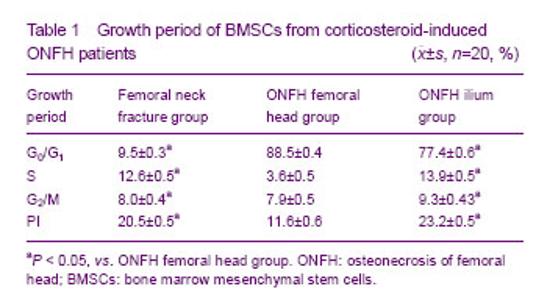
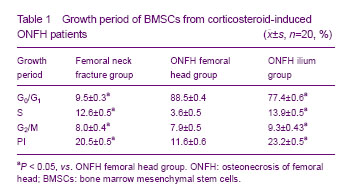
Growth period of BMSCs from corticosteroid-induced ONFH patients For FCAS, the percentage of cells in S stage or G2/M+S stages was usually taken as PI to indicate the proliferation of cells. Compared with the other two groups, the percentage of cells in G0/G1 stages in the corticosteroid-induced ONFH femoral head group was increased significantly while the percentage in G2/M+S stages (PI) was decreased significantly (P < 0.05). The percentage of cells in G2 stage in the corticosteroid-induced ONFH ilium group was the highest in the three groups. These were in consistent with results revealed by MTT method (Table 1)."
| [1] Jones JP Jr. Fat embolism, intravascular coagulation,and osteonecrosis. Clin Orthop Relat Res. 1993;(292):294-308. [2] Mirzai R, Chang C, Greenspan A, et al. The pathogenesis of osteonecrosis and the relationships to corticosteroids. J Asthma.1999;36(1):77-95. [3] Pittenger MF, Mackay AM, Jaiswal SC, et al. Multilineage potential of adult human mesenchamal stem cells. Science. 1999;284(5411):143-147. [4] Hernigou P, Beaujean F, Lambotte JC. Decrease in the mesenchymal stem cell pool in the proximal femur in corticosteroid-induced osteonecrosis. J Bone Joint Surg (Br). 1999;81(2):349-355. [5] Gangji V, Hauzeur JP, Schoutens A, et al. Abnormalities in the replicative capacity of osteoblastic cells in the proximal femur of patients with osteonecrosis of the femoral head. J Rheumatol. 2003;30(2):348-351. [6] Wang GJ, Cui Q, Balian G. The pathogenesis and prevention of steroid-induced osteonecrosis. Clin Orthop. 2000;(370):295-310. [7] State Council of the People’s Republic of China. Administrative Regulations on Medical Institution. 1994-09-01.[8] Suh KT, Kim SW, Roh HL, et al. Decreased osteogenic differentiation of mesenchymal stem cells in alcohol-induced osteonecrosis. Clin Orthop Relat Res. 2005;(431):220-225. [9] Beyer Nardi N, da Silva Meirelles L. Mesenchymal stem cells: isolation, in vitro expansion and characterization. Handb Exp Pharmacol. 2006;(174):249-282. [10] Drescher W, Weigert KP, Bunger MH, et al. Fermoral head blood flow reduction and hypercoagulablitity under 24 h megadose steroid treatment in pigs. J Orthop Res. 2004; 22(3):501-508. [11] Asano T, Takahashi KA, Fujioka M, et al. Genetic analysis of steroid-induced osteonecrosis of the femoral head. J Orthop Sci. 2003;8(3):329-333. [12] Tektonidou MG, Moutsopoulos HM. Immunologic factor in the pathogenesis of osteonecrosis. Orthop Clin North Am. 2004;35(3):259-263. [13] Wu Z, Ji C, Li H, et al. Elevated level of membrane microparticles in the disease of steroid-inducedvascular osteonecrosis. J Craniofac Surg. 2013;24(4):1252-1256. [14] Li X, Jin L, Cui Q, et al. Steroid effects on osteogenesis through mesenchymal cell gene expression. Osteoporos Int. 2005;16(1):101-108. [15] Cui Q, Wang GJ, Balian G. Steroid-induced adipogenesis in a pluripotential cell line from bone marrow. J Bone Joint Surg Am. 1997;79(7):1054-1063. [16] Lee JS, Lee JS, Roh HL, et al. Alterations in the differentiation ability of mesenchymal stem cells in patients with nontraumatic osteonecrosis of the femoral head: comparative analysis according to the risk factor. J Orthop Res. 2006;24(4):604-609. [17] Yin L, Li YB, Wang YS. Dexamethasone-induced adipogenesis in primary marrow stromal cell cultures: mechanism of steroid-induced osteonecrosis. Chin Med J (Engl). 2006;119(7):581-588. [18] Castro-Malaspina H, Gay RE, Resnick G, et al. Characterization of human bone marrow fibroblast colony-forming cells (CFU-F) and their progeny. Blood. 1980;56(2):289-301. [19] Egrise D, Martin D, Vienne A, et al. The number of fibroblastic colonies formed from bone marrow is decreased and the in vitro proliferation rate of trabecular bone cells increased in aged rats. Bone. 1992;13(5): 355-361. [20] Fazeli PK, Horowitz MC, MacDougald OA, et al. Marrow fat and bone--new perspectives. J Clin Endocrinol Metab. 2013;8(3):935-945. [21] Penolazzi L, Mazzitelli S, Vecchiatini R, et al. Human mesenchymal stem cells seeded on extracellular matrix-scaffold: viability and osteogenic potential. J Cell Physiol. 2012;27(2):857-866. [22] Muschler GF, Nitto H, Boehm CA, et al. Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res. 2001;19(1):117-125. [23] Glimcher MJ, Kenzora JE. The biology of osteonecrosis of the human femoral head and its clinical implications: III. Discussion of the etiology and genesis of the pathological sequelae: Comments on treatment. Clin Orthop. 1979;(140): 273-312. [24] Helbig L, Simank HG, Kroeber M, et al. Core decompression combined with implantation of a demineralised bone matrix for non-traumatic osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2012;132(8):1095-1103. [25] Youm YS, Lee SY, Lee SH. Apoptosis in the osteonecrosis of the femoral head. Clin Orthop Surg. 2010;2(4):250-255.[26] Wang BL, Sun W, Shi ZC, et al. Decreased proliferation of mesenchymal stem cells in corticosteroid-induced osteonecrosis of femoral head. Orthopedics. 2008;31(5): 444. [27] Hernigou P, Beaujean F. Abnormalities in the bone marrow of the iliac crest in patients who have osteonecrosis secondary to corticosteroid therapy or alcohol abuse. J Bone Joint Surg (Am). 1997;79(7):1047-1053. [28] Gangji V, De Maertelaer V, Hauzeur JP. Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head: five year follow-up of a prospective controlled study. Bone. 2011;9(5):1005-1009. [29] Weinstein RS, Nicholas RW, Manolagas SC. Apoptosis of osteocytes in glucocorticoid-induced osteonecrosis of the hip. J Clin Endocrinol Metab. 2000;85(8):2907-2912. [30] Weinstein RS, Jilka RL, Parfitt AM, et al. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids.Potential mechanisms of their deleterious effects on bone. J Clin Invest. 1998;102(2):274-282. [31] Hofbauer LC, Khosla S, Dunstan CR, et al. The roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorption. J Bone Mner Res. 2000;15: 2-12. [32] Wang BL, Sun W, Shi ZC, et al. Treatment of nontraumatic osteonecrosis of the femoral head with the implantation of core decompression and concentrated autologous bone marrow containing mononuclear cells. Arch Orthop Trauma Surg. 2010;130(7):859-865.[33] Zhao D, Cui D, Wang B, et al. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone. 2012;50(1):325-330. [34] Chotivichit A, Korwutthikulrangsri E, Auewarakul C, et al. Core decompression and concentrated autologous bone marrow injection for treatment of osteonecrosis of the femoral head. J Med Assoc Thai. 2012;95(Suppl 9):S14-S20. [35] Ji WF, Ding WH, Ma ZC, et al. Three-tunnels core decompression with implantation of bone marrow stromal cells (bMSCs) and decalcified bone matrix (DBM) for the treatment of early femoral head necrosis. Zhongguo Gu Shang. 2008;21(10):776-778. [36] Yan ZQ, Chen YS, Li WJ, et al. Treatment of osteonecrosis of the femoral head by percutaneous decompression and autologous bone marrow mononuclear cell infusion. Chin J Traumatol. 2006;9(1):3-7. [37] Liu Y, Liu S, Su X. Core decompression and implantation of bone marrow mononuclear cells with porous hydroxylapatite composite filler for the treatment of osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2013;133(1):125-133. [38] Chang T, Tang K, Tao X, et al. Treatment of early avascular necrosis of femoral head by core decompression combined with autologous bone marrow mesenchymal stem cells transplantation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24(6):739-743. |
| [1] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [2] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [3] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [4] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [5] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [6] | Geng Yao, Yin Zhiliang, Li Xingping, Xiao Dongqin, Hou Weiguang. Role of hsa-miRNA-223-3p in regulating osteogenic differentiation of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1008-1013. |
| [7] | Lun Zhigang, Jin Jing, Wang Tianyan, Li Aimin. Effect of peroxiredoxin 6 on proliferation and differentiation of bone marrow mesenchymal stem cells into neural lineage in vitro [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1014-1018. |
| [8] | Zhu Xuefen, Huang Cheng, Ding Jian, Dai Yongping, Liu Yuanbing, Le Lixiang, Wang Liangliang, Yang Jiandong. Mechanism of bone marrow mesenchymal stem cells differentiation into functional neurons induced by glial cell line derived neurotrophic factor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1019-1025. |
| [9] | Pei Lili, Sun Guicai, Wang Di. Salvianolic acid B inhibits oxidative damage of bone marrow mesenchymal stem cells and promotes differentiation into cardiomyocytes [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1032-1036. |
| [10] | Wang Shiqi, Zhang Jinsheng. Effects of Chinese medicine on proliferation, differentiation and aging of bone marrow mesenchymal stem cells regulating ischemia-hypoxia microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1129-1134. |
| [11] | Cai Qunbin, Zou Xia, Hu Jiantao, Chen Xinmin, Zheng Liqin, Huang Peizhen, Lin Ziling, Jiang Ziwei. Relationship between tip-apex distance and stability of intertrochanteric femoral fractures with proximal femoral anti-rotation nail: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 831-836. |
| [12] | Chen Junyi, Wang Ning, Peng Chengfei, Zhu Lunjing, Duan Jiangtao, Wang Ye, Bei Chaoyong. Decalcified bone matrix and lentivirus-mediated silencing of P75 neurotrophin receptor transfected bone marrow mesenchymal stem cells to construct tissue-engineered bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 510-515. |
| [13] | Liu Jiangfeng. Nano-hydroxyapatite/polyamide 66 composite filling combined with locking plate in the treatment of fibrous dysplasia of femoral bone [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 542-547. |
| [14] | Nie Shaobo, Li Jiantao, Sun Jien, Zhao Zhe, Zhao Yanpeng, Zhang Licheng, Tang Peifu. Mechanical stability of medial support nail in treatment of severe osteoporotic intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 329-333. |
| [15] | Cheng Shigao, , Wang Wanchun, Jiang Dong, Li Tengfei, Li Xun, Ren Lian. Comparison of the standard and long-stem bone cement prosthesis replacement in the treatment of intertrochanteric fractures in elderly patients [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 362-367. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||