Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (22): 3509-3516.doi: 10.12307/2024.488
Previous Articles Next Articles
Repair of infected osteochondral defect with sustained release vancomycin three-dimensional scaffold in rabbits
Li Xingyu1, Zhou Jie1, Li Shasha1, Zhang Tianxi1, Guo Guoning1, Yu Anyong1, Deng Jiang2, Ye Peng1
- 1Emergency Department of Affiliated Hospital of Zunyi Medical University (First Aid Trauma Ward), Zunyi 563003, Guizhou Province, China; 2Department of Orthopedics, Zunyi First People’s Hospital, Zunyi 563003, Guizhou Province, China
-
Received:2023-04-04Accepted:2023-09-28Online:2024-08-08Published:2024-01-20 -
Contact:Ye Peng, MD, Associate chief physician, Emergency Department of Affiliated Hospital of Zunyi Medical University (First Aid Trauma Ward), Zunyi 563003, Guizhou Province, China -
About author:Li Xingyu, Master, Emergency Department of Affiliated Hospital of Zunyi Medical University (First Aid Trauma Ward), Zunyi 563003, Guizhou Province, China -
Supported by:National Natural Science Foundation of China (Regional Science Foundation), No. H0606 (to DJ); Guizhou Science and Technology Plan Project, No. [2021]074 (to YP); Guizhou Science and Technology Plan Project, No. [2022]034 (to GGN); Outstanding Young Talents Training Program of Affiliated Hospital of Zunyi Medical University, No. RC220220911 (to YP)
CLC Number:
Cite this article
Li Xingyu, Zhou Jie, Li Shasha, Zhang Tianxi, Guo Guoning, Yu Anyong, Deng Jiang, Ye Peng. Repair of infected osteochondral defect with sustained release vancomycin three-dimensional scaffold in rabbits[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(22): 3509-3516.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
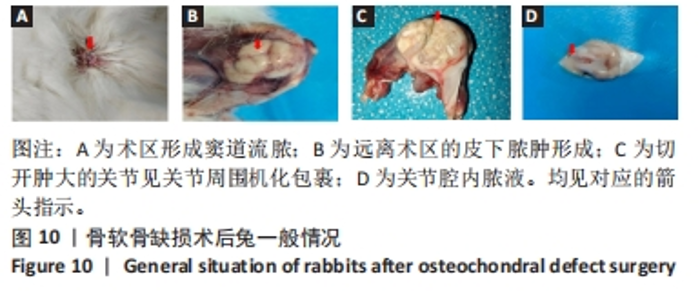
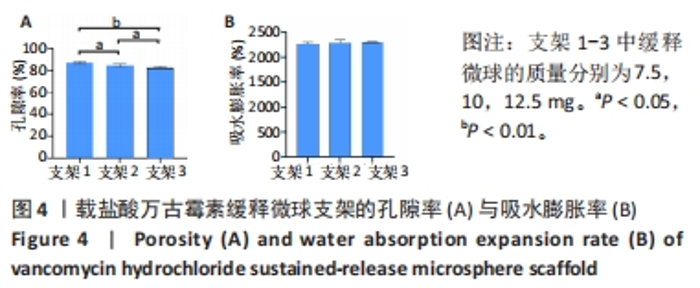
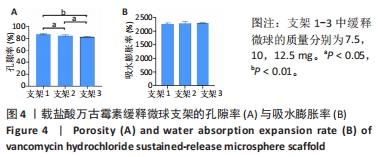
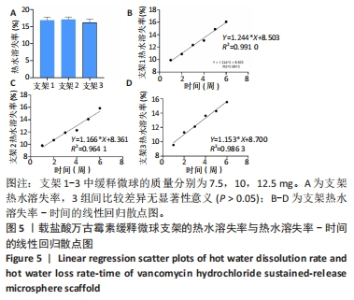
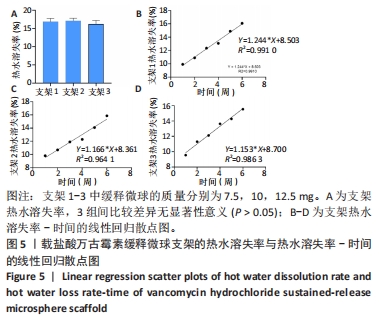
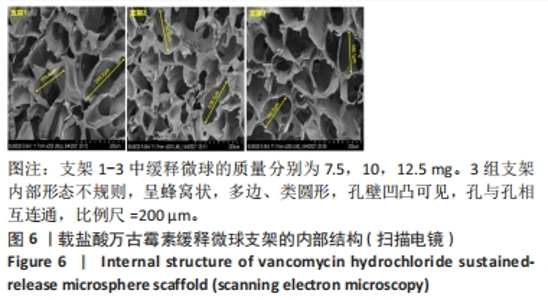
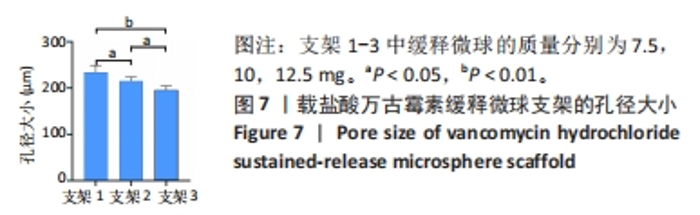
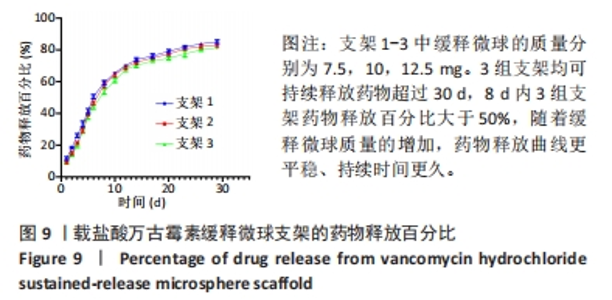
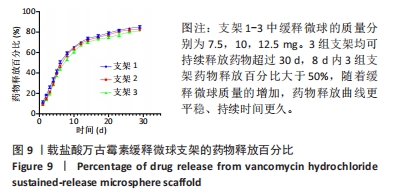
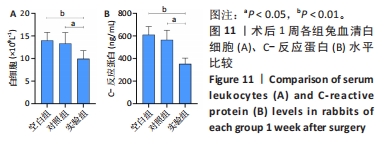
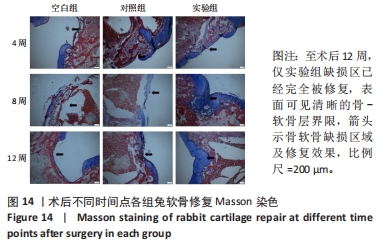
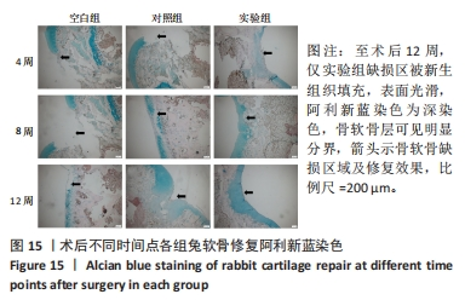
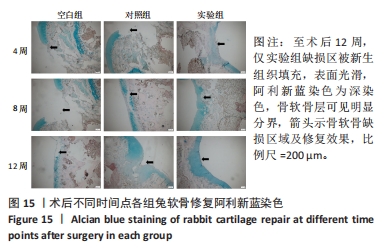
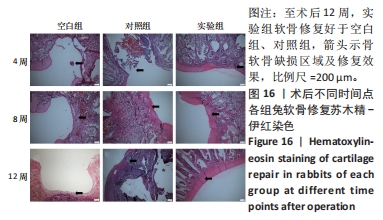
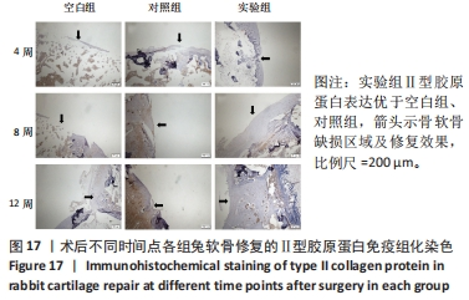
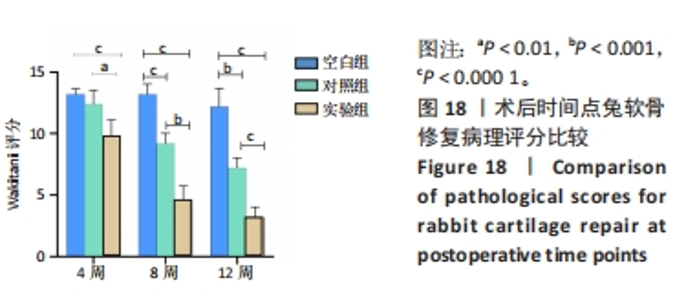
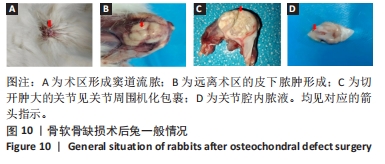
尽管增加载药微球的量可以提高支架的药物释放效率,但是太多的载药微球也会导致支架的孔隙率和孔径减小,只有加入适当的载药微球才能为细胞的生长、增殖、分化等提供更好的空间和环境。综合以上结果,在支架中加入10 mg VANCO缓释微球最符合细胞生长需求,故选择支架2完成动物实验部分。 2.3 兔软骨缺损修复效果 2.3.1 实验动物数量分析 45只兔全部进入结果分析。 2.3.2 术后兔一般情况 3组兔术后第1-3天精神饮食差,饮食自如。在术后1个月内,空白组有12只兔术区肿胀,红肿面积大,周围组织坏死,见窦道形成,并伴随大量脓液的排出周围形成窦道并流脓;对照组有10只兔术区红肿明显,周围形成窦道并流脓;实验组有2只兔膝关节周围形成窦道并流脓。1个月以后,空白组、对照组兔术后术区及关节处肿胀明显,关节畸形,步态不稳,活动明显受限,切开肿大的关节见机化包裹,暴露关节腔见黄色脓性关节液,部分兔在远离术区的颈背部可见皮下脓肿;实验组兔术后关节活动及饮食自如,部分兔关节活动稍受限,暴露关节腔见关节液透明。见图10。"

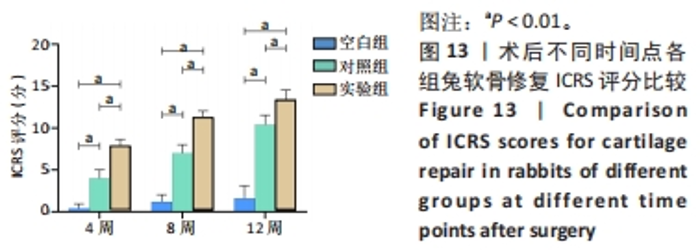
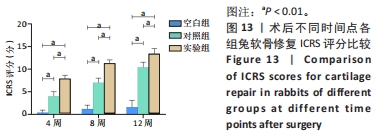
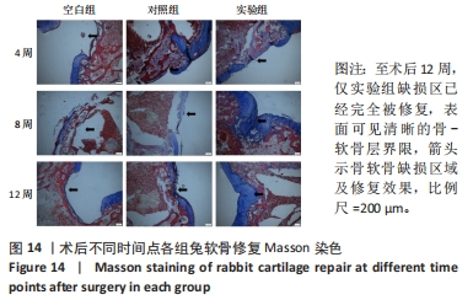
2.3.4 各组兔关节软骨大体观察及ICRS软骨修复评分 空白组、对照组术区均有明显粘连,其中一些液体为黄色,轻微红肿;实验组2只兔术区有轻微粘连,其余兔关节和关节囊均无异常,无明显的滑膜炎和骨赘。空白组术后4-12周缺损部位没有愈合,缺损部位和正常软骨之间的界限清楚。对照组术后4周缺损区无明显修复,8周后术区已被局部软组织覆盖,并出现了局部凹陷;术后12周,术区周边被透明软骨和纤维组织包裹,但中心凹痕依然清晰可见且边缘清晰。实验组术后4周修复区域仍呈明显的凹形,并有一层新的纤维层包裹在其表面;术后8周,术区内充盈纤维及透明软骨;第12周,术区被新的软骨细胞替代,表面平整、光滑,缺损处与关节面边界模糊。各组兔关节软骨大体观察见图12。"

| [1] DING H, CHENG Y, NIU X, et al. Application of electrospun nanofibers in bone, cartilage and osteochondral tissue engineering. J Biomater Sci Polym Ed. 2021;32(4):536-561. [2] VAISH A, SHANMUGASUNDARAM S, KIM SA, et al. Biological reconstruction of the joint: Concepts of articular cartilage regeneration and their scientific basis. J Clin Orthop Trauma. 2022;24:101718. [3] LIU Y, LI M, YIN Z, et al. SUMO-modified bone marrow mesenchymal stem cells promoted the repair of articular cartilage in rats. Cell Biol Int. 2020;44(2):560-568. [4] LI H, CAO X, WANG J, et al. [Redintegration of articular surface and alignment with tibia type III Pilon fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012;26(8):926-929. [5] LEE CH, KWON Y, JUNG IY, et al. Effect of the Articular Surface Incongruency on Surgical Outcome of the Distal Radius Fracture. Biomed Res Int. 2022;2022:8357675. [6] COOK JL, RUCINSKI K, CRECELIUS CR, et al. Initial Outcomes After Unicompartmental Tibiofemoral Bipolar Osteochondral and Meniscal Allograft Transplantation in the Knee Using MOPS-Preserved Fresh (Viable) Tissues. Am J Sports Med. 2023;51(3):596-604. [7] FLETCHER AN, JOHNSON LG, EASLEY ME, et al. Midterm Prospective Evaluation of Structural Allograft Transplantation for Osteochondral Lesions of the Talar Shoulder. Foot Ankle Int. 2022;43(7):899-912. [8] DHILLON J, DECILVEO AP, KRAEUTLER MJ, et al. Third-Generation Autologous Chondrocyte Implantation (Cells Cultured Within Collagen Membrane) Is Superior to Microfracture for Focal Chondral Defects of the Knee Joint: Systematic Review and Meta-analysis. Arthroscopy. 2022;38(8):2579-2586. [9] SCHUETTE HB, KRAEUTLER MJ, SCHROCK JB, et al. Primary Autologous Chondrocyte Implantation of the Knee Versus Autologous Chondrocyte Implantation After Failed Marrow Stimulation: A Systematic Review. Am J Sports Med. 2021;49(9):2536-2541. [10] LEE H, KIM HT, JO S. Femoral head cartilage reconstruction using autologous osteochondral mosaicplasty: A case report. Medicine (Baltimore). 2023;102(6):e32913. [11] YU JR, NAVARRO J, COBURN JC, et al. Current and Future Perspectives on Skin Tissue Engineering: Key Features of Biomedical Research, Translational Assessment, and Clinical Application. Adv Healthc Mater. 2019;8(5):e1801471. [12] YANG Z, WANG B, LIU W, et al. In situ self-assembled organoid for osteochondral tissue regeneration with dual functional units. Bioact Mater. 2023;27:200-215. [13] SHI Y, HAN X, PAN S, et al. Gold Nanomaterials and Bone/Cartilage Tissue Engineering: Biomedical Applications and Molecular Mechanisms. Front Chem. 2021;9:724188. [14] OMID H, ABDOLLAHI S, BONAKDAR S, et al. Biomimetic vascular tissue engineering by decellularized scaffold and concurrent cyclic tensile and shear stresses. J Mater Sci Mater Med. 2023;34(3):12. [15] YU H, FENG M, MAO G, et al. Implementation of Photosensitive, Injectable, Interpenetrating, and Kartogenin-Modified GELMA/PEDGA Biomimetic Scaffolds to Restore Cartilage Integrity in a Full-Thickness Osteochondral Defect Model. ACS Biomater Sci Eng. 2022;8(10):4474-4485. [16] HE T, LI B, COLOMBANI T, et al. Hyaluronic Acid-Based Shape-Memory Cryogel Scaffolds for Focal Cartilage Defect Repair. Tissue Eng Part A. 2021;27(11-12):748-760. [17] WANG T, XU W, ZHAO X, et al. Repair of osteochondral defects mediated by double-layer scaffolds with natural osteochondral-biomimetic microenvironment and interface. Mater Today Bio. 2022;14:100234. [18] KIM JW, LEE KJ. Development of a Single-nucleotide Polymorphism Genotyping Assay for the Rapid Detection of Vancomycin-intermediate Resistance in Staphylococcus aureus Epidemic Lineage ST5. Ann Lab Med. 2023;43(4):355-363. [19] LANDERSDORFER CB, LEE WL, NATION RL, et al. Penetration of Vancomycin into Noninfected Bone in Patients Undergoing Total Joint Arthroplasty Evaluated by a Minimal Physiologically Based Population Pharmacokinetic Modeling Approach. Mol Pharm. 2023;20(3):1509-1518. [20] MOSTAFA AA, EL-SAYED M, MAHMOUD AA, et al. Bioactive/Natural Polymeric Scaffolds Loaded with Ciprofloxacin for Treatment of Osteomyelitis. AAPS PharmSciTech. 2017;18(4):1056-1069. [21] WANG G, CUI Y, LIU H, et al. Antibacterial peptides-loaded bioactive materials for the treatment of bone infection. Colloids Surf B Biointerfaces. 2023;225:113255. [22] KHAYAT KASHANI HR. Answer to the letter to the editor of M. Kataria et al. concerning “Local vancomycin therapy to reduce surgical site infection in adult spine surgery: a randomized prospective study” by Salimi S, et al. (Eur Spine J [2022];31:454-460). Eur Spine J. 2023;32(3):1090. [23] LI S, SHI X, XU B, et al. In vitro drug release and antibacterial activity evaluation of silk fibroin coated vancomycin hydrochloride loaded poly (lactic-co-glycolic acid) (PLGA) sustained release microspheres. J Biomater Appl. 2022;36(9):1676-1688. [24] LI J, LI K, DU Y, et al. Dual-Nozzle 3D Printed Nano-Hydroxyapatite Scaffold Loaded with Vancomycin Sustained-Release Microspheres for Enhancing Bone Regeneration. Int J Nanomedicine. 2023;18:307-322. [25] 肖红利,邓江,韩子冀,等.渐进性梯度孔径骨软骨支架的制备及细胞相容性研究[J].中华老年医学杂志,2020,39(4):456-461. [26] SALTZMAN BM, RIBOH JC. Subchondral Bone and the Osteochondral Unit: Basic Science and Clinical Implications in Sports Medicine. Sports Health. 2018;10(5):412-418. [27] ZHANG Y, YU J, REN K, et al. Thermosensitive Hydrogels as Scaffolds for Cartilage Tissue Engineering. Biomacromolecules. 2019;20(4):1478-1492. [28] DONELL S. Subchondral bone remodelling in osteoarthritis. EFORT Open Rev. 2019;4(6):221-229. [29] LI B, DING T, CHEN H, et al. CircStrn3 targeting microRNA-9-5p is involved in the regulation of cartilage degeneration and subchondral bone remodelling in osteoarthritis. Bone Joint Res. 2023;12(1):33-45. [30] JACOB G, SHIMOMURA K, NAKAMURA N. Osteochondral Injury, Management and Tissue Engineering Approaches. Front Cell Dev Biol. 2020;8:580868. [31] FU L, YANG Z, GAO C, et al. Advances and prospects in biomimetic multilayered scaffolds for articular cartilage regeneration. Regen Biomater. 2020;7(6):527-542. [32] LE TM, VU NB, HUYNH PD, et al. Treatment of Osteochondral Femoral Head Defect by Human Umbilical Cord Mesenchymal Stem Cell Sheet Transplantation: An Experimental Study in Rats. Adv Exp Med Biol. 2021. doi: 10.1007/5584_2021_671. [33] VAN TUIJN IM, EMANUEL KS, VAN HUGTEN P, et al. Prognostic Factors for the Clinical Outcome after Microfracture Treatment of Chondral and Osteochondral Defects in the Knee Joint: A Systematic Review. Cartilage. 2023;14(1):5-16. [34] OTLANS P, LATTERMANN C, SHERMAN SL, et al. Cartilage Disease of the Patellofemoral Joint: Realignment, Restoration, Replacement. Instr Course Lect. 2021;70:289-308. [35] MICHALIK R, PAUER T, BRILL N, et al. Quantitative articular cartilage sub-surface defect assessment using optical coherence tomography: An in-vitro study. Ann Anat. 2019;221:125-134. [36] HIGA K, KITAMURA N, GOTO K, et al. Effects of osteochondral defect size on cartilage regeneration using a double-network hydrogel. BMC Musculoskelet Disord. 2017;18(1):210. [37] LUO M, CHEN M, BAI J, et al. A bionic composite hydrogel with dual regulatory functions for the osteochondral repair. Colloids Surf B Biointerfaces. 2022;219:112821. [38] ALOMAR AZ, SOMILY AM, ALRAIYES TM, et al. Quantification Analysis of the Intraoperative Bacterial Contamination Rate and Level in Osteochondral Autografts. Am J Sports Med. 2016; 44(3):761-766. [39] WEI J, XIA X, XIAO S, et al. Sequential Dual-Biofactor Release from the Scaffold of Mesoporous HA Microspheres and PLGA Matrix for Boosting Endogenous Bone Regeneration. Adv Healthc Mater. 2023;12(20):e2300624. [40] WANG W, SONG Y, TIAN Y, et al. TCPP/MgO-loaded PLGA microspheres combining photodynamic antibacterial therapy with PBM-assisted fibroblast activation to treat periodontitis. Biomater Sci. 2023;11(8):2828-2844. [41] GANDOMKARZADEH M, MOGHIMI HR, MAHBOUBI A. Evaluation of the Effect of Ciprofloxacin and Vancomycin on Mechanical Properties of PMMA Cement; a Preliminary Study on Molecular Weight. Sci Rep. 2020;10(1):3981. [42] LIU N, HUANG S, GUO F, et al. Calcium phosphate cement with icariin-loaded gelatin microspheres as a local drug delivery system for bone regeneration. Biomed Eng Online. 2022;21(1):89. [43] GHAREH SM, SHABANI RN, BEHROUZI M, et al. Engineered PLGA microspheres for extended-release of naltrexone: in vitro, in vivo, and IVIVR. Pharm Dev Technol. 2023;28(2):190-199. [44] 刘华蔚.壳聚糖导管复合NGF缓释微球修复兔面神经缺损的实验研究[D].北京:解放军医学院,军医进修学院,解放军总医院,2011. [45] FAN L, TENG W, HE J, et al. Value of 3D Printed PLGA Scaffolds for Cartilage Defects in Terms of Repair. Evid Based Complement Alternat Med. 2022;2022:3561430. [46] LUO M, CHEN M, BAI J, et al. A bionic composite hydrogel with dual regulatory functions for the osteochondral repair. Colloids Surf B Biointerfaces. 2022;219:112821. [47] 高泽,石志良,李锋,等.材料和孔隙率对可降解支架内骨形成的影响[J].医用生物力学, 2021,36(4):582-588. [48] PRANANINGRUM W, NAITO Y, GALLI S, et al. Bone ingrowth of various porous titanium scaffolds produced by a moldless and space holder technique: an in vivo study in rabbits. Biomed Mater. 2016;11(1):15012. [49] MOURA CS, SILVA JC, FARIA S, et al. Chondrogenic differentiation of mesenchymal stem/stromal cells on 3D porous poly (epsilon-caprolactone) scaffolds: Effects of material alkaline treatment and chondroitin sulfate supplementation. J Biosci Bioeng. 2020;129(6):756-764. [50] MARTINS EA, MICHELACCI YM, BACCARIN RY, et al. Evaluation of chitosan-GP hydrogel biocompatibility in osteochondral defects: an experimental approach. BMC Vet Res. 2014;10:197. [51] ZHU D, WANG H, TRINH P, et al. Elastin-like protein-hyaluronic acid (ELP-HA) hydrogels with decoupled mechanical and biochemical cues for cartilage regeneration. Biomaterials. 2017; 127:132-140. [52] 向柄彦,李鹏,柏帆,等.载万古霉素缓释微球纳米羟基磷灰石/壳聚糖支架联合自体红骨髓可修复慢性骨髓炎兔的骨缺损[J].中国组织工程研究,2019,23(6):843-848. [53] LI J, LI K, DU Y, et al. Dual-Nozzle 3D Printed Nano-Hydroxyapatite Scaffold Loaded with Vancomycin Sustained-Release Microspheres for Enhancing Bone Regeneration. Int J Nanomedicine. 2023;18:307-322. [54] 马涛,尚北城,陈庆华,等.万古霉素阳离子脂质体复合纳米羟基磷灰石/壳聚糖/魔芋葡苷聚糖支架的制备与降解及药物的体外释放研究[J].中华创伤骨科杂志,2014,16(10):891-897. [55] 冯建波,李陈诚,刘金月,等.金黄色葡萄球菌生物膜克氏针置入建立创伤性大鼠骨髓炎模型[J].中国组织工程研究,2022,26(5):700-705. [56] 唐洪.自体软骨微粒复合仿生凝胶修复局灶性关节软骨缺损研究[D].重庆:第三军医大学,2016. |
| [1] | Yang Yufang, Yang Zhishan, Duan Mianmian, Liu Yiheng, Tang Zhenglong, Wang Yu. Application and prospects of erythropoietin in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1443-1449. |
| [2] | Chen Kaijia, Liu Jingyun, Cao Ning, Sun Jianbo, Zhou Yan, Mei Jianguo, Ren Qiang. Application and prospect of tissue engineering in treatment of osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1450-1456. |
| [3] | Wang Shanshan, Shu Qing, Tian Jun. Physical factors promote osteogenic differentiation of stem cells [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1083-1090. |
| [4] | Mei Jingyi, Liu Jiang, Xiao Cong, Liu Peng, Zhou Haohao, Lin Zhanyi. Proliferation and metabolic patterns of smooth muscle cells during construction of tissue-engineered blood vessels [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(7): 1043-1049. |
| [5] | Chen Xiaofang, Zheng Guoshuang, Li Maoyuan, Yu Weiting. Preparation and application of injectable sodium alginate hydrogels [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 789-794. |
| [6] | Wang Jiani, Chen Junyu. Angiogenesis mechanism of metal ions and their application in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 804-812. |
| [7] | Wang Wu, Fan Xiaolei, Xie Jie, Hu Yihe, Zeng Min. Hydroxyapatite-polyvinyl alcohol/collagen-chitosan-gelatin composite hydrogel for repairing rabbit osteochondral defect [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 682-689. |
| [8] | Shen Ziqing, Xia Tian, Shan Yibo, Zhu Ruijun, Wan Haoxin, Ding Hao, Pan Shu, Zhao Jun. Vascularized tracheal substitutes constructed by exosome-load hydrogel-modified 3D printed scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 697-705. |
| [9] | Wang Jianchun, Yang Shuqing, Su Xin, Wang Hongyuan. Different contents of B2O3 affect mechanical properties and bioactivity of bioactive glass scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 712-716. |
| [10] | Zhang Yihai, Shang Peng, Ma Benyuan, Hou Guanghui, Cui Lunxu, Song Wanzhen, Qi Dexuan, Liu Yancheng. Structural design and mechanical property analysis of trabecular scaffold of triply periodic minimal surface with a radial gradient [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 741-746. |
| [11] | Zhu Liwei, Wang Jiangyue, Bai Ding. Application value of nanocomposite gelatin methacryloyl hydrogels in different bone defect environments [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 753-758. |
| [12] | Yang Yuqing, Chen Zhiyu. Role and application of early transient presence of M1 macrophages in bone tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 594-601. |
| [13] | Li Yulin, Yu Haipeng, Tang Huajing, Zhang Zitong, Lin Xingnan. The mechanism, safety and application of berberine in promoting bone regeneration [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(35): 5702-5708. |
| [14] | Yu Pengxin, Han Yuqiu, Guo Lina, Wang Xiuli. The construction of rat intestinal smooth muscle collagen band and evaluation of periodic stretching culture in vitro [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(35): 5630-5635. |
| [15] | Shang Yonghui, Li Shuai, Liu Yicong, Zhao Qihang, Liu Wen. Three-dimensional finite element study on the effect of posterior tooth forward movement on temporomandibular joint stress in orthodontic reduction patients [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(34): 5516-5520. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||