Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (4): 975-986.doi: 10.12307/2025.913
Previous Articles Next Articles
Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects
Jiang Yang1, Peng Hao1, Song Yanping2, Yao Na2, Song Yueyu1, Yin Xingxiao1, Li Yanqi1, Chen Qigang2
- 1School of Physical Education, Yunnan Normal University, Kunming 650500, Yunnan Province, China; 2Department of Rehabilitation Medicine, Third Affiliated Hospital of Yunnan University of Chinese Medicine (Kunming Municipal Hospital of Traditional Chinese Medicine), Kunming 650011, Yunnan Province, China
-
Received:2024-10-10Accepted:2024-11-25Online:2026-02-08Published:2025-05-21 -
Contact:Chen Qigang, Chief physician, Department of Rehabilitation Medicine, Third Affiliated Hospital of Yunnan University of Chinese Medicine (Kunming Municipal Hospital of Traditional Chinese Medicine), Kunming 650011, Yunnan Province, China Co-corresponding author: Yao Na, MS, Therapist-in-charge, Department of Rehabilitation Medicine, Third Affiliated Hospital of Yunnan University of Chinese Medicine (Kunming Municipal Hospital of Traditional Chinese Medicine), Kunming 650011, Yunnan Province, China -
About author:Jiang Yang, Master candidate, School of Physical Education, Yunnan Normal University, Kunming 650500, Yunnan Province, China -
Supported by:Yunnan Provincial Science and Technology Plan Project, No. 202201AH070001-060 (to CQG); Yunnan Provincial Joint Special Youth Project of Traditional Chinese Medicine, No. 202301AZ070001-154 (to YN)
CLC Number:
Cite this article
Jiang Yang, Peng Hao, Song Yanping, Yao Na, Song Yueyu, Yin Xingxiao, Li Yanqi, Chen Qigang. Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 975-986.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

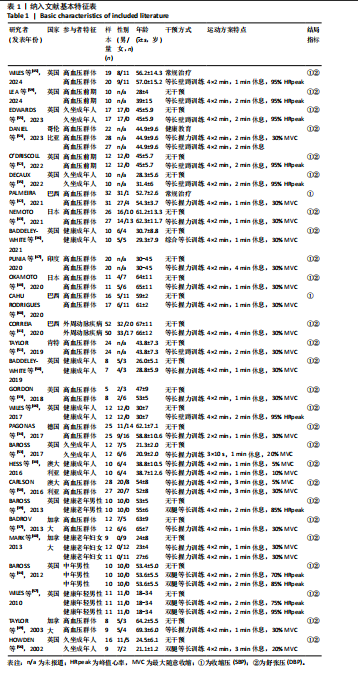
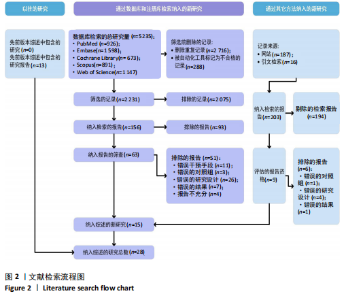
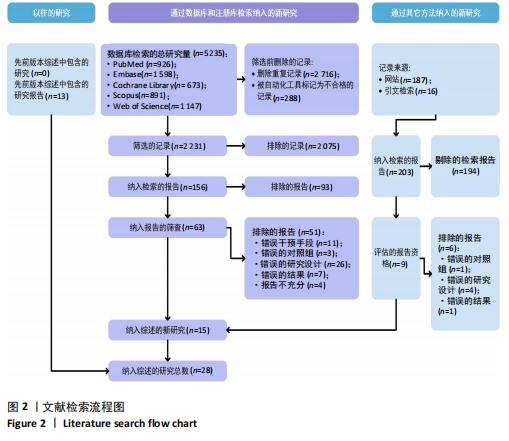
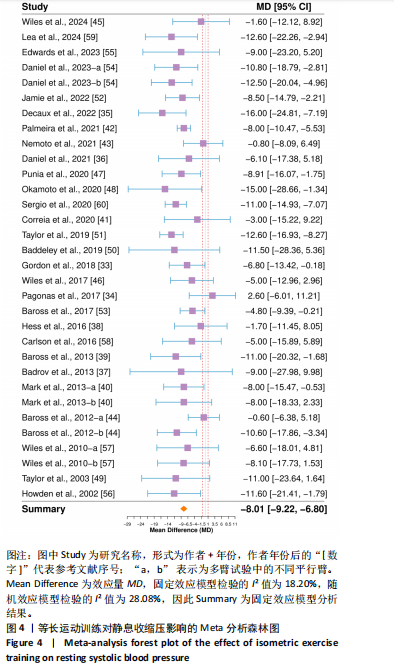
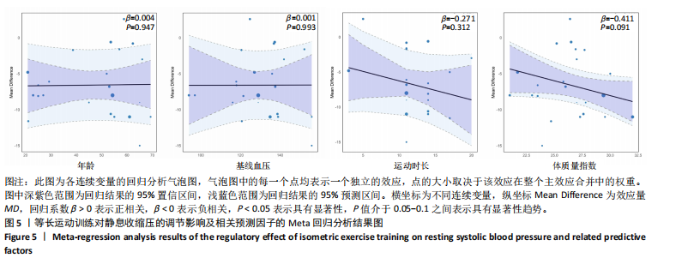
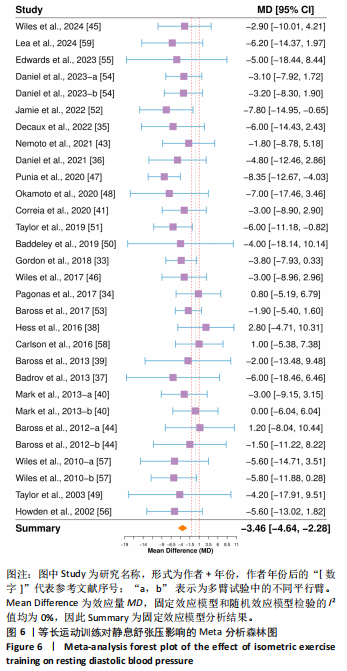
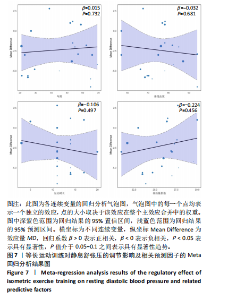
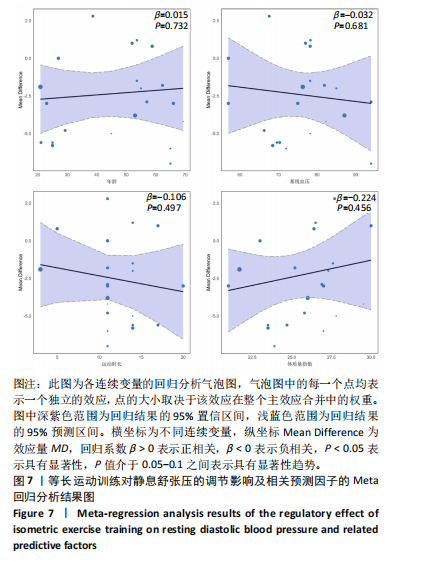
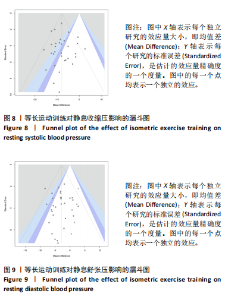
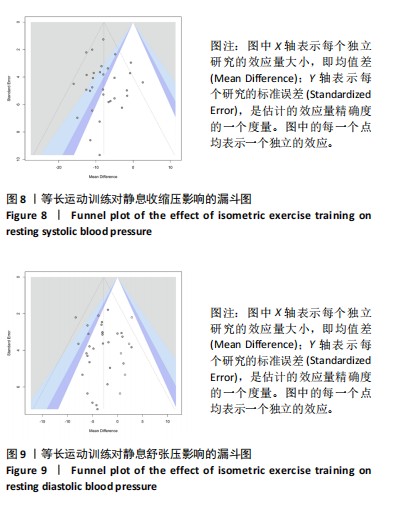
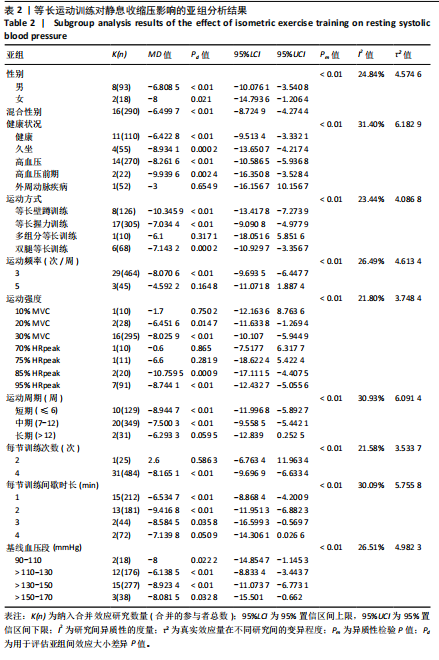
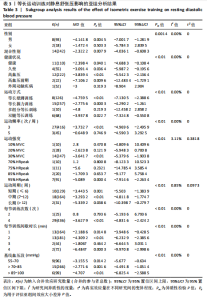
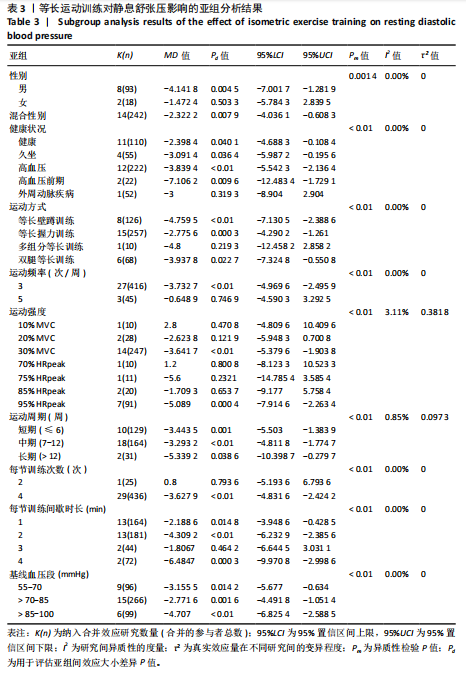
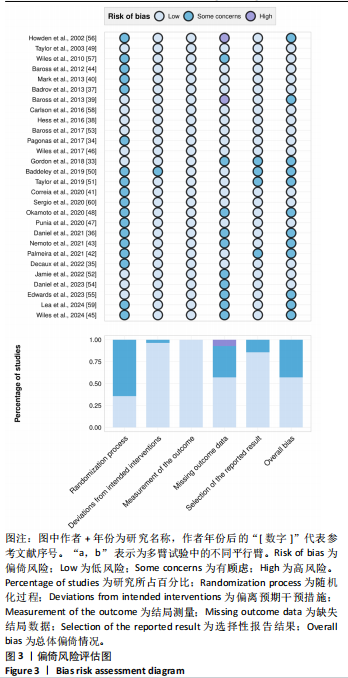
盖32项随机对照试验),共涉及977名参与受试者。单例研究参与者人数为5-52人,年龄为18-78岁,单一性别或混合性别报道,参与者群体特征为健康(194人,19.9%)、久坐(103人,10.5%)、高血压(534人,54.7%)、高血压前期(44人,4.5%)、外周动脉疾病(102人,10.4%)。28篇研究中报道了32项收缩压(SBP)条件和30项舒张压(DBP)条件,运动方式为等长握力训练(IGST)有17项,等长壁蹲训练(IWST)有8项,双腿等长训练(BILT)有6项,综合等长训练(IIT)有1项。 2.3 文献质量评估结果 根据RoB 2.0偏倚风险评估工具的要求,对随机化过程、偏离预期干预措施、结局测量、缺失结局数据、选择性报告结果和总体偏倚情况这6个栏目进行评估。除结局测量无风险外,其他栏目均存在一定风险。详情见图3。 2.4 Meta分析结果 2.4.1 等长运动训练对静息收缩压的影响 32项随机对照试验分析结果显示[33-60],等长运动组与对照组相比对收缩压有显著的降压效果(MD=-8.01,95%CI:-9.22至-6.80,P < 0.01),研究间异质性较低(I2=18.20%,P=0.18),见图4。敏感性分析结果显示,逐一删除每个研究的Meta分析效应量(MD值)在-7.62至-8.35,置信区间范围为-9.59至-6.36,P值均显著,证实以上等长运动训练对改善收缩压的显著效果。 亚组分析结果见表2,等长运动训练的降压作用受到性别、健康状况、运动方式、运动频率、运动强度、运动周期、每节训练次数、每节训练间歇时长和基线血压水平因素的显著影响(P < 0.05)。具体而言,该训练在女性(MD=-8,P=0.021)、高血压前期(MD=-9.939 6,P=0.002 4)、基线收缩压为130-150 mmHg (MD=-8.923 4,P < 0.01)群体中的降压效果最好。此外,运动类型为等长壁蹲训练(MD=-10.345 9,P < 0.01),运动频率为每周3次(MD=-8.070 6,P < 0.01),运动强度为85% HRpeak (MD=-10.759 5,P=0.000 9),运动周期为短期(≤6周)(MD=-8.944 7,P < 0.01),每次训练4组运动(MD=-8.165 1,P < 0.01),每组运动间歇2 min (MD=-9.416 8,P < 0.01)的等长运动训练方案能达到最佳的降压效应。 Meta回归分析结果见图5,未发现参与者的年龄、基线血压(收缩压)、运动时长、体质量指数因素对等长运动训练的降低收缩压作用存在显著的影响(P > 0.05)。但值得注意的是,参与者的体质量指数(β=-4.11,P=0.091)虽未达到统计显著性水平,但显示出接近显著性的负向趋势,P值介于0.05与0.1之间。 2.4.2 等长运动训练对静息舒张压的影响 30项随机对照试验分析结果显示[33-41,43-59],等长运动组与对照组相比对舒张压有显著的降压效果(MD=-3.46,95%CI:-4.64至-2.28,P < 0.01),研究间异质性极低(I2=0%,P=0.89),见图6。敏感性分析结果显示,逐一删除每个研究的Meta分析效应量(MD值)在-3.061 528到-3.655 455,置信区间范围为-4.908 819到-1.834 743,P值均差异显著,同样证实以上等长运动训练对改善舒张压的显著效果。 亚组分析结果见表3,等长运动训练的降压作用受到性别、健康状况、运动方式、运动频率、运动强度、运动周期、每节训练次数、每节训练间歇时长和基线血压水平因素的显著影响(P < 0.05)。具体而言,该运动在男性(MD=-4.141 8,P=0.004 5)、高血压前期(MD=-7.106 2,P=0.009 6)、基线舒张压为85-100 mmHg (MD=-4.707,P < 0.01)群体中的降压效果最好。此外,运动类型为等长壁蹲训练(MD=-4.759 5,P < 0.01),运动频率为每周3次(MD=-3.732 7,P < 0.01),运动强度为95% HRpeak (MD=-5.089,P=0.000 4),运动周期为长期(> 12周)(MD=-5.339 2,P=0.038 6),每次训练4组运动(MD=-3.627 9,P < 0.01),每组运动间歇4 min (MD=-6.484 7,P=0.000 3)的等长运动训练方案能达到最佳的降压效应。 Meta回归分析结果见图7,未发现参与者的年龄、基线血压(收缩压)、运动时长、体质量指数因素对等长运动训练的降低舒张压作用存在显著的影响(P > 0.05)。 2.5 发表偏倚结果 图8,9分别展示了基于Egger’s检验后所绘制的等长运动训练对静息收缩压和舒张压影响的漏斗图。Egger’s检验结果显示,两者的P > 0.05,表明在这2个指标中不存在显著的发表偏倚。 2.6 证据等级评估结果 此研究基于GRADE框架的证据等级评估结果见表4。"
| [1] JOSEPH P, LEONG D, MCKEE M, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circulation Res. 2017;121(6):677-694. [2] LEONG DP, JOSEPH PG, MCKEE M, et al. Reducing the global burden of cardiovascular disease, part 2: prevention and treatment of cardiovascular disease. Circulation Res. 2017;121(6):695-710. [3] ZHOU B, BENTHAM J, DI CESARE M, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37-55. [4] THOM SM, CRUICKSHANK K, STANTON A, et al. Differential impact of blood pressure–lowering drugs on central aortic pressure and clinical outcomes. Circulation. 2006;113:1213-1225. [5] WANG G, GROSSE SD, SCHOOLEY MW. Conducting research on the economics of hypertension to improve cardiovascular health. Am J Prev Med. 2017;53(6): S115-S117. [6] ASSIRI GA, SHEBL NA, MAHMOUD MA, et al. What is the epidemiology of medication errors, error-related adverse events and risk factors for errors in adults managed in community care contexts? A systematic review of the international literature. BMJ Open. 2018;8(5):e019101. [7] WHELTON PK, CAREY RM, ARONOW WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2018; 71(19):2199-2269. [8] HALLAL PC, DUMITH SC, REICHERT FF, et al. Cross-sectional and longitudinal associations between physical activity and blood pressure in adolescence: birth cohort study. J Phys Act Health. 2011;8(4):468-474. [9] DE SOUZA VIEIRA V, DA COSTA AGUIAR S, CAMPOS MC, et al. Light-intensity physical activity and sedentary behavior are associated with blood pressure levels in adolescents. Pediatr Exerc Sci. 2024; 1(aop):1-9. [10] GUAN T, CAO M, ZHENG C, et al. Dose-response association between physical activity and blood pressure among Chinese adults: a nationwide cross-sectional study. J Hypertens. 2024;42(2):360-370. [11] STAMATAKIS E, GALE J, BAUMAN A, et al. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019; 73(16):2062-2072. [12] DIAZ KM, SHIMBO D. Physical activity and the prevention of hypertension. Curr Hypertens Rep. 2013;15:659-668. [13] CORNELISSEN VA, SMART NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473. [14] BÖRJESSON M, ONERUP A, LUNDQVIST S, et al. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. 2016;50(6):356-361. [15] ARNETT DK, BLUMENTHAL RS, ALBERT MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; 74(10):1376-1414. [16] SCHULTZ MG, CURRIE KD, HEDMAN K, et al. The identification and management of high blood pressure using exercise blood pressure: current evidence and practical guidance. Int J Environ Res Public Health. 2022;19(5):2819. [17] CLARKE SL. Hypertension in adults: initial evaluation and management. Am Fam Physician. 2023;108(4):352-359. [18] MILLAR PJ, MCGOWAN CL, CORNELISSEN VA, et al. Evidence for the role of isometric exercise training in reducing blood pressure: potential mechanisms and future directions. Sports Med. 2014;44:345-356. [19] EDWARDS JJ, COLEMAN DA, RITTI-DIAS RM, et al. Isometric exercise training and arterial hypertension: an updated review. Sports Med. 2024;54(6):1459-1497. [20] EDWARDS JJ, DEENMAMODE AHP, GRIFFITHS M, et al. Exercise training and resting blood pressure: a large-scale pairwise and network meta-analysis of randomized controlled trials. Br J Sports Med. 2023;57(20):1317-1326. [21] KELLEY GA, KELLEY KS, STAUFFER BL. Isometric exercise and inter-individual response differences on resting systolic and diastolic blood pressure in adults: a meta-analysis of randomized controlled trials. Blood Pressure. 2021;30(5):310-321. [22] HANDFORD HJ, PARMENTER BJ, MCLEOD KA, et al. The effectiveness and safety of isometric resistance training for adults with high blood pressure: a systematic review and meta-analysis. Hypertens Res. 2021;44(11):1373-1384. [23] BAFFOUR-AWUAH B, PEARSON MJ, DIEBERG G, et al. Isometric resistance training to manage hypertension: systematic review and meta-analysis. Curr Hypertens Rep. 2023;25(4):35-49. [24] PAGE MJ, MCKENZIE JE, BOSSUYT PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [25] HIGGINS JP. Cochrane handbook for systematic reviews of interventions. Cochrane Collaboration and John Wiley & Sons Ltd. 2008. [26] CUMPSTON M, LI T, PAGE MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;2019(10): ED000142. [27] HIGGINS JPT, SAVOVIĆ J, PAGE MJ, et al. Assessing risk of bias in a randomized trial. Cochrane Handbook for Systematic Reviews of Interventions; 2019:205-228. [28] DERSIMONIAN R, LAIRD N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986; 7(3):177-188. [29] MOSTAFAEI H, GHOJAZADEH M, HAJEBRAHIMI S. Fixed-effect versus random-effects models for meta-analyses: fixed-effect models. Eur Urol Focus. 2023; 9(5):691-692. [30] NAKAGAWA S, NOBLE DWA, SENIOR AM, et al. Meta-evaluation of meta-analysis: ten appraisal questions for biologists. BMC Biol. 2017;15:1-14. [31] BINNEY ZO, MANSOURNIA MA. Methods matter: (mostly) avoid categorising continuous data-a practical guide. Br J Sports Med. 2024;58(5):241-243. [32] RICO-GONZÁLEZ M, PINO-ORTEGA J, CLEMENTE F, et al. Guidelines for performing systematic reviews in sports science. Biol Sport. 2022;39(2):463-471. [33] GORDON BDH, THOMAS EV, WARREN-FINDLOW J, et al. A comparison of blood pressure reductions following 12-weeks of isometric exercise training either in the laboratory or at home. J Am Soc Hypertens. 2018;12(11):798-808. [34] PAGONAS N, VLATSAS S, BAUER F, et al. Aerobic versus isometric handgrip exercise in hypertension: a randomized controlled trial. J Hypertens. 2017;35(11):2199-2206. [35] DECAUX A, EDWARDS JJ, SWIFT HT, et al. Blood pressure and cardiac autonomic adaptations to isometric exercise training: a randomized sham‐controlled study. Physiological Reports. 2022;10(2):e15112. [36] BADDELEY-WHITE DS, WOOD CN, MCGOWAN CLM, et al. Blood pressure-lowering efficacy of a 6-week multi-modal isometric exercise intervention. Blood Pressure Monit. 2021;26(1):30-38. [37] BADROV MB, HORTON S, MILLAR PJ, et al. Cardiovascular stress reactivity tasks successfully predict the hypotensive response of isometric handgrip training in hypertensives. Psychophysiology. 2013; 50(4):407-414. [38] HESS NCL, CARLSON D, INDER JD, et al. Clinically meaningful blood pressure reductions with low intensity isometric handgrip exercise: a randomized trial. 2016. 2016;65(3):46146-46148. [39] BAROSS AW, WILES JD, SWAINE IL. Double-leg isometric exercise training in older men. Open Access J Sports Med. 2013;4:33-40. [40] BADROV MB, BARTOL CL, DIBARTOLOMEO MA, et al. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113:2091-2100. [41] CORREIA A, OLIVEIRA PL, FARAH BQ, et al. Effects of isometric handgrip training in patients with peripheral artery disease: a randomized controlled trial. J Am Heart Assoc. 2020;9(4):e013596. [42] PALMEIRA AC, FARAH BQ, SILVA GO, et al. Effects of isometric handgrip training on blood pressure among hypertensive patients seen within public primary healthcare: a randomized controlled trial. Sao Paulo Med J. 2021;139(6):648-656. [43] NEMOTO Y, SATOH T, TAKAHASHI T, et al. Effects of isometric handgrip training on home blood pressure measurements in hypertensive patients: a randomized crossover study. Intern Med. 2021;60(14): 2181-2188. [44] BAROSS AW, WILES JD, SWAINE IL. Effects of the intensity of leg isometric training on the vasculature of trained and untrained limbs and resting blood pressure in middle‐aged men. Int J Vasc Med. 2012;2012(1):964697. [45] WILES JD, SANTER E, REES-ROBERTS M, et al. Feasibility study to assess the delivery of a novel isometric exercise intervention for people with high blood pressure in a healthcare setting. medRxiv. 2024;2024:24302961. [46] WILES JD, GOLDING N, COLEMAN D. Home-based isometric exercise training induced reductions in resting blood pressure. Eur J Appl Physiol. 2017;117:83-93. [47] PUNIA S, KULANDAIVELAN S. Home‐based isometric handgrip training on RBP in hypertensive adults-Partial preliminary findings from RCT. Physiotherapy Res Int. 2020;25(1):e1806. [48] OKAMOTO T, HASHIMOTO Y, KOBAYASHI R. Isometric handgrip training reduces blood pressure and wave reflections in East Asian, non-medicated, middle-aged and older adults: a randomized control trial. Aging Clin Exp Res. 2020;32:1485-1491. [49] TAYLOR AC, MCCARTNEY N, KAMATH MV, et al. Isometric training lowers resting blood pressure and modulates autonomic control. Med Sci Sports Exerc. 2003;35(2):251-256. [50] BADDELEY-WHITE DS, MCGOWAN CL, HOWDEN R, et al. Blood pressure lowering effects of a novel isometric exercise device following a 4-week isometric handgrip intervention. Open Access J Sports Med. 2019;10:89-98. [51] TAYLOR KA, WILES JD, COLEMAN DA, et al. Neurohumoral and ambulatory haemodynamic adaptations following isometric exercise training in unmedicated hypertensive patients. J Hypertens. 2019; 37(4):827-836. [52] O’DRISCOLL JM, EDWARDS JJ, COLEMAN DA, et al. One year of isometric exercise training for blood pressure management in men: a prospective randomized controlled study. J Hypertens. 2022;40(12):2406-2412. [53] BAROSS AW, HODGSON DA, PADFIELD SL, et al. Reductions in resting blood pressure in young adults when isometric exercise is performed while walking. J Sports Med. 2017;2017(1):7123834. [54] COHEN DD, AROCA-MARTINEZ G, CARREÑO-ROBAYO J, et al. Reductions in systolic blood pressure achieved by hypertensives with three isometric training sessions per week are maintained with a single session per week. J Clin Hypertens. 2023;25(4):380-387. [55] EDWARDS JJ, JALALUDEEN N, BEQIRI A, et al. The effect of isometric exercise training on arterial stiffness: a randomized crossover controlled study. Physiol Rep. 2023;11(10):e15690. [56] HOWDEN R, LIGHTFOOT JT, BROWN SJ, et al. The effects of isometric exercise training on resting blood pressure and orthostatic tolerance in humans. Exp Physiol. 2002; 87(4):507-515. [57] WILES JD, COLEMAN DA, SWAINE IL. The effects of performing isometric training at two exercise intensities in healthy young males. Eur J Appl Physiol. 2010;108:419-428. [58] CARLSON DJ, INDER J, PALANISAMY SKA, et al. The efficacy of isometric resistance training utilizing handgrip exercise for blood pressure management: a randomized trial. Medicine. 2016;95(52):e5791. [59] LEA J WD, O’DRISCOLL JM, WILES JD. The implementation of a home-based isometric wall squat intervention using ratings of perceived exertion to select and control exercise intensity: a pilot study in normotensive and pre-hypertensive adults. Eur J Appl Physiol. 2024;124(1):281-293. [60] CAHU RODRIGUES SL, FARAH BQ, SILVA G, et al. Vascular effects of isometric handgrip training in hypertensives. Clin Exp Hypertens. 2020;42(1):24-30. [61] LOPEZ-VALENCIANO A, RUIZ-PEREZ I, AYALA F, et al. Updated systematic review and meta-analysis on the role of isometric resistance training for resting blood pressure management in adults. J Hypertens. 2019;37(7):1320-1333. [62] EDWARDS J, DE CAUX A, DONALDSON J, et al. Isometric exercise versus high-intensity interval training for the management of blood pressure: a systematic review and meta-analysis. Br J Sports Med. 2022; 56(9):506-514. [63] CARLSON DJ, DIEBERG G, HESS NC, et al. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89(3):327-334. [64] EDWARDS JJ, WILES J, O’DRISCOLL J. Mechanisms for blood pressure reduction following isometric exercise training: a systematic review and meta-analysis. J Hypertens. 2022;40(11):2299-2306. [65] GLASER S, FRIEDRICH N, KOCH B, et al. Exercise blood pressure and heart rate reference values. Heart Lung Circ. 2013; 22(8):661-667. [66] DEVEREUX GR, WILES JD, HOWDEN R. Immediate post-isometric exercise cardiovascular responses are associated with training-induced resting systolic blood pressure reductions. Eur J Appl Physiol. 2015;115:327-333. [67] BETZ HH, EISENMANN JC, LAURSON KR, et al. Physical activity, BMI, and blood pressure in US youth: NHANES 2003-2006. Pediatr Exerc Sci. 2018;30(3):418-425. [68] DE MEDEIROS REGO ML, CABRAL DAR, DA COSTA KG, et al. Systolic blood pressure mediates the association between body mass index and inhibitory control in children. Biol Psychol. 2020;157:107988. [69] CONEGLIAN JC, BARCELOS GT, BANDEIRA A CN, et al. Acute blood pressure response to different types of isometric exercise: a systematic review with meta-analysis. Rev Cardiovasc Med. 2023;24(2):60. [70] DE OLIVEIRA PC, LEHNEN AM, WACLAWOWSKY G. Effect of isometric exercise on blood pressure in prehypertensive and hypertensive individuals: protocol for a systematic review and meta-analysis of randomized controlled trials. Syst Rev. 2022;11(1):100. [71] DEVEREUX GR, WILES JD, SWAINE I. Markers of isometric training intensity and reductions in resting blood pressure. J Sports Sci. 2011;29(7):715-724. [72] ENOKA RM, DUCHAITEAU J. Muscle fatigue: what, why and how it influences muscle function. J Physiol. 2008;586(1):11-23. [73] SWIFT HT, O’DRISCOLL JM, COLEMAN DD, et al. Acute cardiac autonomic and haemodynamic responses to leg and arm isometric exercise. Eur J Appl Physiol. 2022;122(4):975-985. [74] ALMEIDA JPAS, BESSA M, LOPES LTP, et al. Isometric handgrip exercise training reduces resting systolic blood pressure but does not interfere with diastolic blood pressure and heart rate variability in hypertensive subjects: a systematic review and meta-analysis of randomized clinical trials. Hypertens Res. 2021;44(9):1205-1212. [75] ETTEHAD D, EMDIN CA, KIRAN A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957-967. [76] STRANDBERG TE, PITKÄLÄ K. What is the most important component of blood pressure: systolic, diastolic or pulse pressure? Curr Opin Nephrol Hypertens. 2003;12(3):293-297. [77] TIAN Z, VOLLMER BARBOSA C, LANG H, et al. Efficacy of pharmacological and interventional treatment for resistant hypertension: a network meta-analysis. Cardiovasc Res. 2024;120(1):108-119. [78] FLACK JM, ADEKOLA B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30(3):160-164. |
| [1] | Wang Jingfeng, Xia Fan, Mao Sujie, Li Xiaolin. Potential target values of low temperature and cold receptor transient receptor potential M8 and glutamate receptor-3/glutamate receptor ionotropic, kainate 2 in the treatment of hypertension [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1499-1507. |
| [2] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [3] | Zhang Cuicui, Chen Huanyu, Yu Qiao, Huang Yuxuan, Yao Gengzhen, Zou Xu. Relationship between plasma proteins and pulmonary arterial hypertension and potential therapeutic targets [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1331-1340. |
| [4] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [5] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [6] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [7] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [8] | Tian Jinxin, Zhao Yuxin, Hu Tong, Cui Tiantian, Ma Lihong. Effects of different transcranial magnetic stimulation modes on refractory depression in adults: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7639-7648. |
| [9] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [10] | Qiao Zhengji, Chai Niubing, Zheng Luyao, Gao Yunna, Wang Yang. Effect of whole‑body vibration training on bone mineral density in postmenopausal women: a meta‑analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5195-5202. |
| [11] | Zhao Yuxin, Zhang Deqi, Bi Hongyan. Effect of different stimulation modalities of non-invasive brain stimulation on cognitive function in patients with Parkinson’s disease: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5212-5223. |
| [12] | Hu Tong, Li Xuan, Yuan Jing, Wang Wei. Different electromagnetic stimulation programs improve post-stroke dysphagia: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5224-5236. |
| [13] | Chai Jinlian, Sun Tiefeng, Li Wei, Zhang Bochun, Li Guangzheng, Shao Xuekun, Wang Ping, Liang Xuezhen. Cathepsins and osteonecrosis: analysis based on European samples from the FinnGen Database and IEU OpenGWAS Database [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(24): 5254-5262. |
| [14] | Lin Qing, Liu Huan, Cheng Yongzhong, Jiang Junjie, Li Yongyao, Li Guangyao. Meta-analysis of external stent fixation and internal plate fixation for treatment of comminuted distal radius fractures [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(21): 4602-4611. |
| [15] | Yin Mingyue, Liu Qian, Xu Xiongzhuang, Ma Zhiying, Deng Shengji, Deng Jianfeng, Li Yongming. Acute effects and moderators of sedentary interruption on vascular function in adults: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(17): 3684-3696. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||