Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (15): 2398-2403.doi: 10.12307/2024.388
Previous Articles Next Articles
Biomaterials and pore characteristics of tendon tissue engineering scaffolds
Wang Xiaolong1, Huang Haoran1, Zhang Zhongxin1, Wang Limin2, Hu Yongcheng3
- 1Chengyang District People’s Hospital, Qingdao 266109, Shandong Province, China; 2Beijing Weidafeng Medical Biomaterials Co., Ltd., Beijing 101100, China; 3Tianjin Hospital, Tianjin 300202, China
-
Received:2023-04-20Accepted:2023-07-04Online:2024-05-28Published:2023-09-23 -
Contact:Hu Yongcheng, Chief physician, Professor, Tianjin Hospital, Tianjin 300202, China -
About author:Wang Xiaolong, Master, Attending physician, Chengyang District People’s Hospital, Qingdao 266109, Shandong Province, China
CLC Number:
Cite this article
Wang Xiaolong, Huang Haoran, Zhang Zhongxin, Wang Limin, Hu Yongcheng. Biomaterials and pore characteristics of tendon tissue engineering scaffolds[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(15): 2398-2403.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

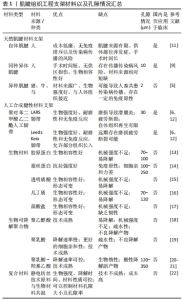
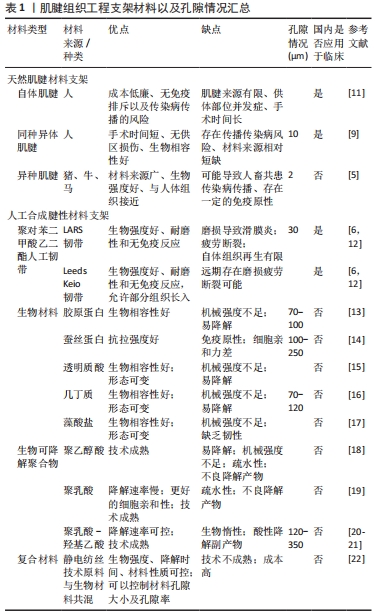
2.1.1 天然材料肌腱支架 天然材料肌腱支架主要包括自体肌腱、同种异体肌腱和异种肌腱3种。 自体肌腱是目前临床上开展最为广泛的肌腱移植手术材料,尤其是在前交叉韧带重建术中的使用[23],其具有成本低廉、不存在免疫排斥及传染病传播的风险、术后远期效果良好等优点。骨-髌腱-骨和半腱肌、股薄肌腱自体移植物是目前前交叉韧带重建中最常用的移植物。虽然骨-髌腱-骨自体移植物是以前的“金标准”,但最近的研究已经确定四股半腱肌移植物是前交叉韧带重建的较好选择[24]。腘绳肌移植物固定技术的进步与骨-髌腱-骨与半腱肌、股薄肌移植物之间的固定强度相似。这两种技术为重建韧带提供了较高的强度和刚度[25]。 对于自体髌腱移植物,许多患者在供体部位经历功能受损和包括继发性膝前疼痛、髌腱炎、髌下挛缩和髌骨骨折的发病困扰。同样,在自体半腱肌、股薄肌前交叉韧带重建的患者中,出现腘绳肌损伤和隐神经损伤并发症的概率居高不下[26]。还有部分研究显示,在长期随访中自体骨-髌腱-骨移植物的稳定性要优于自体半腱肌、股薄肌移植物的前交叉韧带重建,因此在自体肌腱供区的选择上还存在一定争议[27]。 同种异体肌腱与自体肌腱相比具有显著的优势,包括:能够缩短手术时间和减少患者自体取肌腱所致的术后并发症;肌腱量充足,能够保证重建肌腱的长度和直径,易于手术操作和固定;具有与人体接近的组织构成及生物相容性;能够避免细胞外蛋白基质的降解,维持整个健骨愈合过程中的抗拉伸性能[7]。已有研究证明,同种异体移植物和自体移植物在前交叉韧带重建中有着相似的临床结果[28]。尽管同种异体移植物和自体移植物之间存在基本的科学差异,但临床研究并未发现二者用于前交叉韧带重建时的显著差异,两种移植物均有相当好的或极好的重建结果[28-32]。PEARSALL等[33]对同种异体双股胫前肌腱的力学测量发现,其力学各方面数据优于原生前交叉韧带。也有其他研究表明,采用同种异体移植物重建前交叉韧带的膝关节松弛程度比自体移植物更大[34-36]。总的共识是:同种异体移植物在恢复稳定性、活动范围和主观膝关节评分方面与自体移植物相差不大。此外多项研究表明,同种异体肌腱在二次翻修手术中应用更多,在翻修手术中使用同种异体移植物可有效改善症状、稳定性、功能限制和主观膝关节评分[29,31]。 在同种异体肌腱使用安全性等方面,目前还没有确切的数据说明使用异体软组织移植相关的HIVⅠ/Ⅱ、乙型肝炎病毒或丙型肝炎病毒传播风险。对于外科医生来说,在使用异体移植物之前了解软组织库的制备方法是谨慎的。尽管少有报道因同种异体移植物导致感染细菌及病毒的案例,但那些极少数进行同种异体移植术后感染的案例让医生触目惊心[37]。尽管同种异体移植组织捐献、获取、测试、加工、保存、储存和分发的安全标准有所提高,但不能完全排除通过同种异体移植组织传播疾病和恶性肿瘤的风险,这种事件可能导致潜在的危及生命并发症,所以同种异体肌腱的消毒及储存方案有待于进一步的研究。 随着肌腱脱细胞技术的成熟及同种异体肌腱来源的短缺,异种肌腱的研究逐渐被重视。异种肌腱较其他两种天然腱性组织的潜在优势包括以下几点[10]:容易获得无供体病变的组织来源;减少疾病传播;增加组织材料和物理特性的同质性;缩短手术时间。最近,来自畜牧业的异种移植物因其材料的广泛性已成为异种移植物市场的主要肌腱来源,猪、牛和马来源的移植物因其在尺寸和生物力学特性上的相似性,目前被考虑为是与人体最接近的异种移植物组织[38]。猪作为供体物种具有来源广泛、价格低廉的优势,但由于人猪共患疾病的原因使得这种肌腱具有一定传播病原体的风险[39]。据此,马异种移植物越来越多地被用于异种肌腱研究中[40]。 虽然异种肌腱在材料获取及肌腱的强度方面有着得天独厚的优势,但是异体动物移植组织内存在的α半乳糖抗原会引起人体的超急性排斥反应,现有的处理方式只能部分去除此类抗原(诸如通过十二烷基硫酸钠洗涤剂或α半乳糖酶处理),但该处理方法并没有完全消除α半乳糖抗原,可在后续裸鼠体内观察到对异种肌腱的弱毒免疫反应。因此,异种肌腱的成功开发及应用可能需要进一步的研究[41]。 2.1.2 人工合成腱性支架 最早的人工合成肌腱是1973年由美国Vitek公司生产的名为Proplast(聚芳纶纤维和乙烯聚合物合成)的支架材料,这种材料具有足够强的韧性及无免疫原性,并且在动物实验中发现该材料允许细胞向内生长且固定于骨界面,被临床广泛使用。在接下来的10年里,又有像涤纶、GORE-TEXVR和其他用不可生物降解聚合物制成的移植物被发明利用,但后期发现这种强度过高的支架材料都会导致膝关节磨损,引起颗粒性滑膜炎和/或移植物失效的类似问题,美国食品和药品监管局便停止了此类人工韧带的使用[42-45]。 虽然用于人工韧带织物材料的改进停止了,但人工韧带仍然在临床中继续使用,相关研究也在不断报道[12]。现阶段以Leeds Keio、LARS为代表的人工韧带产品在临床应用中虽然表现出了良好的初始力学强度及术后关节稳定性,但由于材料本身的黏弹性缺乏、磨损老化以及有限的自体组织再生,远期随访尚不能排除可能导致滑膜炎、移植物力学强度受损甚至失效等问题,使人工韧带的临床应用备受争议[46]。 目前许多含有生物蛋白组织的合成生物材料腱性支架被研究开发,这种材料统称为组织工程支架,包括生物材料、生物可降解聚合物和复合材料,这种支架主要包含以下几个特点:可生物降解;允许组织长入;促进韧带再生所需的细胞过程。20世纪90年代,由肌腱的基本成分Ⅰ型胶原所构建的支架材料被开发,但在动物实验中发现其抗降解能力较差,6周内就会被完全吸收,后续研究通过将胶原蛋白与化学试剂交联等方法增加了支架的抗降解能力且增强了生物力学性能,但其机械性能仍低于预期,需进一步探索[47-50]。与胶原蛋白类似,蚕丝蛋白作为一种可降解材料弥补了胶原蛋白的不足,它在体内能保持1年的拉力强度,2年时间可以被完全降解,且与人体组织具有高度的生物相容性,但存在制作成本高、工艺复杂、不能促进细胞的黏附增殖、细胞亲和力较差等不足,仍需进一步研究。 生物可降解聚合物材料所制备的肌腱组织工程支架于20世纪末被发明,由最初的降解过快、强度不足的聚乙醇酸支架到降解减慢但降解产物有害的聚乳酸支架再到降解速率可控但降解产物仍然有害的聚乳酸-羟基乙酸支架[51-53],研究人员发现通过单一材料的研究难以达到良好的材料性质要求,因此复合材料被逐渐发掘。 复合材料最常用制造技术之一是编织,类似于纺织工业。过去20年中很受欢迎的方法是静电纺丝,通过纺丝技术与天然生物材料相结合共同编织的生物复合材料逐渐被挖掘。在21世纪初,LI等[54-55]首次将该技术应用于生物医学研究。较上面所提及的Leeds Keio、LARS人工韧带,这种电纺丝技术把原材料与生物材料合成,并且可操控编织的孔隙保证正常组织浸润生长,并且具有一定的可降解性。BOURKE等[56]研究了编织聚二氨基酪氨酸碳酸乙酯支架,并证明了该支架支持成纤维细胞的生长,并显示出用作前交叉韧带移植所需的强度。SURRAO等[57]报道了将一种静电纺丝聚酯纤维包埋在非细胞贴壁的光交联N-甲基丙烯酸乙二醇壳聚糖水凝胶中,并在体外证明了良好的细胞活力和细胞外基质沉积。将疏水聚己内酯和亲水聚乙醇酸-聚己内酯-聚乙醇酸三嵌段共聚物共混物静电纺丝制成支架,通过改变聚己内酯和聚乙醇酸- 聚己内酯-聚乙醇酸共聚物的比例来控制这些支架的亲水性、机械强度和降解率等性能,但是其远期效果并没有被进一步证实。 其他生物材料如透明质酸、海藻酸盐和壳聚糖等已被组织工程广泛运用,研究人员开发了多种改性方法,但仍未克服其固有的确定缺点(如材料强度、韧性),需要进一步的研究来确定它们在肌腱组织工程中的潜在用途[38]。 2.2 肌腱组织工程生物材料的孔隙率 肌腱愈合以及肌腱再生是一个缓慢的过程,通过移植周围细胞的增殖分化黏附重建逐步愈合。MALININ等[58]对9例前交叉韧带重建患者进行了异体移植物恢复研究,发现前交叉韧带移植物的重塑是一个渐进或缓慢的过程,整个移植物的完全重塑和细胞置换可能需要3年或更长时间。早期愈合始于成纤维细胞,外在愈合始于肌腱鞘和周围软组织的成纤维细胞和炎症细胞入侵增殖,形成新的胶原基质。在黏附过程中,肌腱与骨表面之间的接触面积以及肌腱表面较小的孔径(小于150 μm)能够促进成纤维细胞的黏附,这一效应可能是由材料表面积、粗糙度的增加或通过微机械性能的调节所驱动的。然而,孔隙大小也与整体孔隙度密切相关,孔隙越大孔隙度越高[59-61]。较高的孔隙率改善了营养物质的质量运输、增加了成纤维细胞的增殖和迁移,并能够更深地渗透到支架中[62-65]。总的来说,大孔隙、高孔隙度支架提高的细胞增殖速率抵消了小孔隙带来的最初优势[66]。高孔隙率也能够调节异物反应,可能是通过调控巨噬细胞种群偏向M2表型[67](偏向愈合的表型)。此外,ARTEL等[68]通过计算模型发现,适当的血管化结构需要160-270 μm的大孔径,具有较高连通性但孔隙率不变的支架有利于成纤维细胞向支架内迁移。MURPHY等[69]通过胶原-糖胺聚糖支架发现,平均孔径为325 μm的支架被认为是骨组织工程的最佳选择。KUBOKI等[70]通过大鼠体内植入不同孔隙大小的材料诱导成骨发现,羟基磷灰石多孔块中骨形成效果的最佳孔径为300-400 μm;在蜂窝状羟基磷灰石中,具有较小直径(90-120 μm)的隧道诱导软骨形成,随后形成骨,而具有较大直径(350 μm)的那些隧道直接在隧道内诱导骨形成。然而,重要的是要确定孔径的上限,因为大的孔隙可能会增加孔隙体积,从而损害支架的力学性能[69]。 在同种异体肌腱的研究中发现,去除细胞及感染性物质等过程导致了肌腱孔隙率的增加,从而导致体内细胞浸润的增加。WHITLOCK等[9]研究发现,处理人同种异体肌腱的过程会导致肌腱的孔隙及渗透性增加,动物体内实验证明处理后的人肌腱细胞浸润深度大于处理前肌腱,表明化学物理以及酶处理的肌腱能够增加细胞增殖、促进愈合,但其具体机制有待进一步探索。在动物同种异体肌腱的模型当中也发现相同的现象。XU等[71]采用过氧乙酸-乙醇溶液处理对同种异体人肌腱,发现肌腱组织具有更大的组织间隙,这种组织间隙可能是由于过氧乙酸在基质中分解产生的氧气气泡造成的,这种开放也可能使移植物在体内更快地被宿主细胞穿透,可能会导致植入后移植物和宿主组织融合率的提高。 在异种肌腱的开发过程中也同样发现了此类现象。SEYLER等[5]通过使用结合物理、化学和酶的脱细胞方案对猪髌腱肌腱进行结构修饰,发现支架上的细胞结构减少、DNA含量显著降低,肌腱纤维束之间的间距明显增大,肌腱孔隙率由(37.70±4.25)%增加到(68.43±8.76)%,平均孔径由(0.24±0.11) μm增加到(2.32±2.36) μm;在体外细胞实验中发现,处理后肌腱的细胞相容性明显较高;未处理肌腱和处理后肌腱的极限拉伸载荷、刚度和弹性模量无差异。 聚对苯二甲酸乙二酯人工韧带目前是人工韧带临床应用的主力军,以LARS和Leedse Keio韧带为代表的人工韧带在欧洲和亚洲被广泛使用[46]。MA等[12]通过热压缩法改变孔径和孔隙率来制造不同孔径的聚对苯二甲酸乙二酯材料,发现低孔隙组具有84.9%的孔隙率和30 μm的平均孔径,而高孔隙组具有89.6%的孔隙率和39 μm的平均孔径;通过培养滋养层ED27细胞发现,低孔隙基质中的初始细胞增殖率高于高孔隙基质,但是低孔隙基质的较小孔径限制了大细胞聚集体的形成并降低了细胞分化。MA等[12]还观察了使用聚对苯二甲酸乙二酯纤维制造的3D非织造基质对大鼠间充质干细胞增殖和成骨分化的影响,结果发现具有更大直径(> 12 μm)、较高孔隙率(约96.7%)的聚对苯二甲酸乙二酯纤维基质增强了细胞增殖率,这可能是由于促进了营养物和氧在体外的转运。因此,细胞行为可受材料性质(例如孔隙率、孔径、互连性和纤维直径)的影响。 生物相容性和机械强度是评估组织工程化韧带的2个关键特性[72]。此外,适当的生物降解速率也是软组织再生的决定性因素[73]。在组织工程化韧带研究中已经采用了许多生物材料,这些材料乍一看具有令人鼓舞的优势,然而一些研究发现了它们的缺陷[74]。不可否认,近年来,在组织工程化韧带项目中使用的生物材料取得了很大进展。ITOI等[75]通过脂肪干细胞测试Ⅰ型胶原海绵、无纺布聚乙醇酸或透明质酸凝胶3种临床常用组织工程支架的脂肪细胞相容性,发现Ⅰ型胶原海绵最能储存并诱导生成脂肪细胞,测得孔径范围为70-110 μm,但Ⅰ型胶原海绵的孔隙率并未进一步测量。BIMAN等[76]研究了不同冷冻温度下蚕丝蛋白三维支架的微观结构,形成了直径为200-250 μm的孔隙,发现该大小孔隙有利于人类真皮成纤维细胞的浸润增殖。 早期静电纺纤维支架的一个基本缺点是其低孔隙率和不适合植入细胞浸润[77]。OLVERA等[78]通过改变收集芯轴的转速设计了一种多孔三维(3D)超纤维支架,纤维的孔隙率为95%,使静电纺丝板更容易弯曲,其力学性能与天然前交叉韧带相似。更高的孔隙度也允许间充质干细胞更好地浸泡在植入物中。为了在增大纤维尺寸的同时增强细胞的附着、扩散和增殖,研究人员缩短了喷嘴与收集器之间的距离,以N,N-二甲基甲酰胺/NaOH为溶剂静电纺丝透明质酸/胶原蛋白混合物,并在静电纺丝过程中通过化学交联和氯化钠颗粒浸泡在整个支架上产生特定孔径。 GUNER等[79]将旋喷纺丝和湿静电纺丝生产的纤维垫组装成双相纤维支架,双相支架的外壳由对齐的聚己内酯纤维组成,以确保更好的力学性能和强度;支撑芯由聚己内酯或聚己内酯/明胶纤维组成,其排列是随机的,提供了适合细胞黏附的仿生结构。随后的体外研究表明,核心纤维随机排列在双相支架对齐的聚己内酯纤维壳中,提高了小鼠成纤维细胞系的初始黏附、增殖和分化。聚己内酯纤维的排列可以促进排列纤维的伸长,从而通过引导细胞增殖和细胞外基质沉积来促进肌腱组织愈合。"

| [1] PATEL S, CALDWELL JM, DOTY SB, et al. Integrating Soft and Hard Tissues via Interface Tissue Engineering. J Orthop Res. 2018;36(4):1069-1077. [2] WHITLOCK PW, SMITH TL, POEHLING GG, et al. A naturally derived cytocompatible, and architecturally optimized scaffold for tendon and ligament regeneration. Biomaterials. 2007;28(29):4321-4329. [3] HINSENKAMP M, MUYLLE L, EASTLUND T, et al. Adverse reactions and events related to musculoskeletal allografts: Reviewed by the World Health Organisation Project NOTIFY. Int Orthop. 2012;36:633-641. [4] MALLICK TK, MOSQUERA A, ZINDERMAN CE, et al. Reported infections after human tissue transplantation before and after new Food and Drug Administration (FDA) regulations, United States, 2001 through June, 2010. Cell Tissue Bank. 2012;13:259-267. [5] SEYLER TM, BRACEY DN, PLATE JF, et al. The Development of a Xenograft-Derived Scaffold for Tendon and Ligament Reconstruction Using a Decellularization and Oxidation Protocol. Arthroscopy. 2017;33(2):374-386. [6] CHEN T, JIANG J, CHEN S. Status and headway of the clinical application of artificial ligaments. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(1):15-26. [7] LIM WL, LIAU LL, NG MH, et al. Current Progress in Tendon and Ligament Tissue Engineering. Tissue Eng Regen Med. 2019;16(6):549-571. [8] CHEN B, WANG B, ZHANG WJ, et al. In vivo tendon engineering with skeletal muscle derived cells in a mouse model. Biomaterials. 2012;33(26):6086-6097. [9] WHITLOCK PW, SEYLER TM, PARKS GD, et al. A novel process for optimizing musculoskeletal allograft tissue to improve safety, ultrastructural properties, and cell infiltration. J Bone Joint Surg Am. 2012;94(16):1458-1467. [10] OZASA Y, AMADIO PC, THORESON AR, et al. Repopulation of intrasynovial flexor tendon allograft with bone marrow stromal cells: an ex vivo model. Tissue Eng Part A. 2014;20(3-4):566-574. [11] LORD BR, EL-DAOU H, SABNIS M, et al. Biomechanical comparison of graft structures in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):559-568. [12] MA T, LI Y,YANG ST, et al. Effects of pore size in 3-D fibrous matrix on human trophoblast tissue developmen. Biotechnol Bioeng. 2000;70(6):606-618. [13] ITOI Y, TAKATORI M, HYAKUSOKU H, et al. Comparison of readily available scaffolds for adipose tissue engineering using adipose-derived stem cells. J Plast Reconstr Aesthet Surg. 2010;63(5):858-864. [14] MANDAL B, KUNDU S. Cell proliferation and migration in silk fibroin 3D scaffolds. Biomaterials. 2009;30(15):2956-2965. [15] CRISTINO S, GRASSI F, TONEGUZZI S, et al. Analysis of mesenchymal stem cells grown on a three-dimensional HYAFF 11-based prototype ligament scaffold. J Biomed Mater Res A. 2005;73:275-283. [16] GRIFFON DJ, SEDIGHI MR, SCHAEFFER DV, et al.Chitosan scaffolds: interconnective pore size and cartilage engineering. Acta Biomater. 2006; 2(3):313-320. [17] YAMANE S, IWASAKI N, MAJIMA T, et al. Feasibility of chitosan-based hyaluronic acid hybrid biomaterial for a novel scaffold in cartilage tissue engineering. Biomaterials. 2005;26:611-619. [18] LIN VS, LEE MC, O’NEAL S, et al. Ligament tissue engineering using synthetic biodegradable fiber scaffolds. Tissue Eng. 1999;5:443-452. [19] LU HH, COOPER JR JA, MANUEL S, et al. Anterior cruciate ligament regeneration using braided biodegradable scaffolds:in vitro optimization studies. Biomaterials. 2005;26:4805e4816. [20] WANG M, PEI H, ZHANG L, et al. Hepatogenesis of adipose-derived stem cells on poly-lactide-co-glycolide scaffolds: in vitro and in vivo studies. Tissue Eng Part C Methods. 2010;16:1041. [21] LI J, TAO R, WU W, et al. 3D PLGA scaffolds improve differentiation and function of bone marrow mesenchymal stem cell-derived hepatocytes. Stem Cells Dev. 2010;19(9):1427-1436. [22] HOYER M, DRECHSEL N, MEYER M, et al. Embroidered polymer-collagen hybrid scaffold variants for ligament tissue engineering. Mater Sci Eng C Mater Biol Appl. 2014;43:290-299. [23] TALBOT M, BERRY G, FERNANDES J, et al.Knee dislocations:experience at the Hôpital du Sacré-Coeur de Montréal. Tissue Eng Part C Methods. 2010;16(5):1041-1050. [24] KRUDWIG WK. Anterior cruciate ligament reconstruction using an alloplastic ligament of polyethylene terephthalate (PET-Trevira-hochfest).Follow-up study. Biomed Mater Eng. 2002;12(1):59-67. [25] LIDÉN M, EJERHED L, SERNERT N, et al. Re: patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-Year follow-up. Am J Sports Med. 2007;35(5):740-748. [26] MASCARENHAS R, PETER B. MacDonald.Anterior cruciate ligament reconstruction: a look at prosthetics - past, present and possible future. McGill J Med. 2008;11(1):29-37. [27] GUOAN L, RAMPRASAD P, LOUIS ED, et al. Comparison of the ACL and ACL graft forces before and after ACL reconstruction. Acta Orthop. 2006; 77(2):267-274. [28] CAREY JL, DUNN WR, DAHM DL, et al. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009;91(9):2242-2250. [29] HARNER CD, OLSON E, IRRGANG JJ, et al. Allograft versus autograft anterior cruciate ligament reconstruction: 3- to 5-year outcome. Clin Orthop. 1996; 324:134-144. [30] PETERSON RK, SHELTON WR, BOMBOY AL. Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: a 5-year follow-up. Arthroscopy. 2001;17:9-13. [31] POEHLING GG, CURL WW, LEE CA, et al. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: allograft versus autograft. Arthroscopy. 2005;21:774-785. [32] SHELTON WR, PAPENDICK L, DUKES AD. Autograft versus allograft anterior cruciate ligament reconstruction. Arthroscopy. 1997;13:446-449. [33] PEARSALL IV AW, HOLLIS JM, RUSSELL GV JR, et al. A biomechanical comparison of three lower extremity tendons for ligamentous recons truction about the knee. Arthroscopy. 2003;19:1091-1096. [34] BARRETT G, STOKES D, WHITE M. Anterior cruciate ligament reconstruction in patients older than 40 years: allograft versus autograft patellar tendon. Am J Sports Med. 2005;33:1505-1512. [35] GROSSMAN MG, ELATTRACHE NS, SHIELDS CL, et al. Revision anterior cruciate ligament reconstruction: three to nine year follow-up. Arthroscopy. 2005;21:418-423. [36] URIBE JW, HECHTMAN KS, ZVIJAC JE, et al. Revision anterior cruciate ligament surgery: experience from Miami. Clin Orthop. 1996;325:91-99. [37] COHEN SB, SEKIYA JK. Allograft Safety in Anterior Cruciate Ligament Reconstruction. Clin Sports Med. 2007;26(4):597-605. [38] LEONG NL, PETRIGLIANO FA, MCALLISTER DR. Current tissue engineering strategies in anterior cruciate ligament reconstruction J Biomed Mater Res A. 2014;102(5):1614-1624. [39] BORIE DC, CRAMER DV, PHAN-THANH L, et al. Microbiological hazards related to xenotransplantation of porcine organs into man. Infect Control Hosp Epidemiol. 1998;19(5):355-365. [40] WEESE J. A review of equine zoonotic diseases: risks in veterinary medicine. Proc Ann Convent AAEP. 2002;48:362-369. [41] KONAKCI KZ, BOHLE B, BLUMER R, et al. Alpha-Gal on bioprostheses: Xenograft immune response in cardiac surgery. Euro J Clin Invest. 2005; 35:17-23. [42] BOLTON CW, BRUCHMAN WC. The GORE-TEX expanded polytetra-fluoroethylene prosthetic ligament. An in vitro and in vivo evaluation. Clin Orthop Relat Res 1985;(196):202-213. [43] RICHMOND JC, MANSEAU CJ, PATZ R, et al. Anterior cruciate reconstruction using a Dacron ligament prosthesis. A long-term study. Am J Sports Med. 1992;20(1):24-28. [44] RADING J, PETERSON L. Clinical experience with the Leeds-Keio artificial ligament in anterior cruciate ligament reconstruction. A prospective two-year follow-up study. Am J Sports Med. 1995;23(3):316-319. [45] FUJIKAWA K, ISEKI F, SEEDHOM BB. Arthroscopy after anterior cruciate reconstruction with the Leeds-Keio ligament. J Bone Joint Surg Br. 1989; 71(4):566-570. [46] CHEN T, JIANG J, CHEN S. Status and headway of the clinical application of artificial ligaments. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(1):15-26. [47] KOOB TJ, WILLIS TA, QIU YS, et al. Biocompatibility of NDGA-polymerized collagen fibers. II. Attachment, proliferation,and migration of tendon fibroblasts in vitro. J Biomed Mater Res. 2001;56:40-48. [48] CARUSO AB, DUNN MG. Changes in mechanical properties and cellularity during long-term culture of collagen fiber ACL reconstruction scaffolds. J Biomed Mater Res A. 2005;73:388-397. [49] DUNN MG, LIESCH JB, TIKU ML, et al. Development of fibroblast-seeded ligament analogs for ACL reconstruction. J Biomed Mater Res. 1995;29: 1363-1371. [50] BELLINCAMPI LD, CLOSKEY RF, PRASAD R, et al. Viability of fibroblast-seeded ligament analogs after autogenous implantation. J Orthop Res. 1998;16: 414-420. [51] JAMES R, TOTI US, LAURENCIN CT, et al. Electrospun nanofibrous scaffolds for engineering soft connective tissues. Methods Mol Biol. 2011;726: 243e258. [52] LIN VS, LEE MC, O’NEAL S, et al. Ligament tissue engineering using synthetic biodegradable fiber scaffolds. Tissue Eng. 1999;5:443e452. [53] LU HH, COOPER JR JA, MANUEL S, et al. Anterior cruciate ligament regeneration using braided biodegradable scaffolds: in vitro optimization studies. Biomaterials. 2005;26:4805-4816. [54] LI WJ, LAURENCIN CT, CATERSON EJ, et al. Electrospun nanofibrous structure: A novel scaffold for tissue engineering. J Biomed Mater Res. 2002;60:613-621. [55] MATTHEWS JA, WNEK GE, SIMPSON DG, et al. Electrospining of collagen nanofibers. Biomacromolecules. 2002;3:232-238. [56] BOURKE SL, KOHN J, DUNN MG. Preliminary development of a novel resorbable synthetic polymer fiber scaffold for anterior cruciate ligament reconstruction. Tissue Eng. 2004;10:43-52. [57] SURRAO DC, WALDMAN SD, AMSDEN BG. Biomimetic poly(lactide) based fibrous scaffolds for ligament tissue engineering. Acta Biomater. 2012;8(11):3997-4006. [58] MALININ TI, LEVITT RL, BASHORE C, et al. A study of retrieved allografts used to replace anterior cruciate ligaments. Arthroscopy. 2002;18:163-170. [59] GRIER WK, IYOHA EM, HARLEY BAC. The influence of pore size and stiffness on tenocyte bioactivity and transcriptomic stability in collagen –GAG scaffolds. J Mech Behav Biomed Mater. 2017;65:295-305. [60] YANG J, SHI G, BEI J, et al. Fabrication and surface modification of macroporous poly(L-lactic acid) and poly(L-lactic-co-glycolic acid) (70/30) cell scaffolds for human skin fibroblast cell culture. J Biomed Mater Res. 2002;62(3):438-446. [61] TANG Y, WONG C, WANG H, et al. Three-dimensional tissue scaffolds from interbonded poly(e-caprolactone) fibrous matrices with controlled porosity. Tissue Eng Part C Methods. 2011;17:209-218. [62] BUTLER S, KOHLES S, THIELKE R, et al. Interstitial fluid flow in tendons or ligaments:a porous medium finite element simulation. Med Biol Eng Comput. 1997;35:742-746. [63] RNJAK-KOVACINA J, WISE S, LI Z, et al. Tailoring the porosity and pore size of electrospun synthetic human elastin scaffolds for dermal tissue engineering. Biomaterials. 2011;32:6729-6736. [64] MANDAL B, KUNDU S. Cell proliferation and migration in silk fibroin 3D scaffolds. Biomaterials. 2009;30:2956-2965. [65] GU B, PARK S, KIM M, et al. Fabrication of sonicated chitosan nanofiber mat with enlarged porosity for use as hemostatic materials. Carbohydr Polym. 2003;97:65-73. [66] MURPHY C, O’BRIEN F. Understanding the effect of mean pore size on cell activity in collageng lyco saminogly can scaffolds. Cell Adhes Migr. 2010;4:377-381. [67] SUSSMAN EM, HALPIN MC, MUSTER J, et al. Porous implants modulate healing and induce shifts in local macrophage polarization in the foreign body reaction. Ann Biomed Eng. 2014;42:1508-1516. [68] ARTEL A, MEHDIZADEH H, CHIU YC, et al. An agent-based model for the investigation of neovascularization within porous scaffolds. Tissue Eng Part A. 2011;17(17-18):2133-2141. [69] MURPHY CM, HAUGH MG, O’BRIEN FJ. The effect of mean pore size on cell attachment, proliferation and migration in collagen–glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials. 2010;31(3):461-466. [70] KUBOKI Y, JIN Q, TAKITA H. Geometry of carriers controlling phenotypic expression in BMP-induced osteogenesis and chondrogenesis. J Bone Joint Surg Am. 2001;83-A Suppl 1(Pt 2):S105-115. [71] XU MY, ZHANG HR, ZHANG L, et al. Peracetic Acid-Ethanol Processed Human Tendon Allograft: A Morphological, Biochemical, and Biomechanical Study In Vitro. Orthop Surg. 2021. doi: 10.1111/os.13030. [72] XU HH, SIMON JR CG. Fast setting calcium phosphate-chitosan scaffold: mechanical properties and biocompatibility. Biomaterials. 2005;26:1337-1348. [73] FREED LE, MARQUIS JC, NOHRIA A, et al. Neocartilage formation in vitro and in vivo using cells cultured on synthetic biodegradable polymers. J Biomed Mater Res. 1993;27:11-23. [74] CHEN TW, JIANG J, CHEN SY. Status and headway of the clinical application of artificial ligaments. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(1):15-26. [75] ITOI U, TAKATORI M, HYAKUSOKU H, et al. Comparison of readily available scaffolds for adipose tissue engineering using adipose-derived stem cells. J Plast Reconstr Aesthet Surg. 2010;63:858-864. [76] BIMAN BM, SUBHAS CK. Cell proliferation and migration in silk fibroin 3D scaffolds. Biomaterials. 2009;30(15):2956-2965. [77] EIVAZI ZADEH Z, SOLOUK A, SHAFIEIAN M, et al. Electrospun polyurethane/carbon nanotube composites with different amounts of carbon nanotubes and almost the same fiber diameter for biomedical applications. Mater Sci Eng C Mater Biol Appl. 2021;118:111403. [78] OLVERA D, SCHIPANI R, SATHY BN, et al. Electrospinning of highly porous yet mechanically functional microfibrillar scaffolds at the human scale for ligament and tendon tissue engineering. Biomed Mater. 2019;14:035016. [79] GUNER MB, DALGIC AD, TEZCANER A, et al. A dual-phase scaffold produced by rotary jet spinning and electrospinning for tendon tissue engineering. Biomed Mater. 2020;15:065014. [80] JAMES R, KESTURU G, BALIAN G, et al. Tendon:biology, biomechanics, repair, growth factors, and evolving treatment options. J Hand Surg Am. 2008;33(1):102-112. [81] CHEN J, XU J, WANG A, et al. Scaffolds fortendonand ligament repair: review of the efficacy ofcommercial products. Expert Rev Med Devices. 2009;6(1):61-73. [82] BAYER ML, SCHJERLING P, HERCHENHAN A, et al. Release of tensile strain on engineered human tendon tissue disturbs cell adhesions, changes matrix architecture,and induces an inflammatory phenotype. PLoS One. 2014;9(1):86078. [83] MATHEW B, SARAH S, STEPHANIE D. Augmenting endogenous repair of soft tissues with nanofibre scaffolds. J R Soc Interface. 2018;15(141):20180019. [84] NELLY AP, EVAN LF, LOUIS JS. Tendon basic science: Development, repair, regeneration, and healing. J Orthop Res. 2015;33(6):780-784. |
| [1] | Xu Rong, Wang Haojie, Geng Mengxiang, Meng Kai, Wang Hui, Zhang Keqin, Zhao Huijing. Research advance in preparation and functional modification of porous polytetrafluoroethylene artificial blood vessels [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 759-765. |
| [2] | Cheng Jinhui, Wu Quan, Peng Min, Huang Changli, Tian Huimin, Li Yang. Preparation and properties of selective laser melting of porous titanium at a low energy density [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 664-668. |
| [3] | Xu Xiaodong, Zhou Jiping, Zhang Qi, Feng Chen, Zhu Mianshun, Shi Hongcan. 3D printing process of gelatin/oxidized nanocellulose skin scaffold with high elastic modulus and high porosity [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 398-403. |
| [4] | Shang Xiaoke, Ma Zhanjun, Wen Peng, Wang Hao, Ma Shaowei, Hu Jianzhong, Li Jian, Zheng Jun, Li Qi. Disposal methods of allografts affect bone remodeling at the tendon-bone healing interface after canine anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(34): 5516-5522. |
| [5] | Wei Qin, Amanguli·Ruze, Chen Bingxin, Zhao Ling, Zhao Banghao, Jiang Tao, Zhang Chun, Li Zhiqiang, Gao Xiaoming, Duan Mingjun. Relaxin protects myocardial microvascular endothelial cells from hypoxia-reoxygenation injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(28): 4519-4524. |
| [6] | Wang Xu, Yang Tengyun, Xiong Bohan, Zhang Yaozhang, Lu Xiaojun, Long Dan, Zhao Daohong. Regeneration mechanism and problems of tissue engineering in rotator cuff tendon-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(18): 2928-2934. |
| [7] | Yang Shenglin, Pu Xingwei, Luo Chunshan, Yang Jianwen. Neuroprotective effects of tetrandrine preconditioning in rabbits with spinal cord ischemia-reperfusion injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1223-1227. |
| [8] | Wu Li, Huang Wei, Li Xuetao, Li Panpan, Zhang Kaihang, Shen Zhiyuan. Analysis of adhesion and permeability of bone scaffold with Voronoi architecture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(28): 4472-4476. |
| [9] | Meng Zengdong, Zhu Bin, Zhang Yanan, Luo Lilin, Zhang Yuqin. Mechanical properties and biocompatibility of porous ZnO/hydroxyapatite composites with different porosities [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(22): 3498-3504. |
| [10] | Yang Jiaojiao, Hu Ming, Li Yan, Xia Delin. Effect of hydroxyapatite three-dimensional scaffolds with different apertures on the biological properties of MC3T3-E1 cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(21): 3338-3344. |
| [11] | Li Yaoming, Jiang Hong, Shi Yongfang. Preparation and characterization of chitosan/polylactic acid/hydroxyapatite/polyvinyl alcohol composite bone scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(18): 2888-2893. |
| [12] | Liu Xiaolin, Liu Shutai, Han Xiaoqian, Mu Xinyue. Topical simvastatin administration in the treatment of periodontitis: effect of loading on sustained drug release system or biomaterial scaffold system [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(16): 2596-2601. |
| [13] | Ma Ziyue, Ju Xiaochen, Zhang Lei, Sun Rongxin. Tendon-bone healing in anterior cruciate ligament reconstruction with and without remnant preservation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 582-587. |
| [14] | Wang Qing, Weng Yiping, Liu Hongwei, Zhang Wen, Shi Qin, Zhang Runze, Jiang Junfeng, Wang Caimei. Three-dimensional printed porous titanium alloy scaffolds with different apertures in repair of femoral defects in rabbits: 600 μm aperture is more conducive to osseointegration [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(28): 4441-4446. |
| [15] | Hu Chaoran, Qiu Bing, Zhou Zhuxing, Yang Yang, Li Jia. In vitro biocompatibility of 3D printed polycaprolactone/nano-hydroxyapatite composite scaffold with bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2020, 24(4): 589-595. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||