Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (36): 5747-5752.doi: 10.3969/j.issn.2095-4344.1894
Previous Articles Next Articles
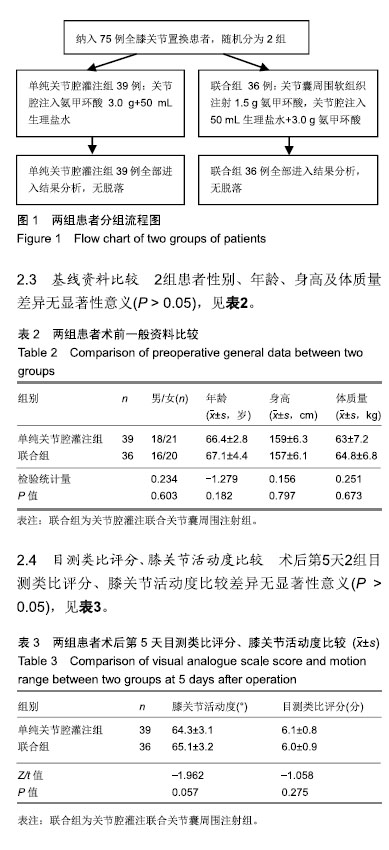
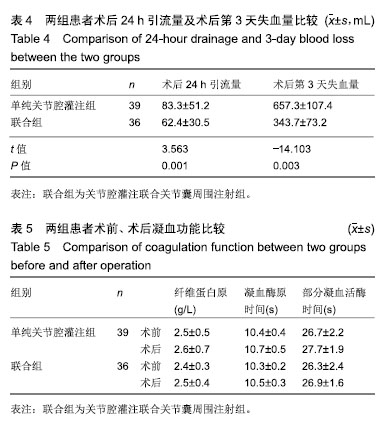
Relationship between intra-articular infusion combined with peri-articular injection of tranexamic acid and postoperative blood loss after total knee arthroplasty
- 1Guizhou Medical University, Guiyang 550001, Guizhou Province, China; 2Guizhou Provincial People’s Hospital, Guiyang 550002, Guizhou Province, China; 3GYBY Cardiovascular Disease Hospital, Guiyang 550014, Guizhou Province, China
-
Online:2019-12-28Published:2019-12-28 -
Contact:Sun Li, MD, Chief physician, Guizhou Provincial People’s Hospital, Guiyang 550002, Guizhou Province, China -
About author:Bao Hongbo, Attending physician, Guizhou Medical University, Guiyang 550001, Guizhou Province, China -
Supported by:the National Natural Science Foundation of China, No. 81560356 (to TXB)| the Guizhou Science and Technology Plan, No. (2019)1429 (to SL)
CLC Number:
Cite this article
Bao Hongbo, Sun Li, Tian Xiaobin, Chen Long, Li Senlei, Yang Xianteng, Wang Shaobin, Cai Jian. Relationship between intra-articular infusion combined with peri-articular injection of tranexamic acid and postoperative blood loss after total knee arthroplasty[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(36): 5747-5752.
share this article
| [1] | Wang H, Shen B, Zeng Y. Comparison of topical versus intravenous tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled and prospective cohort trials. Knee.2014;21:987-993. |
| [2] | Legnani C, Oriani G, Parente F , et al.Reducing transfusion requirements following total knee arthroplasty: effectiveness of a double infusion of tranexamic acid. Eur Rev Med Pharmacol Sci.2019;23:2253-2256. |
| [3] | Tang Y, Wen Y, Li W, et al. The efficacy and safety of multiple doses of oral tranexamic acid on blood loss, inflammatory and fibrinolysis response following total knee arthroplasty: A randomized controlled trial. Int J Surg.2019;65:45-51. |
| [4] | Chen TP, Chen YM, Jiao JB, et al. Comparison of the effectiveness and safety of topical versus intravenous tranexamic acid in primary total knee arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res.2017; 2:11. |
| [5] | Zhang YM, Yang B, Sun XD, et al.Combined intravenous and intra-articular tranexamic acid administration in total knee arthroplasty for preventing blood loss and hyperfibrinolysis: A randomized controlled trial. Medicine (Baltimore).2019;98: e14458. |
| [6] | Zhang LK, Ma JX, Kuang MJ, et al. The efficacy of tranexamic acid using oral administration in total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2017;12:159. |
| [7] | Meftah M, White PB, Siddiqi A , et al. Tranexamic acid reduces transfusion rates in obese patients undergoing total joint arthroplasty. Surg Technol Int.2019;34:451-455. |
| [8] | Lum ZC, Manoukian MAC, Pacheco CS , et al. Intravenous tranexamic acid versus topical aminocaproic acid: which method has the least blood loss and transfusion rates? J Am Acad Orthop Surg Glob Res Rev. 2018;2:e072. |
| [9] | Yozawa S, Ogawa H, Matsumoto K , et al. Periarticular injection of tranexamic acid reduces blood loss and the necessity for allogeneic transfusion after total knee arthroplasty using autologous transfusion: a retrospective observational study. J Arthroplasty.2018;33:86-89. |
| [10] | Phan DL, Rinehart JB, Ran S. Can tranexamic acid change preoperative anemia management during total joint arthroplasty? World J Orthop. 2015; 6:521. |
| [11] | Lin ZX, Woolf SK. Safety, efficacy, and cost-effectiveness of tranexamic acid in orthopedic surgery. Orthopedics. 2016; 39: 119-130. |
| [12] | Mahringer-Kunz A, Efe T, Fuchs-Winkelmann S, et al. Bleeding in TKA: posterior stabilized vs. cruciate retaining. Arch Orthop Trauma Surg. 2015; 135: 867-870. |
| [13] | Ricket AL, Stewart DW, Wood RC , et al. Comparison of postoperative bleeding in tha and tka patients receiving rivaroxaban or enoxaparin. Ann Pharmacother. 2016;50(4): 270-275. |
| [14] | Sun Q, Li J, Chen J , et al. Comparison of intravenous, topical or combined routes of tranexamic acid administration in patients undergoing total knee and hip arthroplasty: a meta-analysis of randomised controlled trials. BMJ Open. 2019; 9:e024350. |
| [15] | Grant AL, Letson HL, Morris JL, et al. Tranexamic acid is associated with selective increase in inflammatory markers following total knee arthroplasty (TKA): a pilot study. J Orthop Surg Res.2018;13:149. |
| [16] | Laoruengthana A, Rattanaprichavej P, Rasamimongkol S, et al. Intra-articular tranexamic acid mitigates blood loss and morphine use after total knee arthroplasty. A randomized controlled trial. J Arthroplasty. 2019;34(5):877-881. |
| [17] | 雷金来,丛雨轩,庄岩,等.术前应用氨甲环酸对股骨近端防旋髓内钉固定治疗股骨转子间骨折隐性失血的影响[J].中华创伤骨科杂志,2017,19(2): 103-108. |
| [18] | 鲍航行,朱磊,张佳颖,等.不放置引流管结合局部灌注TXA对全膝关节置换术后出血量的影响[J].浙江临床医学,2018,20(3): 464-465. |
| [19] | 郭焕来,杨建祥,赵杰,等.重复使用氨甲环酸对TKA术后失血量及安全性的影响[J].创伤外科杂志,2017,19(9): 681-684. |
| [20] | Hill J, Magill P, Dorman A, et al. Assessment of the effect of addition of 24 hours of oral tranexamic acid post-operatively to a single intraoperative intravenous dose of tranexamic acid on calculated blood loss following primary hip and knee arthroplasty (TRAC-24): a study protocol for a randomised controlled trial. Trials.2018;19: 413. |
| [21] | Wang D, Wang HY, Luo ZY, et al. Blood-conserving efficacy of multiple doses of oral tranexamic acid associated with an enhanced-recovery programme in primary total knee arthroplasty: a randomized controlled trial. Bone Joint J. 2018;100-B(8):1025-1032. |
| [22] | Kim YT, Kang MW, Lee JK, et al. Combined use of topical intraarticular tranexamic acid and rivaroxaban in total knee arthroplasty safely reduces blood loss, transfusion rates, and wound complications without increasing the risk of thrombosis. BMC Musculoskelet Disord. 2018;19: 227. |
| [23] | Wilde JM, Copp SN, McCauley JC, et al. One Dose of Intravenous Tranexamic Acid Is Equivalent to Two Doses in Total Hip and Knee Arthroplasty. J Bone Joint Surg Am. 2018; 100: 1104-1109. |
| [24] | Alshryda S, Sukeik M, Sarda P, et al. A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J. 2014; 96-B: 1005-1015. |
| [25] | Xie J, Hu Q, Huang Q, et al. Comparison of intravenous versus topical tranexamic acid in primary total hip and knee arthroplasty: An updated meta-analysis. Thromb Res. 2017; 153: 28-36. |
| [26] | 包洪波,田晓滨,孙立等.局部使用不同浓度氨甲环酸对全膝关节置换术后失血量影响的临床随机对照研究[J].中华创伤骨科杂志,2016,18(5):407-411. |
| [27] | 张权,孙立,杨先腾等. 关节腔内使用氨甲环酸对全膝关节置换术后失血量的影响及安全性评估[J].中华创伤骨科杂志,2015, 17(5): 395-398. |
| [28] | Kim C, Park SS, Davey JR. Tranexamic acid for the prevention and management of orthopedic surgical hemorrhage: current evidence. J Blood Med. 2015; 6: 239-244. |
| [29] | Adigweme OO, Lee GC. Tranexamic acid: the new gold standard? Tech Orthop. 2017; 32:17-22. |
| [30] | Dorweiler MA, Boin MA, Froehle AW, et al. Improved early postoperative range of motion in total knee arthroplasty using tranexamic acid: a retrospective analysis. J Knee Surg. 2019; 32(2):160-164. |
| [1] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [2] | Wang Jinjun, Deng Zengfa, Liu Kang, He Zhiyong, Yu Xinping, Liang Jianji, Li Chen, Guo Zhouyang. Hemostatic effect and safety of intravenous drip of tranexamic acid combined with topical application of cocktail containing tranexamic acid in total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1356-1361. |
| [3] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [4] | Yuan Jun, Yang Jiafu. Hemostatic effect of topical tranexamic acid infiltration in cementless total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 873-877. |
| [5] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Intravenous, topical tranexamic acid alone or their combination in total knee arthroplasty: a meta-analysis of randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 948-956. |
| [6] | Zhan Fangbiao, Cheng Jun, Zou Xinsen, Long Jie, Xie Lizhong, Deng Qianrong. Intraoperative intravenous application of tranexamic acid reduces perioperative bleeding in multilevel posterior spinal surgery: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 977-984. |
| [7] | Zhao Zhongyi, Li Yongzhen, Chen Feng, Ji Aiyu. Comparison of total knee arthroplasty and unicompartmental knee arthroplasty in treatment of traumatic osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 854-859. |
| [8] | Lü Zexiang, Wu Jutai, Jiang Jian, Feng Xiao, Li Tengfei, Wang Yehua. Effect of tranexamic acid combined with carbazochrome sodium sulfonate on blood loss and safety after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 386-390. |
| [9] | Hu Shouye, Yang Zhi, Hao Yangquan, Lu Chao, Zhang Qiong, Zhang Weisong, Zhu Yujie, Peng Kan. Tourniquet use in the first half-course of total knee arthroplasty does not affect postoperative functional outcomes or pain: a prospective, randomized controlled trial [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4327-4332. |
| [10] | Kang Bo, Wang Jindong. Development status and strategy of outpatient total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(27): 4408-4414. |
| [11] | Mieralimu•Muertizha, Ainiwaerjiang•Damaola, Lin Haishan, Wang Li . Relationship between tibio-femoral mechanical axis deviation on coronal plane and early joint function recovery after total knee arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3300-3304. |
| [12] | Wang Hao, Wang Yitao, Lü Zexiang, Li Tengfei, Wang Shaolong, Wang Yehua. Effect of repeated intravenous tranexamic acid in the perioperative period of proximal femoral nail antirotation for femoral intertrochanteric fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3319-3323. |
| [13] | Deng Zhibo, Li Zhi, Wu Yahong, Mu Yuan, Mu Yuexi, Yin Liangjun. Local infiltration anesthesia versus femoral nerve block for pain control and safety after total knee arthroplasty: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(21): 3401-3408. |
| [14] | Deng Bo, Hong Hainan, Fan Yongyong, Cai Guoping, Feng Xingbing, Hong Zhenghua. Efficacy and safety of tourniquet application in total knee arthroplasty and only at the time of cementing: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2908-2914. |
| [15] | Huang Chenyu, Tang Cheng, Wei Bo, Li Jiayi, Li Xuxiang, Zhang Huikang, Xu Yan, Yao Qingqiang, Wang Liming. Application of three-dimensional printing guide plate in total knee arthroplasty for patients with varus and valgus deformity [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(18): 2789-2793. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||