Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (1): 58-67.doi: 10.12307/2025.576
Previous Articles Next Articles
Therapeutic effects of adipose-derived mesenchymal stem cells and their exosomes on dexamethasone-induced sarcopenia in mice
Yuan Weiyuan1, 2, Lei Qinhui3, Li Xiuqi3, Lu Tiezhu3, Fu Ziwen4, 5, Liang Zhili5, Ji Shaoyang6, Li Yijia1, 2, Ren Yu3
- 1CiMSC Therapeutics Co., Ltd., Shanghai 200233, China; 2Baoshan Institute of Synthetic Biology and Translational Research, Shanghai 200233, China; 3Mitoch Therapeutics Co., Ltd., Beijing 101319, China; 4Miymi Biotech Co., Ltd., Zhangjiagang 215628, Jiangsu Province, China; 5AdvanCell Biotech Co., Ltd., Zhuhai 519060, Guangdong Province, China; 6Institute of Process Engineering, Chinese Academy of Sciences, Beijing 100190, China
-
Received:2024-11-20Accepted:2025-01-24Online:2026-01-08Published:2025-06-18 -
Contact:Li Yijia, PhD, Associate researcher, CiMSC Therapeutics Co., Ltd., Shanghai 200233, China; Baoshan Institute of Synthetic Biology and Translational Research, Shanghai 200233, China; Co-corresponding author: Ren Yu, PhD, Mitoch Therapeutics Co., Ltd., Beijing 101319, China -
About author:Yuan Weiyuan, MS, CiMSC Therapeutics Co., Ltd., Shanghai 200233, China; Baoshan Institute of Synthetic Biology and Translational Research, Shanghai 200233, China. Lei Qinhui, MS, Mitoch Therapeutics Co., Ltd., Beijing 101319, China. Yuan Weiyuan and Lei Qinhui contributed equally to this work.
CLC Number:
Cite this article
Yuan Weiyuan, Lei Qinhui, Li Xiuqi, Lu Tiezhu, Fu Ziwen, Liang Zhili, Ji Shaoyang, Li Yijia, Ren Yu . Therapeutic effects of adipose-derived mesenchymal stem cells and their exosomes on dexamethasone-induced sarcopenia in mice[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 58-67.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

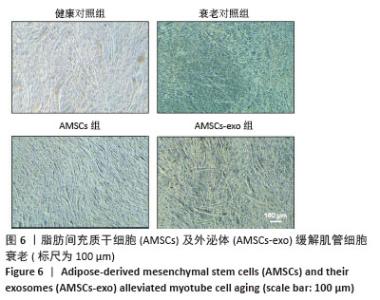
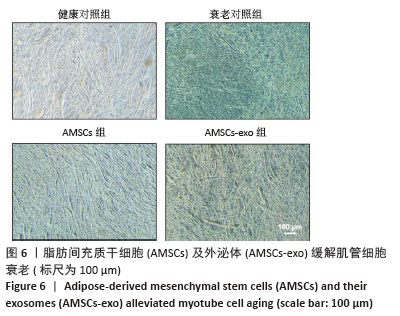
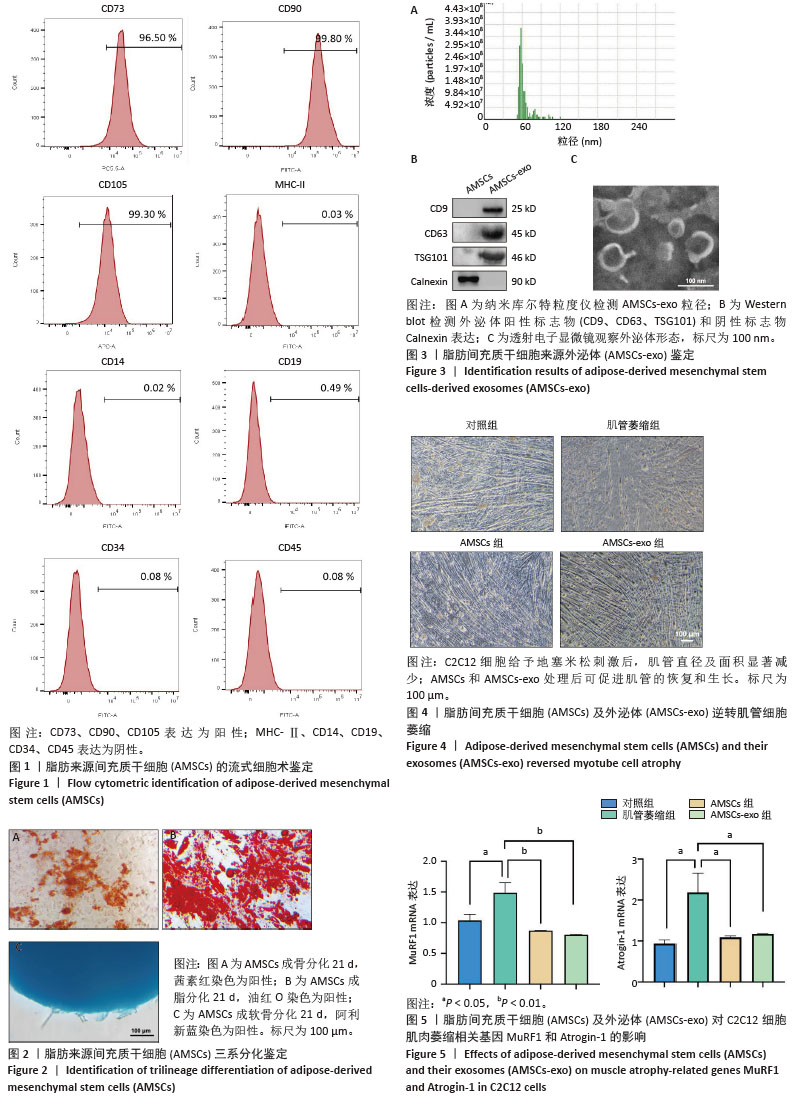
2.1 AMSCs鉴定结果 流式细胞术结果显示,AMSCs阳性标志物CD73、CD90、CD105的阳性百分比分别为96.50%,99.80%,99.30%,阴性指标MHC-Ⅱ、CD14、CD19、CD34、CD45的阳性百分比分别为0.03%,0.02%,0.49%,0.08%,0.08%,以上数据表明分离培养的AMSCs纯度达到95%以上,状态良好,见图1。AMSCs三系分化结果显示,经茜素红染色可见红色钙结节,表明具有成骨分化能力;经油红O染色可见红色脂滴,表明具有成脂分化能力;经阿利新蓝染色可见浅蓝色软骨,表明具有成软骨分化能力,见图2。以上结果表明,分离培养的AMSCs具有良好的分化潜能。 2.2 AMSCs-exo鉴定结果 纳米库尔特粒度仪检测结果显示,AMSCs-exo粒径分布为50-100 nm,平均粒径为60 nm,且呈单峰,提示所获得的外泌体纯度较高。Western blot结果显示,与AMSCs相比,分离制备的AMSCs-exo高表达CD9、CD63、TSG101,低表达Calnexin,符合外泌体的表征验证。透射电子显微镜观察到AMSCs-exo呈现不聚团的具有清晰膜结构的茶托状或杯状结构,边缘清晰。以上结果表明,已成功分离纯化获得高质量的外泌体,见图3。 2.3 AMSCs和AMSCs-exo可逆转地塞米松诱导的体外肌肉细胞萎缩 C2C12细胞使用地塞米松刺激后,肌管直径及面积显著减少,提示体外肌管萎缩模型构建成功。使用AMSCs和AMSCs-exo进行处理后,可促进肌管的恢复和生长,见图4。与对照组相比,肌管萎缩组肌肉萎缩相关基因MuRF1和Atrogin-1 mRNA表达显著升高(P < 0.05,P < 0.05),AMSCs和AMSCs-exo处理后可显著抑制MuRF1和Atrogin-1 mRNA表达(P < 0.01,P < 0.01,P < 0.05,P < 0.05),见图5。以上数据表明AMSCs及AMSCs-exo均可缓解地塞米松诱导的肌管细胞萎缩,抑制肌肉萎缩相关基因表达。 "
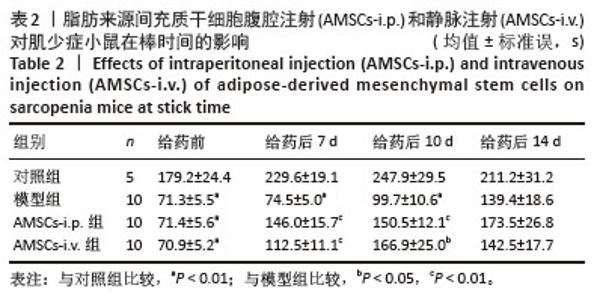
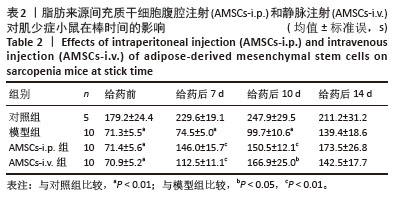
2.5 实验动物数量分析 实验选用C57BL/6J小鼠35只,造模及给药后无死亡,全部进入结果分析。 2.6 AMSCs腹腔和静脉给药可增加肌少症小鼠肌肉耐力 通过转棒疲劳实验评估肌少症小鼠药物治疗后的肌肉耐力行为变化。在给药前,与对照组相比,模型组、AMSCs-i.p.组和AMSCs-i.v.组小鼠的在棒时间均显著降低(P < 0.01,P < 0.01,P < 0.01),分别为(71.3±5.5) s,(71.4±5.6) s,(70.9±5.2) s,提示地塞米松诱导的小鼠肌少症模型构建成功。给药后7 d, 与对照组相比,模型组小鼠的在棒时间为(74.5±5.0) s,差异有显著性意义(P < 0.01),提示肌少症小鼠肌肉耐力下降。与模型组相比,AMSCs-i.p.组和AMSCs-i.v.组小鼠的在棒时间显著增加(P < 0.01,P < 0.01),分别为(146.0±15.7) s,(112.5±11.1) s;给药后10 d,与模型组相比,AMSCs-i.p.组和AMSCs-i.v.组 小鼠的在棒时间也显著增加(P < 0.01,P < 0.05),分别为(150.5±12.1) s,(166.9±25.0) s;给药后14 d,AMSCs-i.p.组和AMSCs-i.v.组小鼠的在棒时间[(173.5±26.8) s,(142.5±17.7) s]虽高于模型组,但无明显差异(P > 0.05),见表2。 "

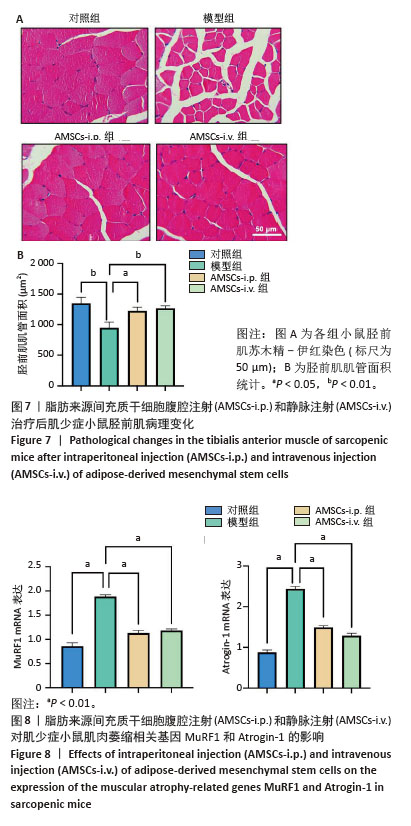
2.7 AMSCs腹腔和静脉给药促进肌少症小鼠肌肉恢复 苏木精-伊红染色结果显示,与对照组相比,模型组胫前肌肌管面积显著降低(P < 0.01);与模型组相比,AMSCs-i.p.组和AMSCs-i.v.组给药后均可显著增加胫前肌肌管面积(P < 0.05,P < 0.01),这与增强肌少症小鼠的肌肉耐力直接相关,见图7。与对照组相比,模型组胫前肌肌肉萎缩相关基因MuRF1和Atrogin-1 mRNA表达显著升高(P < 0.01,P < 0.01),AMSCs-i.p.组和AMSCs-i.v.组给药后可显著抑制MuRF1和Atrogin-1 mRNA表达(P < 0.01,P < 0.01,P < 0.01,P < 0.01),见图8。以上结果表明,AMSCs-i.p.和AMSCs-i.v.给药后可显著促进肌少小鼠的肌肉恢复和生长,抑制肌肉萎缩相关基因表达。"
| [1] CRUZ-JENTOFT AJ, BAEYENS JP, BAUER JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412-423. [2] Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 Suppl): 1121-1235. [3] CHEN LK, WOO J, ASSANTACHAI P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300-307.e2. [4] 中华医学会骨质疏松和骨矿盐疾病分会. 肌少症共识[J].中华骨质疏松和骨矿盐疾病杂志,2016,9(3):215-227. [5] 崔华,王朝晖,吴剑卿,等.老年人肌少症防控干预中国专家共识(2023)[J].中华老年医学杂志,2023,42(2):144-153. [6] ANKER SD, MORLEY JE, VON HAEHLING S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle. 2016;7(5):512-514. [7] MANKHONG S, KIM S, MOON S, et al. Experimental Models of Sarcopenia: Bridging Molecular Mechanism and Therapeutic Strategy. Cells. 2020;9(6):1385. [8] NAJM A, MOLDOVEANU ET, NICULESCU AG, et al. Advancements in Drug Delivery Systems for the Treatment of Sarcopenia: An Updated Overview. Int J Mol Sci. 2024;25(19):10766. [9] FLACK KD, DAVY KP, HULVER MW, et al. Aging, resistance training, and diabetes prevention. J Aging Res. 2010;2011:127315. [10] PIAO L, HUANG Z, INOUE A, et al. Human umbilical cord-derived mesenchymal stromal cells ameliorate aging-associated skeletal muscle atrophy and dysfunction by modulating apoptosis and mitochondrial damage in SAMP10 mice. Stem Cell Res Ther. 2022; 13(1):226. [11] SONG J, LIU J, CUI C, et al. Mesenchymal stromal cells ameliorate diabetes-induced muscle atrophy through exosomes by enhancing AMPK/ULK1-mediated autophagy. J Cachexia Sarcopenia Muscle. 2023;14(2):915-929. [12] MAHINDRAN E, LAW JX, NG MH, et al. Mesenchymal Stem Cell Transplantation for the Treatment of Age-Related Musculoskeletal Frailty. Int J Mol Sci. 2021;22(19):10542. [13] KUROSAWA T, IKEMOTO-UEZUMI M, YOSHIMOTO Y, et al. Tissue-specific functions of MSCs are linked to homeostatic muscle maintenance and alter with aging. Aging Cell. 2024;23(11):e14299. [14] WOSCZYNA MN, KONISHI CT, PEREZ CARBAJAL EE, et al. Mesenchymal Stromal Cells Are Required for Regeneration and Homeostatic Maintenance of Skeletal Muscle. Cell Rep. 2019;27(7):2029-2035.e5. [15] ZHU Y, HUANG C, ZHENG L, et al. Safety and efficacy of umbilical cord tissue-derived mesenchymal stem cells in the treatment of patients with aging frailty: a phase I/II randomized, double-blind, placebo-controlled study. Stem Cell Res Ther. 2024;15(1):122. [16] YOUSEFI K, RAMDAS KN, RUIZ JG, et al. The Design and Rationale of a Phase 2b, Randomized, Double-Blinded, and Placebo-Controlled Trial to Evaluate the Safety and Efficacy of Lomecel-B in Older Adults with Frailty. J Frailty Aging. 2022;11(2):214-223. [17] NGUYEN NT, PHAN HT, LE PM, et al. Safety and efficacy of autologous adipose tissue-derived stem cell transplantation in aging-related low-grade inflammation patients: a single-group, open-label, phase I clinical trial. Trials. 2024;25(1):309. [18] GOLPANIAN S, DIFEDE DL, KHAN A, et al. Allogeneic Human Mesenchymal Stem Cell Infusions for Aging Frailty. J Gerontol A Biol Sci Med Sci. 2017;72(11):1505-1512. [19] TOMPKINS BA, DIFEDE DL, KHAN A, et al. Allogeneic Mesenchymal Stem Cells Ameliorate Aging Frailty: A Phase II Randomized, Double-Blind, Placebo-Controlled Clinical Trial. J Gerontol A Biol Sci Med Sci. 2017;72(11):1513-1522. [20] SHEHATA AS, AL-GHONEMY NM, AHMED SM, et al. Effect of mesenchymal stem cells on induced skeletal muscle chemodenervation atrophy in adult male albino rats. Int J Biochem Cell Biol. 2017;85: 135-148. [21] LI TS, SHI H, WANG L, et al. Effect of Bone Marrow Mesenchymal Stem Cells on Satellite Cell Proliferation and Apoptosis in Immobilization-Induced Muscle Atrophy in Rats. Med Sci Monit. 2016;22:4651-4660. [22] TAKEGAKI J, SASE K, KONO Y, et al. Intramuscular injection of mesenchymal stem cells augments basal muscle protein synthesis after bouts of resistance exercise in male mice. Physiol Rep. 2024;12(7): e15991. [23] ARCHACKA K, GRABOWSKA I, MIERZEJEWSKI B, et al. Hypoxia preconditioned bone marrow-derived mesenchymal stromal/stem cells enhance myoblast fusion and skeletal muscle regeneration. Stem Cell Res Ther. 2021;12(1):448. [24] WANG QQ, JING XM, BI YZ, et al. Human Umbilical Cord Wharton’s Jelly Derived Mesenchymal Stromal Cells May Attenuate Sarcopenia in Aged Mice Induced by Hindlimb Suspension. Med Sci Monit. 2018;24: 9272-9281. [25] WANG C, ZHAO B, ZHAI J, et al. Clinical-grade human umbilical cord-derived mesenchymal stem cells improved skeletal muscle dysfunction in age-associated sarcopenia mice. Cell Death Dis. 2023;14(5):321. [26] 陈三,杨润泽,吴家媛.预处理来源外泌体在细胞增殖分化及凋亡中的作用[J].中国组织工程研究,2023,27(19):3029-3039. [27] MAHINDRAN E, WAN KAMARUL ZAMAN WS, AHMAD AMIN NOORDIN KB, et al. Mesenchymal Stem Cell-Derived Extracellular Vesicles: Hype or Hope for Skeletal Muscle Anti-Frailty. Int J Mol Sci. 2023;24(9):7833. [28] LO SICCO C, REVERBERI D, BALBI C, et al. Mesenchymal Stem Cell-Derived Extracellular Vesicles as Mediators of Anti-Inflammatory Effects: Endorsement of Macrophage Polarization. Stem Cells Transl Med. 2017;6(3):1018-1028. [29] FIGLIOLINI F, RANGHINO A, GRANGE C, et al. Extracellular Vesicles From Adipose Stem Cells Prevent Muscle Damage and Inflammation in a Mouse Model of Hind Limb Ischemia: Role of Neuregulin-1. Arterioscler Thromb Vasc Biol. 2020;40(1):239-254. [30] WANG C, SONG W, CHEN B, et al. Exosomes Isolated From Adipose-Derived Stem Cells: A New Cell-Free Approach to Prevent the Muscle Degeneration Associated With Torn Rotator Cuffs. Am J Sports Med. 2019;47(13):3247-3255. [31] NAKAMURA Y, MIYAKI S, ISHITOBI H, et al. Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle regeneration. FEBS Lett. 2015;589(11): 1257-1265. [32] LI Z, LIU C, LI S, et al. BMSC-Derived Exosomes Inhibit Dexamethasone-Induced Muscle Atrophy via the miR-486-5p/FoxO1 Axis. Front Endocrinol (Lausanne). 2021;12:681267. [33] SANZ-ROS J, ROMERO-GARCÍA N, MAS-BARGUES C, et al. Small extracellular vesicles from young adipose-derived stem cells prevent frailty, improve health span, and decrease epigenetic age in old mice. Sci Adv. 2022;8(42):eabq2226. [34] DAI H, ZHENG W, LUO J, et al. Inhibiting uptake of extracellular vesicles derived from senescent bone marrow mesenchymal stem cells by muscle satellite cells attenuates sarcopenia. J Orthop Translat. 2022;35:23-36. [35] KARTIKA RW, SIDHARTA VM, DJUARTINA T, et al. New Insight in Using of Mesenchyme Stem Cell Conditioning Medium for the Impaired Muscle related Biomarkers: In vivo Study with Rat Model. Ann Afr Med. 2024;23(4):674-679. [36] WANG L, JIAO XF, WU C, et al. Trimetazidine attenuates dexamethasone-induced muscle atrophy via inhibiting NLRP3/GSDMD pathway-mediated pyroptosis. Cell Death Discov. 2021;7(1):251. [37] CRUZ-JENTOFT AJ, LANDI F, TOPINKOVÁ E, et al. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010;13(1):1-7. [38] GE J, ZENG J, MA H, et al. A New Index Based on Serum Creatinine and Cystatin C Can Predict the Risks of Sarcopenia, Falls and Fractures in Old Patients with Low Bone Mineral Density. Nutrients. 2022;14(23):5020. [39] BURGEL CF, CARVALHO BZO, MILESI BM, et al. SARC-CalF using calf circumference adjusted for BMI predicts 6-mo readmission and mortality in hospitalized patients: a secondary analysis of a cohort study. Am J Clin Nutr. 2025;121(1):151-157. [40] HEN LK, LEE WJ, PENG LN, et al. Recent Advances in Sarcopenia Research in Asia: 2016 Update From the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2016;17(8):767.e1-7. [41] BOWEN TS, SCHULER G, ADAMS V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachexia Sarcopenia Muscle. 2015;6(3):197-207. [42] ZHIDU S, YING T, RUI J, et al. Translational potential of mesenchymal stem cells in regenerative therapies for human diseases: challenges and opportunities. Stem Cell Res Ther. 2024;15(1):266. [43] HOANG DM, PHAM PT, BACH TQ, et al. Stem cell-based therapy for human diseases. Signal Transduct Target Ther. 2022;7(1):272. [44] DOMINICI M, LE BLANC K, MUELLER I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315-317. [45] WIDJAJA G, JALIL AT, BUDI HS, et al. Mesenchymal stromal/stem cells and their exosomes application in the treatment of intervertebral disc disease: A promising frontier. Int Immunopharmacol. 2022; 105:108537. [46] CUDKOWICZ ME, LINDBORG SR, GOYAL NA, et al. A randomized placebo-controlled phase 3 study of mesenchymal stem cells induced to secrete high levels of neurotrophic factors in amyotrophic lateral sclerosis. Muscle Nerve. 2022;65(3):291-302. [47] WELSH JA, GOBERDHAN DCI, O’DRISCOLL L, et al. Minimal information for studies of extracellular vesicles (MISEV2023): From basic to advanced approaches. J Extracell Vesicles. 2024;13(2):e12404. [48] MA H, JING Y, ZENG J, et al. Human umbilical cord mesenchymal stem cell-derived exosomes ameliorate muscle atrophy via the miR-132-3p/FoxO3 axis. J Orthop Translat. 2024;49:23-36. [49] WIAFE B, KADAM R, METCALFE PD. Intraperitoneal administration of mesenchymal stem cells is effective at mitigating detrusor deterioration after pBOO. Am J Physiol Renal Physiol. 2020;318(3): F549-F556. [50] BODINE SC, BAEHR LM. Skeletal muscle atrophy and the E3 ubiquitin ligases MuRF1 and MAFbx/atrogin-1. Am J Physiol Endocrinol Metab. 2014;307(6):E469-484. |
| [1] | Yang Lixia, Diao Liqin, Li Hua, Feng Yachan, Liu Xin, Yu Yuexin, Dou Xixi, Gu Huifeng, Xu Lanju. Regulatory mechanism of recombinant type III humanized collagen protein improving photoaging skin in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1988-2000. |
| [2] | Liu Huan, Zeng Shaopeng, Chen Jun, He Linqian, Yang Ying, Zhang Jing. Aging-related dysregulation of glucose metabolism: crossroads of cancer and neurodegenerative diseases [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1527-1538. |
| [3] | Hou Chaowen, Li Zhaojin, Kong Jianda, Zhang Shuli. Main physiological changes in skeletal muscle aging and the multimechanism regulatory role of exercise [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1464-1475. |
| [4] | Zhou Jian, Zhang Tao, Zhou Weili, Zhao Xingcheng, Wang Jun, Shen Jie, Qian Li, Lu Ming. Effects of resistance training on quadriceps mass and knee joint function in patients with osteoporosis and sarcopenia [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1081-1088. |
| [5] | Peng Tuanhui, Song Hongming, Yang Ling, Ding Xiaoge, Meng Pengjun. Effects of long-term endurance exercise on kl/FGF23 axis and calcium-phosphorus metabolism in naturally aging mice [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1089-1095. |
| [6] | Li Guangzheng, Li Wei, Zhang Bochun, Ding Haoqin, Zhou Zhongqi, Li Gang, Liang Xuezhen. A prediction model for sarcopenia in postmenopausal women: information analysis based on the China Health and Retirement Longitudinal Study database [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 849-857. |
| [7] | Sun Jiahe, Shi Jipeng, Zhu Tianrui, Quan Helong, Xu Hongqi. Effect of exercise intervention in elderly individuals with sarcopenia and its comorbidities: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 997-1007. |
| [8] | He Qiwang, , , Chen Bo, Liang Fuchao, Kang Zewei, Zhou Yuan, Ji Anxu, Tang Xialin, . Relationship between Alzheimer’s disease and sarcopenia and body mass index: analysis of GWAS datasets for European populations [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(4): 1036-1046. |
| [9] | Zhou Feng, Fu Pengfei, Qian Yufan, Xu Pingcheng, Guo Jiongjiong, Zhang Lei. Correlation between spinal sagittal imbalance and knee joint parameters detected by whole-body EOS imaging [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(3): 596-603. |
| [10] | Zhang Qian, Wang Fuxia, Wang Wen, Zhang Kun. Characteristic analysis of nanogel composite system and its application strategies in visualization of diagnostic imaging and therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 480-488. |
| [11] | Tan Fengyi, Xie Jiamin, Pan Zhenfeng, Zhang Xinxu, Zheng Zetai, Zeng Zhiying, Zhou Yanfang. Effect and mechanism of collagen combined with microneedles in treatment of skin photoaging [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(2): 451-458. |
| [12] | Yu Manya, Cui Xing. Contribution and interaction of various cells in bone marrow microenvironment to exosomal circular RNA associated with multiple myeloma bone disease [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 101-110. |
| [13] | Wang Yaping, Gao Tianyun, Wang Bin. Senescence of human bone marrow mesenchymal stromal cells with increasing age is not dependent on the mediation of endogenous retroviruses [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 10-20. |
| [14] | Zuo Na, Tang Qi, Yu Meng, Tao Kai. Effect of miR-196b-5p in adipose-derived stem cell exosomes on burn wound healing in rats [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 43-49. |
| [15] | Zhang Zhaowei, Chen Ouzile, Bai Mingru, Wang Chenglin. Therapeutic potential of bioactive substances secreted by dental mesenchymal stem cells for bone repair [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(1): 163-174. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||