Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (4): 997-1007.doi: 10.12307/2026.019
Previous Articles Next Articles
Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis
Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi
- School of Physical Education, Northeast Normal University, Changchun 130024, Jilin Province, China
-
Received:2024-12-05Accepted:2025-02-20Online:2026-02-08Published:2025-05-22 -
Contact:Xu Hongqi, PhD, Professor, Doctoral supervisor, School of Physical Education, Northeast Normal University, Changchun 130024, Jilin Province, China -
About author:Sun Jiahe, Master, School of Physical Education, Northeast Normal University, Changchun 130024, Jilin Province, China -
Supported by:National Social Science Foundation, No. 22BTY075 (to XHQ)
CLC Number:
Cite this article
Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
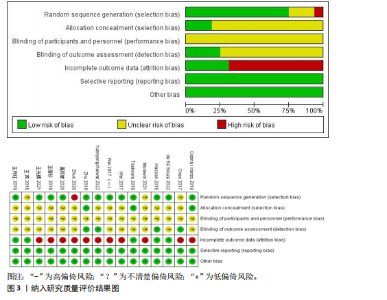
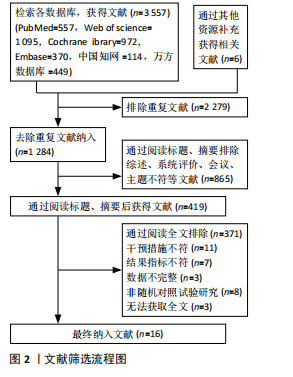
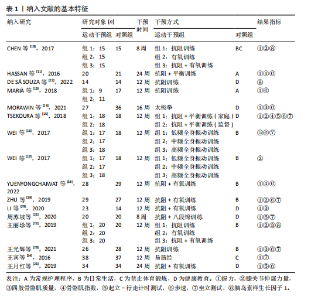
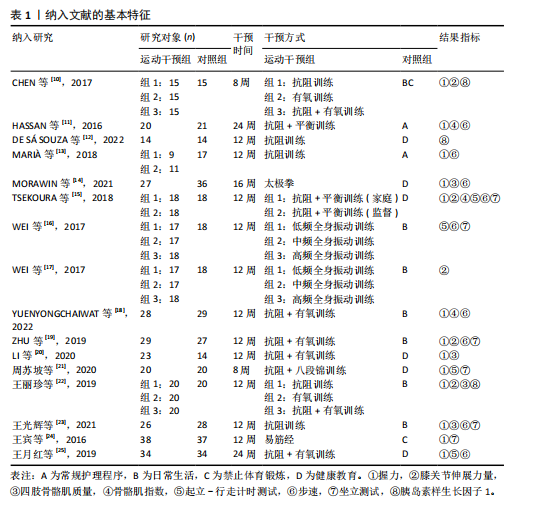
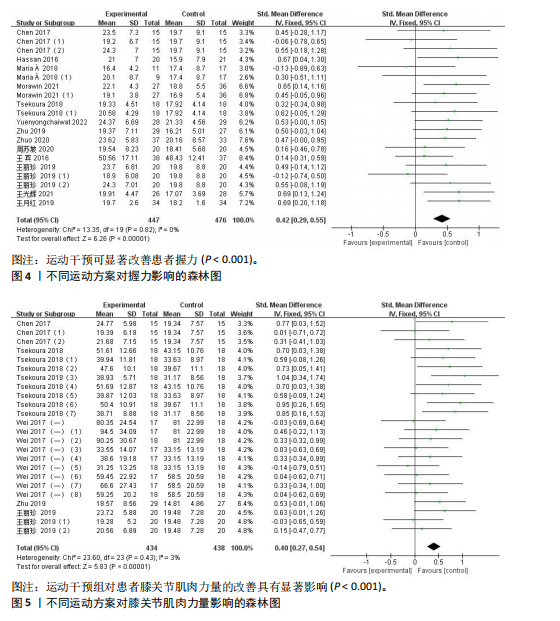
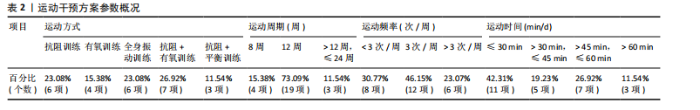
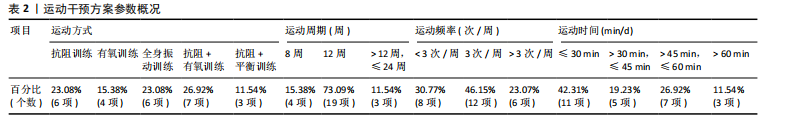
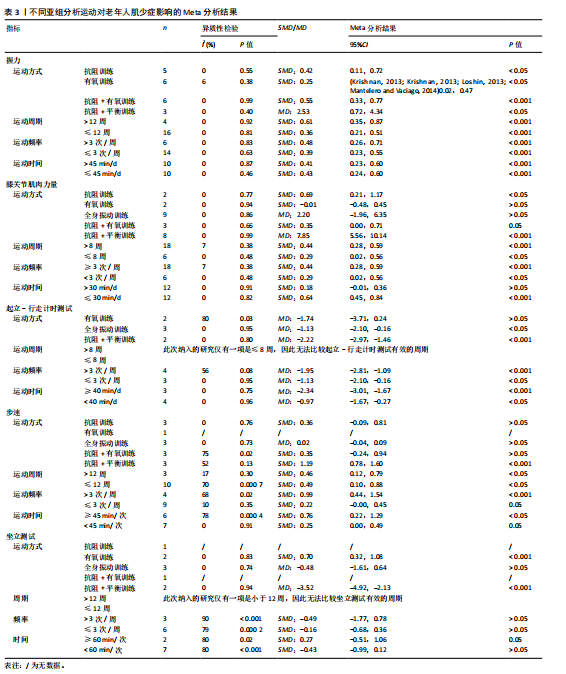
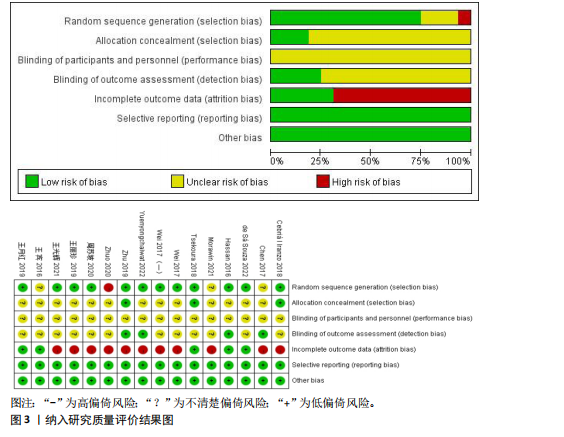
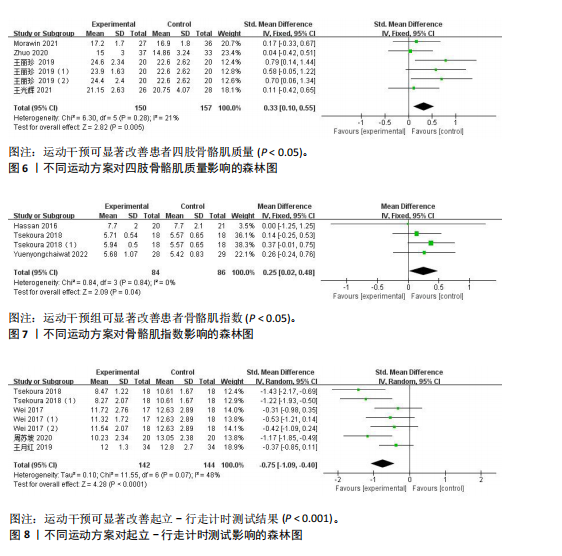
运动干预方案包括4部分内容,即运动方式、运动周期、运动频率、运动时间(表2)。运动方式划分为抗阻训练、有氧训练、全身振动训练等,抗阻联合有氧训练占比最高,为26.92%(7项)。运动周期8-24周不等,其中运动周期为12周的方案占比最高,为73.09%(19项);每周运动频率为3次占比最高,为46.15%(12项);每天运动时间≤30 min占比最高,为42.31%(11项)。 2.3 文献质量评价结果 偏倚风险结果见图3,部分条目被评为“低风险”,因而此次研究所有文献均为B级。 2.4 主要结局指标 2.4.1 肌肉力量 (1)握力:20项随机对照试验(共13篇文献纳入此次研究,包含26项随机对照试验,若一篇文献中包含多种研究方法,则每种方法视为一项独立的研究)报告了患有肌少症及其合并症人群进行运动干预前后握力的结果[10-11,13-15,18-25](图4),I2=0%,P=0.82,因此采用固定效应模型。由于握力测量的结局指标不同(惯用手、非惯用手、双手等),因此使用SMD计算效应量大小,SMD=0.42,95%CI(0.29,0.55),P < 0.001,证明运动干预能够改善握力,从而提高肌肉力量。 为了评估有效的运动方案对患有肌少症及其合并症老年人握力的影响,亚组分析结果显示,运动方式、周期、频率以及时间均显著优于对照组(表3)。 (2)膝关节肌肉力量:24项随机对照试验测量了运动干预前后对膝关节肌肉力量的影响[10,15,17,19,22](图5)。I2=3%,P=0.43,因此采用固定效应模型。由于膝关节肌肉力量的单位不同(Nm、kg等),因此使用SMD计算效应量大小,SMD=0.40,95%CI(0.27,0.54),P < 0.001,证明运动干预是提高膝关节肌肉力量的有效方法。 为了评估有效的运动方案对患有肌少症及其合并症老年人膝关节肌肉力量的影响(表3),亚组分析结果显示,在运动方式中,与有氧训练(SMD=-0.01,95%CI:-0.48-0.45,P > 0.05)、全身振动训练(MD=2.20,95%CI:-1.96-6.35,P > 0.05)和抗阻"
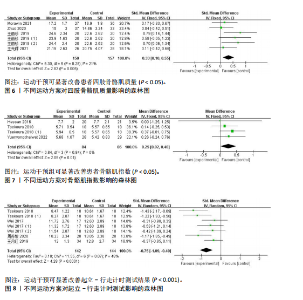
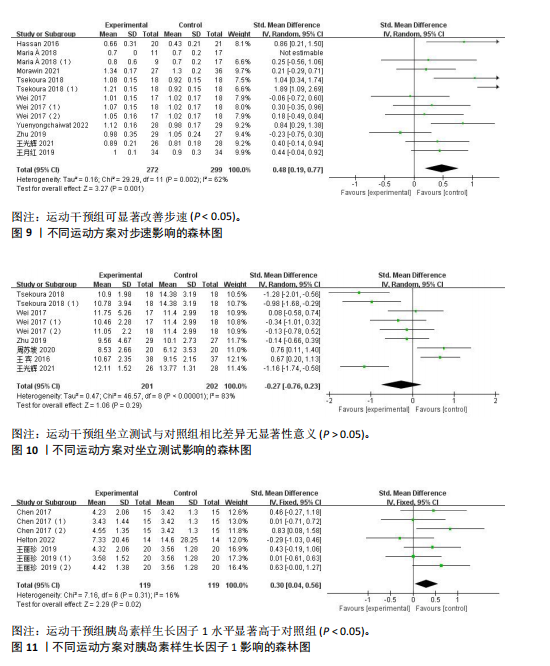
联合有氧训练(SMD=0.35,95%CI:0.00-0.71,P=0.05)相比,抗阻训练(SMD=0.69,95%CI:0.21-1.17,P < 0.05)、抗阻联合平衡训练(MD=7.85,95%CI:5.56-10.14,P < 0.001)对增加老年人膝关节肌肉力量有更显著的促进效果;而运动周期> 8周(SMD=0.44,95%CI:0.28-0.59,P < 0.001)或≤8周(SMD=0.29,95%CI:0.02-0.56,P < 0.05)均能产生中等效应量的影响;将运动频率分为≥3次/周(SMD=0.44,95%CI:0.28-0.59,P < 0.001)和< 3次/周(SMD=0.29,95%CI:0.02-0.56,P < 0.05),均能产生中等效应量的影响;运动时间≤30 min/d(SMD=0.64,95%CI:0.45-0.84,P < 0.001)相比> 30 min/d(SMD=0.18,95%CI:-0.01-0.36,P > 0.05),对增加老年人膝关节肌肉力量有更显著的促进效果,呈现中等效应。 2.4.2 肌肉质量 肌肉质量是指全身或特定部位(如四肢)的骨骼肌含量,是评估肌少症的核心指标之一。同时,肌肉质量减少也是肌少症的必要诊断条件。 (1)四肢骨骼肌质量:6项随机对照试验测量了运动干预前后对四肢骨骼肌质量的影响[14,20,22-23](图6)。I2=21%,P=0.28,因此采用固定效应模型。由于四肢骨骼肌质量的单位不同(kg,%),因此使用SMD计算效应量大小,SMD=0.33,95%CI:0.10-0.55,P < 0.05,证明运动干预是可以帮助改善四肢骨骼肌质量。 (2)骨骼肌指数:4项随机对照试验报告了患有肌少症及其合并症人群进行运动干预前后骨骼肌指数的结果[11,15,18](图7),I2=0%,P=0.84,因此采用固定效应模型。MD=0.25,95%CI:0.02-0.48,P < 0.05,证明运动干预是改善骨骼肌指数有效的干预措施。 2.4.3 身体功能 身体功能反映个体完成日常活动(如行走、起立、站立等)的能力,是评估肌少症严重程度的重要标志。身体功能的减退不仅包括下肢力量和步态的减弱,还涉及平衡能力、运动协调性等方面。 (1)起立-行走计时测试:共有7项随机对照试验报告了患有肌少症及其合并症人群进行运动干预前后起立-行走计时测试的结果[15-16,21,25](图8),I2=48%,P=0.07,故使用固定效应模型计算效应量大小,SMD=-0.75,95%CI(-1.09,-0.40),P < 0.000 1,运动干预能够改善起立-行走计时测试。 为了评估有效的运动方案对患有肌少症及其合并症的老年人起立-行走计时测试的影响(表3),亚组分析结果显示,在运动方式中,与有氧训练(MD=-1.74,95%CI:-3.71-0.24,P > 0.05)相比,全身振动训练(MD=-1.13,95%CI:-2.10至-0.16,P < 0.05)和抗阻联合有氧训练(MD=-2.22,95%CI:-2.97至-1.46,P < 0.001),对提高老年人起立-行走计时测试的时间均有显著促进效果;将运动频率分为>每周3次(MD=-1.95,95%CI:-2.81至-1.09,P < 0.001)和≤每周3次(MD=-1.13,95%CI:-2.10至-0.16,P < 0.05),均能产生效果;运动时间≥每天40 min(MD=-2.34,95%CI:-3.0至-1.67,P < 0.001)和<每天40 min(MD=-0.97,95%CI:-1.67至-0.27,P < 0.05),均能显著提高老年人起立-行走计时测试的时间。 (2)步速:共有13项随机对照试验报告了患有肌少症及其合并症人群进行运动干预前后步速测试的结果[11,13-16,18-19,23,25](图9),I2=62%,P=0.002,因此采用随机效应模型。由于步速测量的结局指标不同(3 m步速测试、6 m步速测试等),因此使用SMD计算效应量大小,SMD=0.48,95%CI:0.19-0.77,P < 0.05,说明运动干预能够提高步速。 为了评估有效的运动方案对患有肌少症及其合并症的老年人步速的影响(表3),亚组分析结果显示,在运动方式中,与抗阻训练(SMD=0.36,95%CI:-0.09-0.81,P > 0.05),全身振动训练(MD=0.02,95%CI:-0.04-0.09,P > 0.05),抗阻联合有氧训练相比(SMD=0.35,95%CI:-0.24-0.94,P > 0.05),抗阻联合平衡训练(SMD=1.19,95%CI:0.78-1.60,P < 0.001),对提高老年人步速有更"

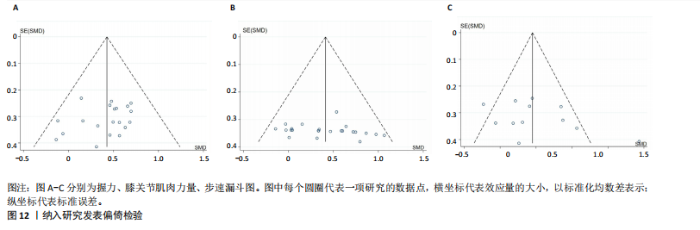
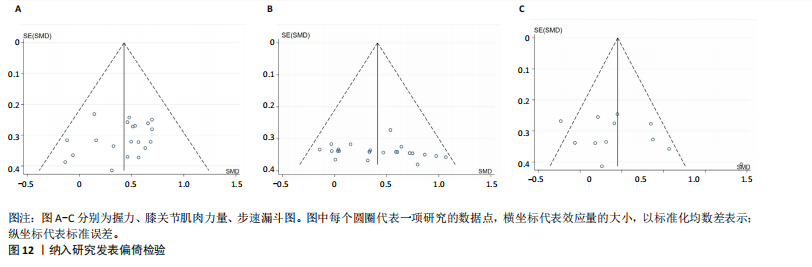
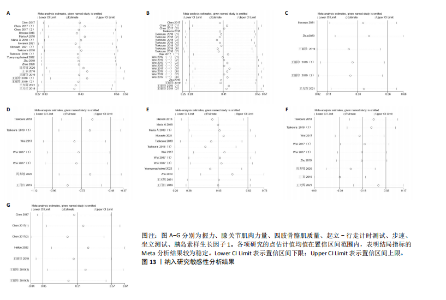
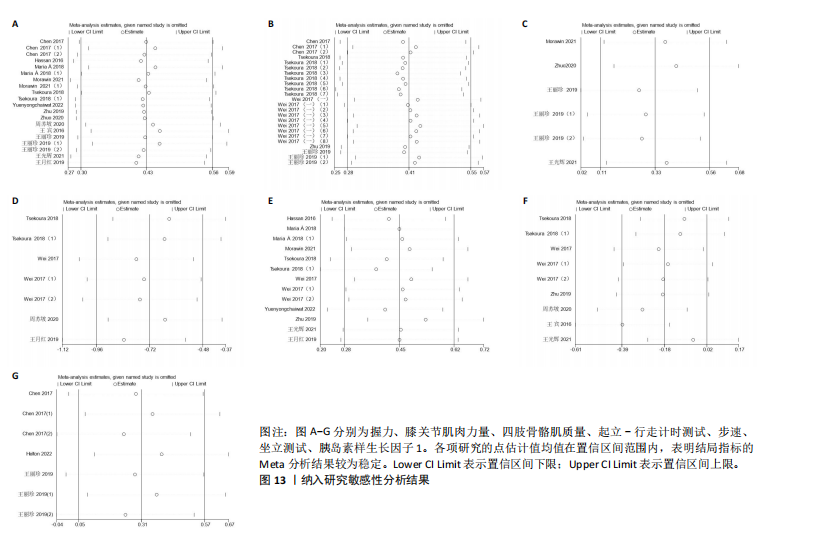
显著促进效果;而运动周期>12周(SMD=0.46,95%CI:0.12-0.79,P < 0.05)和≤12周(SMD=0.49,95%CI:0.10-0.88,P < 0.05)均能产生中等效应量的影响;在运动频率中,相比≤3次/周(SMD=0.22,95%CI:-0.00-0.45,P=0.05),> 3次/周(SMD=0.99,95%CI:0.44-1.54,P < 0.001)的改善呈现较大效应量;相比< 45 min/d(SMD=0.25,95%CI:0.00-0.49,P=0.05),运动时间≥45 min/d (SMD=0.76,95%CI:0.22-1.29,P < 0.05)的改善呈现较大效应量。 (3)坐立测试:9项随机对照试验报告了患有肌少症及其合并症人群进行运动干预前后坐立测试的结果[15-16,19,21,23-24](图10),I2=83%,P < 0.000 1,因此采用随机效应模型。由于坐立测试测量的结局指标不同(5次坐立测试,30 s坐立测试),因此使用SMD计算效应量大小,SMD=-0.27,95%CI:-0.76-0.23,P > 0.05,结果显示运动干预组与对照组坐立测试无显著性差异。 为评估有效的运动方案对患有肌少症及其合并症老年人坐立测试的影响(表3),亚组分析结果显示,在运动方式中,相比全身振动训练(MD=-0.48,95%CI:-1.61-0.64,P > 0.05),有氧训练(SMD=0.70,95%CI:0.32-1.08,P < 0.001)和抗阻联合平衡训练(MD:-3.52,95%CI:-4.92至-2.13,P < 0.001)对提高老年人坐立测试的时间有更显著的促进效果;而运动频率>每周3次(SMD=-0.49,95%CI:-1.77-0.78,P > 0.05)和≤每周3次(SMD=-0.16,95%CI:-0.68-0.36,P > 0.05)均与对照组相比均无显著性差异;运动时间≥60 min/d (SMD=0.27,95%CI:-0.51-1.06,P=0.05)和< 60 min/d (SMD=-0.43,95%CI:-0.99-0.12,P > 0.05),与对照组相比均无显著性差异。 2.5 次要结局指标 胰岛素样生长因子1通过促进肌肉合成代谢、抑制炎症老化及运动诱导表达,多靶点干预肌少症,因此作为次要结局指标纳入此次研究结果。 胰岛素样生长因子1:共有7项随机对照试验报告了患有肌少症及其合并症人群进行运动干预前后胰岛素样生长因子1水平[10,12,22](图11),I2=16%,P=0.31,因此采用固定效应模型。使用SMD计算效应量大小,SMD=0.30,95%CI(0.04,0.56),P < 0.05,与对照组相比,运动干预后胰岛素样生长因子1水平显著增高。 2.6 文献偏倚分析结果 采用漏斗图和Egger检验对纳入研究数量≥10篇的结局指标进行发表偏倚检测(图12)。结果显示,膝关节肌肉力量的漏斗图分布对称,Egger检验P=0.321,提示该指标不存在显著的发表偏倚。而握力和步速的漏斗图虽然对称性较差,提示可能存在发表偏倚,但Egger检验结果显示,膝关节肌肉力量和步速均未达到显著性水平(P=0.246,0.191),表明所纳入的研究未出现显著的发表偏倚。 采用剔除法对纳入研究≥5项的结局指标进行逐一剔除分析。敏感性分析结果显示,合并效应量的方向未发生改变,表明此次Meta分析的结果具有较好的稳健性(图13)。"
| [1] CHEN LK, WOO J, ASSANTACHAI P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020; 21(3):300-307.e2. [2] ZANKER J, SIM M, ANDERSON K, et al. Consensus guidelines for sarcopenia prevention, diagnosis and management in Australia and New Zealand. J Cachexia Sarcopenia Muscle. 2023;14(1):142-156. [3] 黄宏兴,史晓林,李盛华,等.肌少-骨质疏松症专家共识[J].中国骨质疏松杂志,2022,28(11):1561-1570. [4] NIELSON CM, SRIKANTH P, ORWOLL ES. Obesity and fracture in men and women: an epidemiologic perspective. J Bone Miner Res. 2012;27(1):1-10. [5] ORMSBEE MJ, PRADO CM, ILICH JZ, et al. Osteosarcopenic obesity: the role of bone, muscle, and fat on health. J Cachexia Sarcopenia Muscle. 2014;5(3):183-192. [6] KARAKOUSIS ND, BILIOU S, PYRGIOTI EE, et al. Frailty, sarcopenia and diabetic kidney disease: where do we stand? Int Urol Nephrol. 2023;55(5):1173-1181. [7] MONTERO-FERNÁNDEZ N, SERRA-REXACH JA. Role of exercise on sarcopenia in the elderly. Eur J Phys Rehabil Med. 2013;49(1):131-143. [8] HUANG CY, MAYER PK, WU MY, et al. The effect of Tai Chi in elderly individuals with sarcopenia and frailty: A systematic review and meta-analysis of randomized controlled trials. Ageing Res Rev. 2022;82:101747. [9] GREEN S, HIGGINS J. Cochrane handbook for systematic reviews of interventions, version 5.1.0. the cochrane collabo ration. The Cochrane Collaboration. 2011. [10] CHEN HT, CHUNG YC, CHEN YJ, et al. Effects of Different Types of Exercise on Body Composition, Muscle Strength, and IGF-1 in the Elderly with Sarcopenic Obesity. J Am Geriatr Soc. 2017;65(4):827-832. [11] HASSAN BH, HEWITT J, KEOGH JW, et al. Impact of resistance training on sarcopenia in nursing care facilities: A pilot study. Geriatr Nurs. 2016;37(2):116-121. [12] DE SÁ SOUZA H, DE MELO CM, PIOVEZAN RD, et al. Resistance Training Improves Sleep and Anti-Inflammatory Parameters in Sarcopenic Older Adults: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022;19(23):16322. [13] CEBRIÀ IIM, BALASCH-BERNAT M, TORTOSA-CHULIÁ M, et al. Effects of Resistance Training of Peripheral Muscles Versus Respiratory Muscles in Older Adults With Sarcopenia Who are Institutionalized: A Randomized Controlled Trial. J Aging Phys Act. 2018;26(4):637-646. [14] MORAWIN B, TYLUTKA A, CHMIELOWIEC J, et al. Circulating Mediators of Apoptosis and Inflammation in Aging; Physical Exercise Intervention. Int J Environ Res Public Health. 2021;18(6):3165. [15] TSEKOURA M, BILLIS E, TSEPIS E, et al. The Effects of Group and Home-Based Exercise Programs in Elderly with Sarcopenia: A Randomized Controlled Trial. J Clin Med. 2018;7(12):480. [16] WEI N, PANG MY, NG SS, et al. Optimal frequency/time combination of whole body vibration training for developing physical performance of people with sarcopenia: a randomized controlled trial. Clin Rehabil. 2017;31(10):1313-1321. [17] WEI N, PANG MY, NG SS, et al. Optimal frequency/time combination of whole-body vibration training for improving muscle size and strength of people with age-related muscle loss (sarcopenia): A randomized controlled trial. Geriatr Gerontol Int. 2017; 17(10):1412-1420. [18] YUENYONGCHAIWAT K, AKEKAWATCHAI C. Beneficial effects of walking-based home program for improving cardio-respiratory performance and physical activity in sarcopenic older people: a randomized controlled trial. Eur J Phys Rehabil Med. 2022;58(6):838-844. [19] ZHU L Y, CHAN R, KWOK T, et al. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing. 2019;48(2):220-228. [20] LI Z, CUI M, YU K, et al. Effects of nutrition supplementation and physical exercise on muscle mass, muscle strength and fat mass among sarcopenic elderly: a randomized controlled trial. Appl Physiol Nutr Metab. 2021;46(5):494-500. [21] 周苏坡,邹颖,孙小斐,等.八段锦预防老年肌少症人群跌倒的研究[J].体育科技,2020,41(6):27-28+30. [22] 王丽珍,郭颖彬,骆俊宏.居家运动训练对老年肥胖型肌少症的效果[J].中国康复理论与实践,2019,25(1):90-96. [23] 王光辉,蔡文玮,沈晓君,等.弹力带抗阻运动训练12周对社区老年肌少症患者肌力的影响[J].中国临床保健杂志, 2021,24(6):800-804. [24] 王宾,马士荣,胡莺.健身气功易筋经锻炼对骨骼肌减少症患者康复效果的影响[J].中国老年学杂志,2016,36(4):898-899. [25] 王月红,蔺建宇,孙超,等.有氧运动计划记录单在老年肌少症应用的效果评价[J].中国病案,2019,20(12):110-112. [26] MUÑOZ-REDONDO E, MORGADO-PÉREZ A, PÉREZ-SÁEZ MJ, et al. New perspectives on frailty in light of the Global Leadership Initiative on Malnutrition, the Global Leadership Initiative on Sarcopenia, and the WHO’s concept of intrinsic capacity: A narrative review. Maturitas. 2023;177: 107799. [27] SHEN Y, SHI Q, NONG K, et al. Exercise for sarcopenia in older people: A systematic review and network meta-analysis. J Cachexia Sarcopenia Muscle. 2023;14(3): 1199-1211. [28] VALDÉS-BADILLA P, GUZMÁN-MUÑOZ E, HERNANDEZ-MARTINEZ J, et al. Effectiveness of elastic band training and group-based dance on physical-functional performance in older women with sarcopenia: a pilot study. BMC Public Health. 2023;23(1):2113. [29] 温鹏天,张瑞丽,胡文清,等.不同运动干预方式对老年人肌少症改善效果的Meta分析[J].中国康复理论与实践,2021, 27(11):1291-1298. [30] KENNIS E, VERSCHUEREN SM, BOGAERTS A, et al. Long-term impact of strength training on muscle strength characteristics in older adults. Arch Phys Med Rehabil. 2013;94(11): 2054-2060. [31] MARZUCA-NASSR GN, ALEGRíA-MOLINA A, SANMARTíN-CALíSTO Y, et al. Muscle Mass and Strength Gains Following Resistance Exercise Training in Older Adults 65-75 Years and Older Adults Above 85 Years. Int J Sport Nutr Exerc Metab. 2024;34(1):11-19. [32] MCLEOD JC, CURRIER BS, LOWISZ CV, et al. The influence of resistance exercise training prescription variables on skeletal muscle mass, strength, and physical function in healthy adults: An umbrella review. J Sport Health Sci. 2024;13(1):47-60. [33] HOU L, LEI Y, LI X, et al. Effect of Protein Supplementation Combined with Resistance Training on Muscle Mass, Strength and Function in the Elderly: A Systematic Review and Meta-Analysis. J Nutr Health Aging. 2019;23(5):451-458. [34] NEGM AM, LEE J, HAMIDIAN R, et al. Management of Sarcopenia: A Network Meta-Analysis of Randomized Controlled Trials. J Am Med Dir Assoc. 2022;23(5): 707-714. [35] DENISON HJ, COOPER C, SAYER AA, et al. Prevention and optimal management of sarcopenia: a review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin Int Aging. 2015;10:859-869. [36] BEAUDART C, DAWSON A, SHAW SC, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int. 2017; 28(6):1817-1833. [37] ESCRICHE-ESCUDER A, FUENTES-ABOLAFIO IJ, ROLDÁN-JIMÉNEZ C, et al. Effects of exercise on muscle mass, strength, and physical performance in older adults with sarcopenia: A systematic review and meta-analysis according to the EWGSOP criteria. Exp Gerontol. 2021;151:111420. [38] CRUZ-JENTOFT AJ, BAHAT G, BAUER J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48(1):16-31. [39] RUNGE M, REHFELD G, RESNICEK E. Balance training and exercise in geriatric patients. Musculoskelet Neuronal Interact. 2000; 1(1):61-65. [40] CHEN N, HE X, FENG Y, et al. Effects of resistance training in healthy older people with sarcopenia: a systematic review and meta-analysis of randomized controlled trials. Eur Rev Aging Phys Act. 2021;18(1): 23. [41] FILIPOVIĆ TN, LAZOVIĆ MP, BACKOVIĆ AN, et al. A 12-week exercise program improves functional status in postmenopausal osteoporotic women: randomized controlled study. Eur J Phys Rehabil Med. 2021;57(1):120-130. [42] ASCENZI F, BARBERI L, DOBROWOLNY G, et al. Effects of IGF-1 isoforms on muscle growth and sarcopenia. Aging Cell. 2019;18(3):e12954. [43] EKLUND E, HELLBERG A, BERGLUND B, et al. IGF-I and IGFBP-1 in Relation to Body Composition and Physical Performance in Female Olympic Athletes. Front Endocrinol. 2021;12:708421. |
| [1] | Hou Chaowen, Li Zhaojin, Kong Jianda, Zhang Shuli. Main physiological changes in skeletal muscle aging and the multimechanism regulatory role of exercise [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1464-1475. |
| [2] | Sun Yaotian, Xu Kai, Wang Peiyun. Potential mechanisms by which exercise regulates iron metabolism in immune inflammatory diseases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1486-1498. |
| [3] | Liu Yu, Lei Senlin, Zhou Jintao, Liu Hui, Li Xianhui. Mechanisms by which aerobic and resistance exercises improve obesity-related cognitive impairment [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1171-1183. |
| [4] | Wen Fan, Xiang Yang, Zhu Huan, Tuo Yanfang, Li Feng. Exercise improves microvascular function in patients with type 2 diabetes [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1225-1235. |
| [5] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [6] | Yang Zhijie, Zhao Rui, Yang Haolin, Li Xiaoyun, Li Yangbo, Huang Jiachun, Lin Yanping, Wan Lei, HuangHongxing. Postmenopausal osteoporosis: predictive values of muscle mass, grip strength, and appendicular skeletal muscle index [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1073-1080. |
| [7] | Zhou Jian, Zhang Tao, Zhou Weili, Zhao Xingcheng, Wang Jun, Shen Jie, Qian Li, Lu Ming. Effects of resistance training on quadriceps mass and knee joint function in patients with osteoporosis and sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1081-1088. |
| [8] | Jiang Yang, Peng Hao, Song Yanping, Yao Na, Song Yueyu, Yin Xingxiao, Li Yanqi, Chen Qigang. Isometric exercise reduces resting blood pressure: a meta-analysis of moderating factors and dose effects [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 975-986. |
| [9] | Li Hanyue, Li Yini, Xiang Linmei, Li Sen. Effects of resistance exercise therapy on pain and function in patients with cervical spondylotic radiculopathy: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 987-996. |
| [10] | Dong Chao, Zhao Mohan, Liu Yunan, Yang Zeli, Chen Leqin, Wang Lanfang. Effects of magnetic nano-drug carriers on exercise-induced muscle injury and inflammatory response in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 345-353. |
| [11] | Sun Yundi, Cheng Lulu, Wan Haili, Chang Ying, Xiong Wenjuan, Xia Yuan. Effect of neuromuscular exercise for knee osteoarthritis pain and function: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1945-1952. |
| [12] | Wang Qiuyue, Jin Pan, Pu Rui . Exercise intervention and the role of pyroptosis in osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1667-1675. |
| [13] | Wang Yida, Liu Jun, Wang Xiaoling, Wang Liyan, Yang Chengru, Zhang Xuexiao. Effects of wearable electronic device-based interventions on physical activity and sedentary behavior in healthy adolescents: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1693-1704. |
| [14] | Zhang Zixian, Xu Youliang, Wu Shaokui, Wang Xiangying. Effects of blood flow restriction training combined with resistance training on muscle indicators in college athletes: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1705-1713. |
| [15] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||