Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (16): 4137-4145.doi: 10.12307/2026.688
Previous Articles Next Articles
Association between triglyceride-glucose-body mass index and the risk of hypertension in middle-aged and elderly Chinese population
Zhou Zigui, Liu Jingjing
- School of Exercise and Health, Shanghai University of Sport, Shanghai 200438, China
-
Received:2025-06-06Accepted:2025-09-05Online:2026-06-08Published:2025-11-28 -
Contact:Liu Jingjing, PhD, School of Exercise and Health, Shanghai University of Sport, Shanghai 200438, China -
About author:Zhou Zigui, PhD candidate, School of Exercise and Health, Shanghai University of Sport, Shanghai 200438, China
CLC Number:
Cite this article
Zhou Zigui, Liu Jingjing. Association between triglyceride-glucose-body mass index and the risk of hypertension in middle-aged and elderly Chinese population[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(16): 4137-4145.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
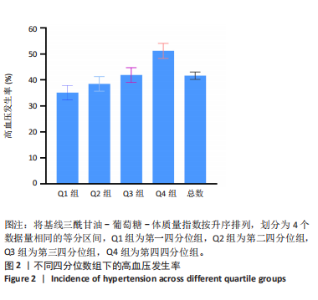
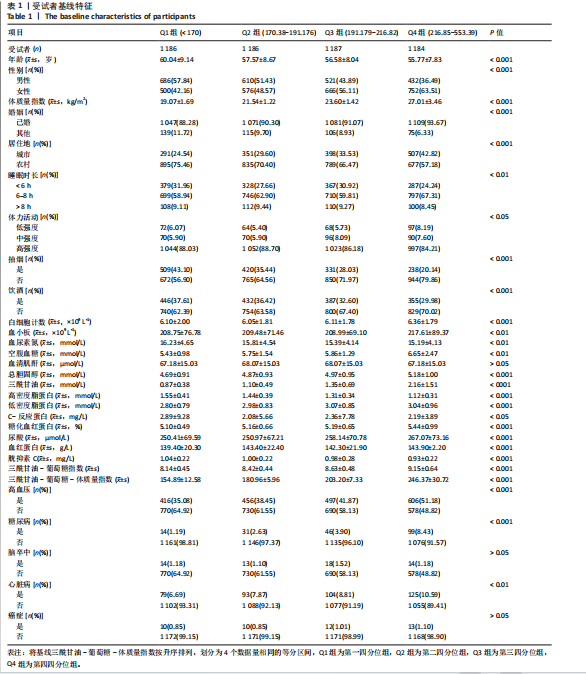
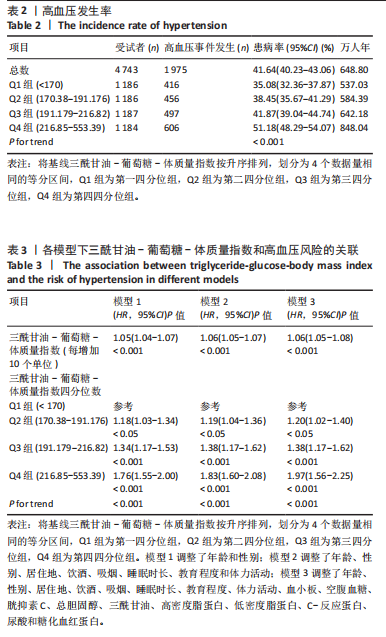
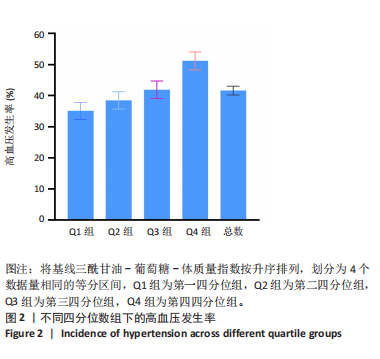
2.1 基线特征 此研究纳入4 743名参与者,女性2 494名,男性2 249名,平均年龄(57.49±8.59)岁。TyG-BMI四分位数分层的基线特征见表1。结果显示,随着TyG-BMI值的增加,年龄、男性比例、农村居住、吸烟、饮酒、高密度脂蛋白和胱抑素C等参数呈下降趋势。相反,女性、城市居住、体质量指数、白细胞计数、空腹血糖、总胆固醇、三酰甘油、糖化血红蛋白、尿酸、血红蛋白、三酰甘油-葡萄糖指数和高血压患病率等参数随TyG-BMI值的升高而增加。 2.2 高血压发生率 在中位随访6.42年期间,新发高血压1 975例,占总人数的41.64% (表2)。高血压发生率为每10 000人年648.80例。各TyG-BMI四分位数的高血压发生率如下:Q1,每10 000人年537.03例;Q2,每10 000人年584.39例;Q3,每10 000人年642.18例;Q4,每10 000人年848.04例。高血压的发生率在各四分位数之间也存在显著差异:Q1,35.08%;Q2,38.45%;Q3,41.87%;Q4,51.18% (图2)。结果表明,与高TyG-BMI组相比,低TyG-BMI组高血压发生率明显更低(P for trend < 0.001)。"
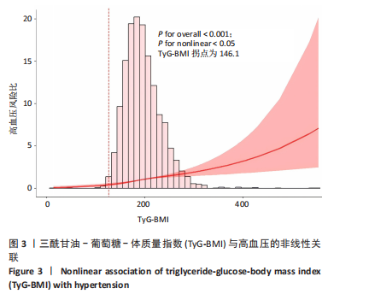
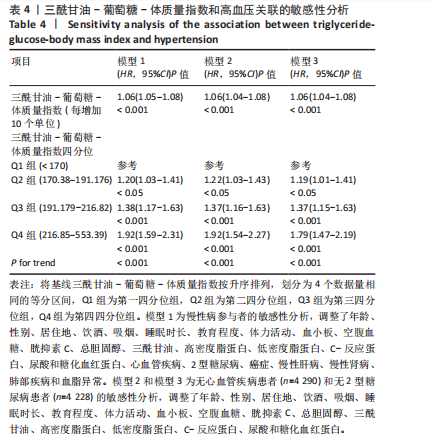
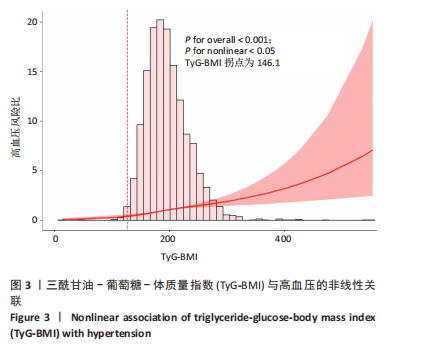
2.3 TyG-BMI与高血压风险的关联 为了探究TyG-BMI与高血压风险之间的关联,此研究建立了3项Cox比例风险回归模型(表3)。在模型1中,TyG-BMI每增加10个单位,高血压发病风险增加5% (HR:1.05,95%CI:1.04-1.07);模型2中,TyG-BMI每增加10个单位,高血压发病风险增加6% (HR:1.06,95%CI:1.05-1.07);模型3中,TyG-BMI每增加10个单位,高血压发病风险增加6% (HR:1.06,95%CI:1.05-1.08)。结果表明,TyG-BMI与高血压发病风险呈显著正相关。 此外,研究将TyG-BMI从连续变量转换为基于四分位的分类变量进行分析。结果显示,与Q1组相比,Q2组患高血压的HR为1.20 (95%CI:1.02-1.40),Q3组为1.38 (95%CI:1.17-1.62),Q4组为1.97 (95%CI:1.56-2.25)。与Q1组相比,Q2组患高血压的风险增加20%,Q3组增加38%,Q4组增加97%。 2.4 Cox比例风险回归模型与平滑曲线拟合 限制性立方样条揭示TyG-BMI与高血压风险之间存在非线性关系(P < 0.001 for overall,P < 0.05 for nonlinear),拐点为146.1(图3)。在确定拐点后,采用了二段式Cox回归模型,进一步探索了拐点两侧的关系。结果显示,拐点前的HR为0.99 (95%CI:0.98-1.01,P > 0.05),拐点后的HR为1.14 (95%CI:1.10-1.19,P < 0.001)。"
| [1] CAREY RM, MORAN AE, WHELTON PK. Treatment of hypertension: A review. JAMA. 2022;328(18):1849-1861. [2] WANG C, YUAN Y, ZHENG M, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality. J Am Coll Cardiol. 2020;75(23):2921-2930. [3] YUSUF S, JOSEPH P, RANGARAJAN S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet. 2020;395(10226):795-808. [4] LEWINGTON S, CLARKE R, QIZILBASH N, et al. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903-1913. [5] MALIK R, GEORGAKIS MK, VUJKOVIC M, et al. Relationship between blood pressure and incident cardiovascular disease: Linear and nonlinear Mendelian randomization analyses. Hypertension. 2021; 77(6):2004-2013. [6] ARVANITIS M, QI G, BHATT DL, et al. Linear and nonlinear Mendelian randomization analyses of the association between diastolic blood pressure and cardiovascular events: The J-curve revisited. Circulation. 2021;143(9):895-906. [7] MCEVOY JW, MCCARTHY CP, BRUNO RM, et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024;45(38):3912-4018. [8] ZHANG M, SHI Y, ZHOU B, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: Findings from six rounds of a national survey. BMJ. 2023;380:e071952. [9] WANG Z, CHEN Z, ZHANG L, et al. China Hypertension Survey Investigators. Status of hypertension in China: Results from the China Hypertension Survey, 2012-2015. Circulation. 2018;137(22):2344-2356. [10] KATSIMARDOU A, IMPRIALOS K, STAVROPOULOS K, et al. Hypertension in metabolic syndrome: Novel insights. Curr Hypertens Rev. 2020; 16(1):12-18. [11] 中华医学会心血管病学分会高血压学组.肥胖相关性高血压管理的中国专家共识[J].中华心血管病杂志,2016,44(3):212-219. [12] YAO Y, WANG B, GENG T, et al. The association between TyG and all-cause/non-cardiovascular mortality in general patients with type 2 diabetes mellitus is modified by age: Results from the cohort study of NHANES 1999-2018. Cardiovasc Diabetol. 2024;23(1):43. [13] LEE SH, PARK SY, CHOI CS. Insulin resistance: From mechanisms to therapeutic strategies. Diabetes Metab J. 2022;46(1):15-37. [14] DZIĘGIELEWSKA-GĘSIAK S, MUC-WIERZGOŃ M. Inflammation and oxidative stress in frailty and metabolic syndromes-two sides of the same coin. Metabolites. 2023;13(4):475. [15] QUESADA O, CLAGGETT B, RODRIGUEZ F, et al. Associations of insulin resistance with systolic and diastolic blood pressure: A study from the HCHS/SOL. Hypertension. 2021;78(3):716-725. [16] 中国高血压防治指南修订委员会.中国高血压防治指南(2024年修订版)[J].中华高血压杂志,2024,32(7):603-700. [17] LEE EY, YANG HK, LEE J, et al. Triglyceride glucose index, a marker of insulin resistance, is associated with coronary artery stenosis in asymptomatic subjects with type 2 diabetes. Lipids Health Dis. 2016;15(1):155. [18] ER LK, WU S, CHOU HH, et al. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS One. 2016;11(3):e0149731. [19] WANG X, LIU J, CHENG Z, et al. Triglyceride glucose-body mass index and the risk of diabetes: A general population-based cohort study. Lipids Health Dis. 2021;20(1):99. [20] YU XR, DU JL, JIANG M, et al. Correlation of TyG-BMI and TyG-WC with severity and short-term outcome in new-onset acute ischemic stroke. Front Endocrinol(Lausanne). 2024;15:1327903. [21] FAN C, GUO M, CHANG S, et al. Elevated TyG-BMI index predicts incidence of chronic kidney disease. Clin Exp Med. 2024;24(1):203. [22] WANG R, DAI L, ZHONG Y, et al. Usefulness of the triglyceride glucose-body mass index in evaluating nonalcoholic fatty liver disease: Insights from a general population. Lipids Health Dis. 2021;20(1):77. [23] ZHAO Y, HU Y, SMITH JP, et al. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1): 61-68. [24] HUO RR, ZHAI L, LIAO Q, et al. Changes in the triglyceride glucose-body mass index estimate the risk of stroke in middle-aged and older Chinese adults: A nationwide prospective cohort study. Cardiovasc Diabetol. 2023;22(1):254. [25] CHEN X, CRIMMINS E, HU PP, et al. Venous blood-based biomarkers in the China Health and Retirement Longitudinal Study: Rationale, design, and results from the 2015 wave. Am J Epidemiol. 2019;188(11):1871-1877. [26] WILLIAMS B, MANCIA G, SPIERING W, et al. ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-3104. [27] SHAO Y, HU H, LI Q, et al. Link between triglyceride-glucose-body mass index and future stroke risk in middle-aged and elderly Chinese: A nationwide prospective cohort study. Cardiovasc Diabetol. 2024;23(1):81. [28] VAN OORT S, BEULENS JWJ, VAN BALLEGOOIJEN AJ, et al. Association of cardiovascular risk factors and lifestyle behaviors with hypertension: A Mendelian randomization study. Hypertension. 2020;76(6):1971-1979. [29] KUANG M, YANG R, HUANG X, et al. Assessing temporal differences in the predictive power of baseline TyG-related parameters for future diabetes: An analysis using time-dependent receiver operating characteristics. J Transl Med. 2023;21(1):299. [30] SELVARAJ S, STEG PG, ELBEZ Y, et al. REACH Registry Investigators. Pulse pressure and risk for cardiovascular events in patients with atherothrombosis: From the REACH registry. J Am Coll Cardiol. 2016; 67(4):392-403. [31] ZHANG Z, GU X, TANG Z, et al. Associations of blood pressure components with risk of cardiovascular events and all-cause death in a Chinese population: A prospective study. J Clin Hypertens(Greenwich). 2022;24(7):825-837. [32] LIU D, QIN P, LIU L, et al. Association of pulse pressure with all-cause and cause-specific mortality. J Hum Hypertens. 2021;35(3):274-279. [33] WANG Y, YANG W, JIANG X. Association between triglyceride-glucose index and hypertension: A meta-analysis. Front Cardiovasc Med. 2021;8:644035. [34] ZHU B, WANG J, CHEN K, et al. A high triglyceride glucose index is more closely associated with hypertension than lipid or glycemic parameters in elderly individuals: A cross-sectional survey from the Reaction Study. Cardiovasc Diabetol. 2020;19(1):112. [35] SHAN S, LI S, LU K, et al. Associations of the triglyceride and glucose index with hypertension stages, phenotypes, and their progressions among middle-aged and older Chinese. Int J Public Health. 2023; 68:1605648. [36] XIN F, HE S, ZHOU Y, et al. The triglyceride glucose index trajectory is associated with hypertension: A retrospective longitudinal cohort study. Cardiovasc Diabetol. 2023;22(1):347. [37] YU L, YANG YX, GONG Z, et al. FcRn-dependent IgG accumulation in adipose tissue unmasks obesity pathophysiology. Cell Metab. 2025;37(3):656-672. [38] JIA G, SOWERS JR, WHALEY-CONNELL AT. Obesity in Hypertension: The Role of the Expanding Waistline Over the Years and Insights Into the Future. Hypertension. 2024;81(4):687-690. [39] HU L, LI J, TANG Z, et al. How does biological age acceleration mediate the associations of obesity with cardiovascular disease? Evidence from international multi-cohort studies. Cardiovasc Diabetol. 2025;24(1):209. [40] ZHAO M, BOVET P, XI B. Weight status change from adolescence to young adulthood and the risk of hypertension and diabetes mellitus. Hypertension. 2020;76(2):583-588. [41] CAI A, LIU L, ZHOU D, et al. Obesity and risk of incident left ventricular hypertrophy in community-dwelling populations with hypertension: An observational study. J Am Heart Assoc. 2024;13(12):e033521. [42] VALENZUELA PL, CARRERA-BASTOS P, CASTILLO-GARCÍA A, et al. Obesity and the risk of cardiometabolic diseases. Nat Rev Cardiol. 2023;20(7):475-494. [43] RAIMI TH, DELE-OJO BF, DADA SA, et al. Triglyceride-Glucose Index and Related Parameters Predicted Metabolic Syndrome in Nigerians. Metab Syndr Relat Disord. 2021;19(2):76-82. [44] ZHOU Z, LIU Q, ZHENG M, et al. Comparative study on the predictive value of TG/HDL-C, TyG and TyG-BMI indices for 5-year mortality in critically ill patients with chronic heart failure: a retrospective study. Cardiovasc Diabetol. 2024;23(1):213. [45] DANG K, WANG X, HU J, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003-2018. Cardiovasc Diabetol. 2024;23(1):8. [46] PENG N, KUANG M, PENG Y, et al. Associations between TyG-BMI and normal-high blood pressure values and hypertension: cross-sectional evidence from a non-diabetic population. Front Cardiovasc Med. 2023;10:1129112. [47] WANG F, HAN L, HU D. Fasting insulin, insulin resistance and risk of hypertension in the general population: A meta-analysis. Clin Chim Acta. 2017;464:57-63. [48] CHE B, ZHONG C, ZHANG R, et al. Triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio as potential cardiovascular disease risk factors: an analysis of UK biobank data. Cardiovasc Diabetol. 2023;22(1):34. [49] LIU Y, ZHU B, ZHOU W, et al. Triglyceride-glucose index as a marker of adverse cardiovascular prognosis in patients with coronary heart disease and hypertension. Cardiovasc Diabetol. 2023;22(1):133. [50] KOSAMI K, KUWABARA M, OKAYAMA A, et al. Body mass index and weight change as predictors of hypertension development: A sex-specific analysis. Nutrients. 2024;17(1):119. [51] CHEN Y, YU W, LV J, et al. Early adulthood BMI and cardiovascular disease: a prospective cohort study from the China Kadoorie Biobank. Lancet Public Health. 2024;9(12):e1005-e1013. |
| [1] | Li Zhenyu, Zhang Siming, Bai Jiaxiang, Zhu Chen. Osthole improves osteogenic differentiation function of bone marrow mesenchymal stem cells under high-glucose conditions [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1641-1648. |
| [2] | Han Nianrong, Huang Yifei, Akram · Osman, Liu Yanlu, Hu Wei . Programmed cell death receptor-1 suppresses osteogenic differentiation of rat bone marrow mesenchymal stem cells in a high-glucose microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(7): 1649-1657. |
| [3] | Wang Jingfeng, Xia Fan, Mao Sujie, Li Xiaolin. Potential target values of low temperature and cold receptor transient receptor potential M8 and glutamate receptor-3/glutamate receptor ionotropic, kainate 2 in the treatment of hypertension [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1499-1507. |
| [4] | Liu Huan, Zeng Shaopeng, Chen Jun, He Linqian, Yang Ying, Zhang Jing. Aging-related dysregulation of glucose metabolism: crossroads of cancer and neurodegenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1527-1538. |
| [5] | Zhang Cuicui, Chen Huanyu, Yu Qiao, Huang Yuxuan, Yao Gengzhen, Zou Xu. Relationship between plasma proteins and pulmonary arterial hypertension and potential therapeutic targets [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1331-1340. |
| [6] | Jiang Yang, Peng Hao, Song Yanping, Yao Na, Song Yueyu, Yin Xingxiao, Li Yanqi, Chen Qigang. Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 975-986. |
| [7] | He Qiwang, , , Chen Bo, Liang Fuchao, Kang Zewei, Zhou Yuan, Ji Anxu, Tang Xialin, . Relationship between Alzheimer’s disease and sarcopenia and body mass index: analysis of GWAS datasets for European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1036-1046. |
| [8] | Wang Peng, Lu Huan, Liu Haifeng, Li Feng. Mechanism by which andrographolide intervenes in insulin resistance in rats with gestational diabetes mellitus [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3058-3065. |
| [9] | Wang Shijie, Hu Xiaoyu, Duan Zhuoran, Tang Yingfeng, Wang Wei . Association between grip strength to weight ratio and new-onset cardiovascular and cerebrovascular diseases: a big data analysis of the China Health and Retirement Longitudinal Study [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3190-3197. |
| [10] |
Zhang Yueting, Li Jinglin, Fu Zhenyi, Yan Fei, Gao Yu, Liu Jiaxin.
Endoplasmic reticulum stress promotes ferroptosis and aggravates cerebral ischemia-reperfusion injury#br#
#br#
[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(11): 2806-2813.
|
| [11] | Zou Yuxi, Chen Yanyan, Jiang Peng, Chen Ting, Ding Lingling. Critical role of lysosomal enzymes in metabolic diseases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(11): 2823-2833. |
| [12] | Cai Zhixing, Xia Qiufang, Chen Lili, Zhu Danyang, Zhu Huiwen, Sun Yanan, Liang Wenyu, Zhao Heqian. Effect of Roujishuncuiyin on the improvement of skeletal muscle insulin resistance in a mouse model of type 2 diabetes mellitus [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7537-7543. |
| [13] | Liu Xuan, Ding Yuqing, Xia Ruohan, Wang Xianwang, Hu Shujuan. Exercise prevention and treatment of insulin resistance: role and molecular mechanism of Keap1/nuclear factor erythroid2-related factor 2 signaling pathway [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7578-7588. |
| [14] | Zhou Lina, , Li Yun, , Liu Xixia, . Effects of different concentrations of hypertonic glucose in the repair of tendon injury in rats [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(32): 6885-6892. |
| [15] | Cui Yuena, Chen Xiaoyu, Liang Meiting, Chen Wujin, He Yi, Dilinur·Ekpa, Du Manxi, Zhu Yuqiu, Abuduwupuer·Haibier, Sun Yuping. Differences of calorie restriction and time-restricted feeding on metabolic indices and gut microbiota of mice [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6449-6456. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||