Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (36): 5753-5759.doi: 10.3969/j.issn.2095-4344.1962
Previous Articles Next Articles
Intravenous and intraarticular tranexamic acid can reduce blood loss and inflammatory response during cemented posterior cruciate ligament-retaining unilateral total knee arthroplasty
- 1Department of Bone and Joint Surgery, the Third People’s Hospital of Hainan Province, Sanya 572000, Hainan Province, China; 2Department of Joint Surgery, the Second Xiangya Hospital of Central South University, Changsha 410000, Hunan Province, China
-
Online:2019-12-28Published:2019-12-28 -
Contact:Zhang Guoru, Master, Chief physician, Department of Bone and Joint Surgery, the Third People’s Hospital of Hainan Province, Sanya 572000, Hainan Province, China -
About author:Wu Xingyuan, Attending physician, Department of Bone and Joint Surgery, the Third People’s Hospital of Hainan Province, Sanya 572000, Hainan Province, China
CLC Number:
Cite this article
Wu Xingyuan, Zhang Guoru, Liu Tang, Zhou Caisheng. Intravenous and intraarticular tranexamic acid can reduce blood loss and inflammatory response during cemented posterior cruciate ligament-retaining unilateral total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(36): 5753-5759.
share this article

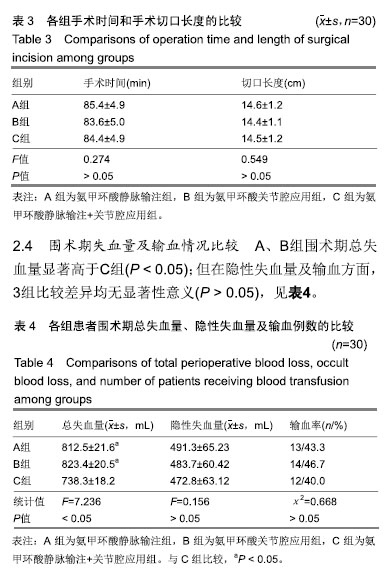
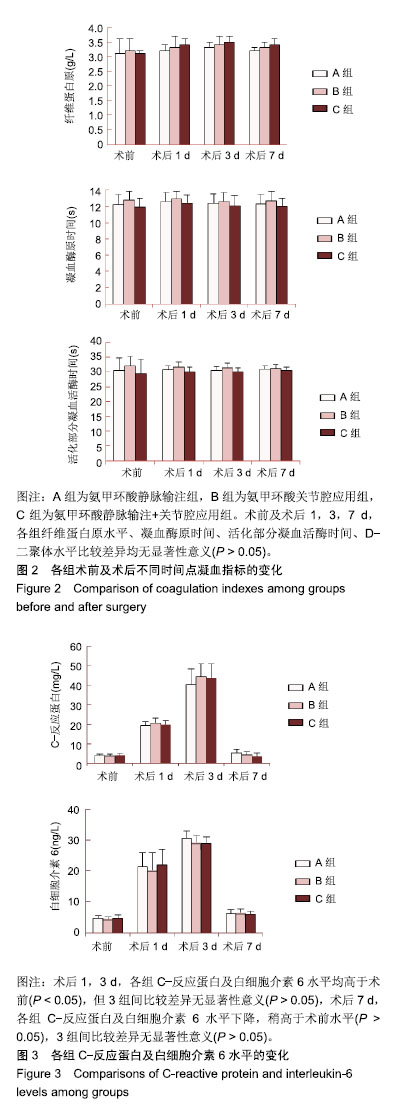
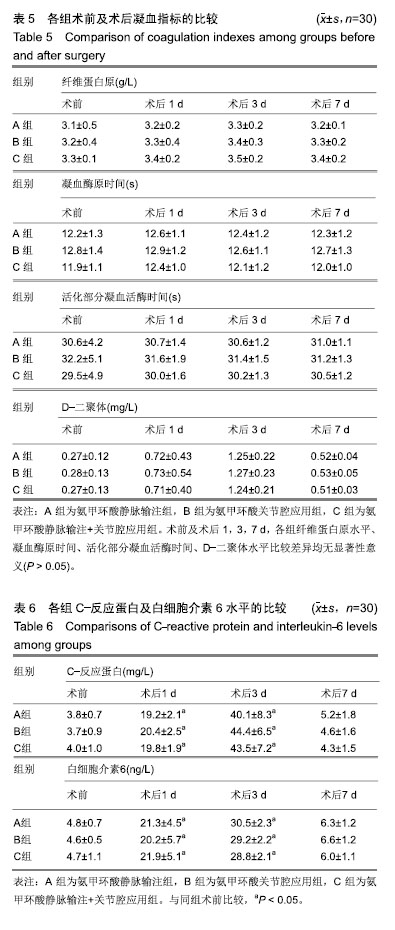
2.5 凝血功能比较 术前及术后1,3,7 d,各组纤维蛋白原水平、凝血酶原时间、活化部分凝血活酶时间、D-二聚体水平比较差异均无显著性意义(P > 0.05),见表5,图2。 2.6 炎性因子水平比较 术前,各组C-反应蛋白及白细胞介素6水平比较差异均无显著性意义(P > 0.05);术后1,3 d,各组C-反应蛋白及白细胞介素6水平均高于术前(P < 0.05),但3组间比较差异无显著性意义(P > 0.05),术后7 d,各组C-反应蛋白及白细胞介素6水平下降,稍高于术前水平(P > 0.05),3组间比较差异无显著性意义(P > 0.05),见表6,图3。 2.7 血栓发生情况 术后1周进行双下肢血管超声检查,显示3组患者均无深静脉血栓形成。随访6个月,3组均未出现下肢深静脉血栓及肺栓塞病例。 2.8 不良反应 3组患者术后切口均一期愈合,术后无感染病例出现,无血栓、恶心、呕吐及腹泻等氨甲环酸药物不良反应发生。"
| [1]Kim YH,Pandey K,Park JW,et al.Comparative Efficacy of Intravenous With Intra-articular Versus Intravenous Only Administration of Tranexamic Acid to Reduce Blood Loss in Knee Arthroplasty.Orthopedics.2018;41(6):e827-e830. [2]Wang F,Zhao KC,Zhao MM,et al.The efficacy of oral versus intravenous tranexamic acid in reducing blood loss after primary total knee and hip arthroplasty: A meta-analysis. Medicine(Baltimore). 2018;97(36):e12270. [3]Han YH, Huang HT, Pan JK, et al. Is the combined application of both drain-clamping and tranexamic acid superior to the single use of either application in patients with total-knee arthroplasty?: A meta-analysis of randomized controlled trials. Medicine(Baltimore).2018;97(36):e11573. [4]Xiong H,Liu Y,Zeng Y,et al.The efficacy and safety of combined administration of intravenous and topical tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled trials.BMC Musculoskelet Disord.2018;19(1):321. [5]彭慧明,翁习生,翟吉良,等.氨甲环酸结合术后引流管临时夹闭降低单侧全膝置换术后失血量的有效性及安全性[J].中华骨科杂志,2014,34(4):400-405.[6]Li H,Bai L,Li Y,et al.Oral tranexamic acid reduces blood loss in total-knee arthroplasty: A meta-analysis.Medicine (Baltimore). 2018;97(45):e12924.[7]Wu YG,Zeng Y,Hu QS,et al.Tranexamic Acid Plus Low-dose Epinephrine Reduces Blood Loss in Total Knee Arthroplasty: A Systematic Review and Meta-analysis.Orthop Surg. 2018; 10(4):287-295. [8]Almeida MDC,Albuquerque RPE,Palhares GM,et al. Evaluation of the use of tranexamic acid in total knee arthroplasty.Rev Bras Ortop.2018;53(6):761-767.[9]Cao G,Xie J,Huang Z,et al.Efficacy and safety of multiple boluses of oral versus intravenous tranexamic acid at reducing blood loss after primary total knee arthroplasty without a tourniquet: A prospective randomized clinical trial. Thromb Res.2018;171:68-73. [10]Wang D,Wang HY,Luo ZY,et al.Blood-conserving efficacy of multiple doses of oral tranexamic acid associated with an enhanced-recovery programme in primary total knee arthroplasty: a randomized controlled trial.Bone Joint J. 2018;100-B(8):1025-1032.[11]Kim YT, Kang MW, Lee JK, et al.Combined use of topical intraarticular tranexamic acid and rivaroxaban in total knee arthroplastysafely reduces blood loss, transfusion rates, and wound complications without increasing the risk of thrombosis. BMC Musculoskelet Disord.2018;19(1):227.[12]Grant AL,Letson HL,Morris JL,et al.Tranexamic acid is associated with selective increase in inflammatory markers following total knee arthroplasty (TKA): a pilot study.J Orthop Surg Res. 2018;13(1):149. [13]Li R,Yin S,Zhong H,et al.[Effect on time of temporarily-closed wound drainage on blood loss of primary total knee arthroplasty after intravenous and intra-articular injection of tranexamic acid]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31(4):417-421.[14]Guo P,He Z,Wang Y,et al.Efficacy and safety of oral tranexamic acid in total knee arthroplasty: A systematic review and meta-analysis.Medicine(Baltimore). 2018;97(18): e0587. [15]李大坤,高忠,邢刚,等.局部应用与静脉注射氨甲环酸减少全髋关节置换术术后失血量有效性与安全性的研究[J].中国骨与关节损伤杂志,2016,31(8):843-844.[16]Yozawa S,Ogawa H,Matsumoto K,et al.Periarticular injection of tranexamic acid reduces blood loss and the necessity for allogeneic transfusion after total knee arthroplasty using autologous transfusion: a retrospective observational study.J Arthroplasty.2018;33(1):86-89.doi: 10.1016/j.arth.2017.08.018. [17]Abdel MP,Chalmers BP,Taunton MJ,et al.Intravenous versus topical tranexamic acid in total knee arthroplasty: both effective in a randomized clinical trial of 640 patients. J Bone Joint Surg Am. 2018;100(12):1023-1029.[18]马瑞,杨佩,王春生,等.不同氨甲环酸给药途径在全膝关节置换术的有效性和安全性[J].中华关节外科杂志(电子版), 2018,12(5): 666-670.[19]高麟超.氨甲环酸的三种给药途径在全膝关节置换术中的有效性及安全性的对比研究[D].宁波:宁波大学,2016.[20]Sun Q,Li J,Chen J,et al.Comparison of intravenous, topical or combined routes of tranexamic acid administration in patients undergoing total knee and hip arthroplasty: a meta-analysis of randomised controlled trials.BMJ Open.2019;9(1):e024350. [21]Jimenez JJ,Iribarren JL,Lorente L,et al.Tranexamic acid attenuates inflammatory response in cardiopulmonary bypass surgery through blockade of fibrinolysis: a case control study followed by a randomized double-blind controlled trial.Crit Care.2007;11(6):R117.[22]Hu Y,Li Q,Wei BG,et al.Blood loss of total knee arthroplasty in osteoarthritis: an analysis of influential factors.J Orthop Surg Res.2018;13(1):325.[23]Li ZJ,Zhao MW,Zeng L.Additional Dose of Intravenous Tranexamic Acid after Primary Total Knee Arthroplasty Further Reduces Hidden Blood Loss.Chin Med J (Engl). 2018; 131(6):638-642. [24]Mufarrih SH,Malik AT,Qureshi NQ,et al.The effect of tranexamic acid in unilateral and bilateral total knee arthroplasty in the South Asian population: A retrospective cohort study.Int J Surg.2018;52:25-29.[25]Subramanyam KN,Khanchandani P,Tulajaprasad PV,et al.Efficacy and safety of intra-articular versus intravenous tranexamic acid in reducing perioperative blood loss in total knee arthroplasty: a prospective randomized double-blind equivalence trial.Bone Joint J.2018;100-B(2):152-160. [26]Yuan X,Wang J,Wang Q,et al.Synergistic effects of intravenous and intra-articular tranexamic acid on reducing hemoglobin loss in revision total knee arthroplasty: a prospective, randomized, controlled study.Transfusion. 2018;58(4):982-988. [27]George J,Eachempati KK,Subramanyam KN,et al.The comparative efficacy and safety of topical and intravenous tranexamic acid for reducing perioperative blood loss in Total knee arthroplasty- A randomized controlled non-inferiority trial.Knee.2018;25(1):185-191.[28]Zhang LK,Ma JX,Kuang MJ,et al.The efficacy of tranexamic acid using oral administration in total knee arthroplasty: a systematic review and meta-analysis.J Orthop Surg Res. 2017;12(1):159. [29]Wang Z,Shen X.The efficacy of combined intra-articular and intravenous tranexamic acid for blood loss in primary total knee arthroplasty: A meta-analysis. Medicine (Baltimore). 2017 Oct;96(42):e8123. [30]Yen SH,Lin PC,Chen B,et al.Topical Tranexamic Acid Reduces Blood Loss in Minimally Invasive Total Knee Arthroplasty Receiving Rivaroxaban.Biomed Res Int. 2017; 2017:9105645.[31]Wang D,Zhu H,Meng WK,et al.Comparison of oral versus intra-articular tranexamic acid in enhanced-recovery primary total knee arthroplasty without tourniquet application: a randomized controlled trial. BMC Musculoskelet Disord.2018;19(1):85. |
| [1] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [2] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [3] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [4] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [5] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [6] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [7] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [8] | Ma Rui, Wang Jialin, Wu Mengjun, Ge Ying, Wang Wei, Wang Kunzheng. Relationship of pathogenic bacteria distribution with drug resistance and treatment cycle for periprosthetic joint infection after total joint arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 380-385. |
| [9] | Lü Zexiang, Wu Jutai, Jiang Jian, Feng Xiao, Li Tengfei, Wang Yehua. Effect of tranexamic acid combined with carbazochrome sodium sulfonate on blood loss and safety after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 386-390. |
| [10] | Hu Shouye, Yang Zhi, Hao Yangquan, Lu Chao, Zhang Qiong, Zhang Weisong, Zhu Yujie, Peng Kan. Tourniquet use in the first half-course of total knee arthroplasty does not affect postoperative functional outcomes or pain: a prospective, randomized controlled trial [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4327-4332. |
| [11] | He Shengcai, Jiang Chengdan, Jing Chunxiang, Luo Minyi, Ma Xingfa, Li Jiazhou, Pan Huashan. Values of alpha defensin and C-reactive protein in synovial fluid in the diagnosis of periprosthetic infection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4344-4347. |
| [12] | Kang Bo, Wang Jindong. Development status and strategy of outpatient total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4408-4414. |
| [13] | Wang Hao, Wang Yitao, Lü Zexiang, Li Tengfei, Wang Shaolong, Wang Yehua. Effect of repeated intravenous tranexamic acid in the perioperative period of proximal femoral nail antirotation for femoral intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3319-3323. |
| [14] | Deng Zhibo, Li Zhi, Wu Yahong, Mu Yuan, Mu Yuexi, Yin Liangjun. Local infiltration anesthesia versus femoral nerve block for pain control and safety after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3401-3408. |
| [15] | Jiang Shengyuan, Li Dan, Jiang Jianhao, Shang-you Yang, Yang Shuye. Biological response of Co2+ to preosteoblasts during aseptic loosening of the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3292-3299. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||