Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (6): 827-832.doi: 10.3969/j.issn.2095-4344.1558
Previous Articles Next Articles
Effect of high-viscosity cement dispersion on the treatment of osteoporotic vertebral compression fracture in elderly women
Chen Cheng1, Zhang Jiyun2, Hao Jie1, Wu Gang2, Zhang Feng1, Chen Xiaoqing1
- 1Affiliated Hospital of Nantong University, Nantong 226001, Jiangsu Province, China; 2Nantong Third Hospital of Nantong University, Nantong 226000, Jiangsu Province, China
-
Received:2018-10-20Online:2019-02-28Published:2019-02-28 -
Contact:Chen Xiao-qing, MD, Associate chief physician, Affiliated Hospital of Nantong University, Nantong 226001, Jiangsu Province, China -
About author:Chen Cheng, Master, Physician, Affiliated Hospital of Nantong University, Nantong 226001, Jiangsu Province, China -
Supported by:the Nantong Municipal Science and Technology Project, No. MS22015109 (to CXQ)
CLC Number:
Cite this article
Chen Cheng, Zhang Jiyun, Hao Jie, Wu Gang, Zhang Feng, Chen Xiaoqing. Effect of high-viscosity cement dispersion on the treatment of osteoporotic vertebral compression fracture in elderly women[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(6): 827-832.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
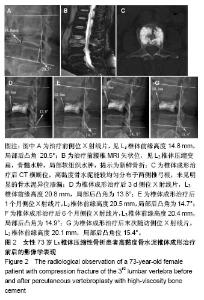
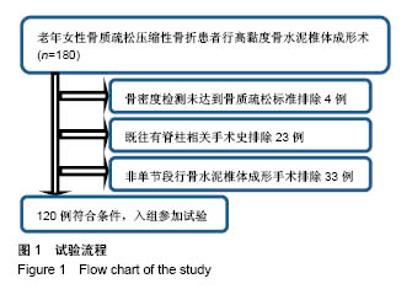
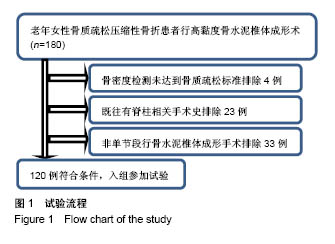
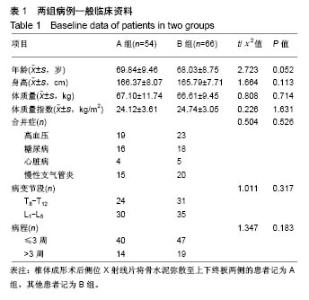
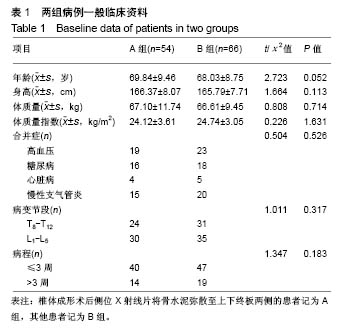
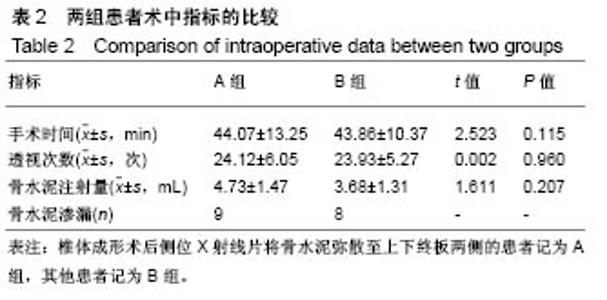
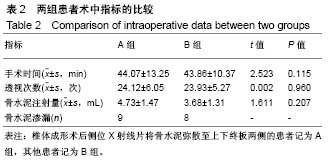
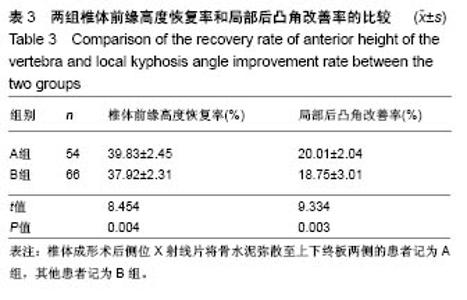
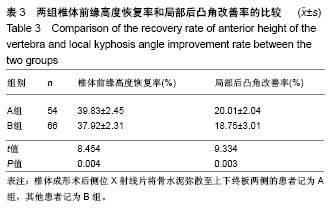
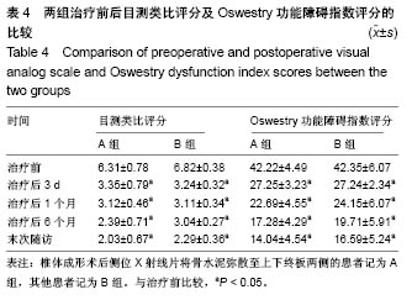
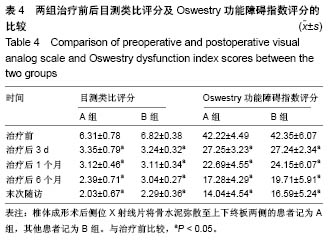
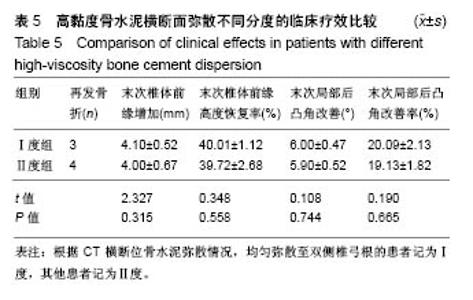
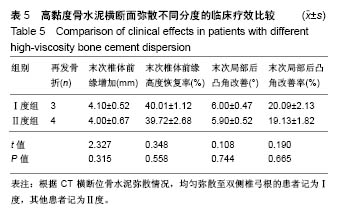
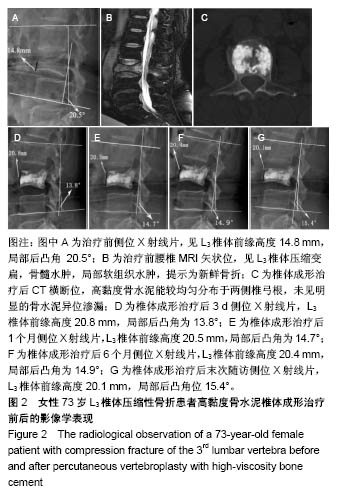
2.5 典型病例 73岁女性L3椎体压缩性骨折患者,行高黏度骨水泥椎体成形治疗前后影像学表现,见图2。图2C,D显示椎体成形后侧位X射线中高黏度骨水泥可有效弥散至上下终板,且CT横断位上显示能有效弥散至双侧椎弓根,故该病例属于A组Ⅰ度。治疗后3 d椎体前缘高度(高度增加6.0 mm)及局部后凸角(Cobb角减少6.7°)有明显改善,且术后随访各时间点显示椎体前缘高度及局部后凸角维持较好,未见高度明显丢失及局部后凸角增加等不良情况发生。 2.6 不良反应 A组患者中骨水泥渗漏9例,术后发热4例,低血压2例;B组患者中骨水泥渗漏8例,发热6例,术后血压升高2例,术后皮肤浅层渗液1例,两组并发症发生情况比较差异无显著性意义(P > 0.05)。32例患者予以对症处理后均获得改善,未出现其他严重血管栓塞及神经损伤等的手术相关并发症。 2.7 可能影响因素 此次研究也存在一些不足之处:第一,研究没有考虑到其他影响椎体中骨水泥弥散分布的因素,如骨折时间等,结论存在偏差;第二,研究纳入的病例数较少,且研究病例中均未发生严重的并发症,故对并发症研究不足;第三,研究方法采用非盲法,因此在病例收集、分析等方面存在一定的偏倚。"
| [1] 李祖浩,王辰宇,王中汉,等.骨质疏松性骨缺损的治疗进展: 支架植入与局部药物递送[J].中国组织工程研究, 2018,22(18): 2939-2945.[2] Anne RC, Dolores MS. Osteoporosis Therapy in Postmenopausal Women with High Risk of Fracture. JAMA. 2016;316(7):715-716.[3] 刘韵婷,郭辉,张一民.骨骼肌含量、身体活动水平与骨密度的相关性[J].中国组织工程研究,2018,22(16): 2478-2482.[4] Orchard T,Yildiz V,Steck SE,et al. Dietary Inflammatory Index, Bone Mineral Density, and Risk of Fracture in Postmenopausal Women: Results from the Women's Health Initiative. J Bone Miner Res. 2017; 32(5):1136-1146.[5] Yang EZ, Xu JG, Huang GZ, et al. Percutaneous Vertebroplasty Versus Conservative Treatment in Aged Patients With Acute Osteoporotic Vertebral Compression Fractures: A Prospective Randomized Controlled Clinical Study.Spine(Phila Pa 1976). 2016;41(8):653-660.[6] 林玉江,林茜,杨利民,等.弯角椎体成形术治疗胸腰椎骨质疏松性椎体压缩骨折的疗效分析[J].中国脊柱脊髓杂志,2017,27(5): 423-428.[7] Corcos G,Dbjay J,Mastier C,et al.Cement leakage in Percutaneous vertebroplasty for Spinal metastases: a retrospective evaluation of incidence and risk factors. Spine (Phila Pa 1976). 2014; 39(5): E332-E338.[8] 邹向南.高粘度骨水泥椎体成形术治疗骨质疏松性椎体压缩骨折的椎体高度恢复情况及相关影响因素[J]. 中国脊柱脊髓杂志, 2017,27(11): 991-996.[9] 何涛,杨定焯,刘忠厚.骨质疏松症诊断标准的探讨[J].中国骨质疏松杂志, 2010,16(2):151-156,104.[10] 杜桂迎,余卫,林强,等.WHO双能X线吸收仪骨质疏松症诊断标准及其相关问题[J].中华骨质疏松和骨矿盐疾病杂志, 2016,9(3): 330-338.[11] 朱敏,李玉前,王晓东,等.椎体成形中病椎内骨水泥弥散与骨折时间的关系[J].中国组织工程研究, 2015,19(52):8391-8395.[12] 李全修,陈晓东,梁鹏展,等.椎体成形术后相邻椎体骨折患者脊柱矢状面参数变化及其临床意义[J].中国骨与关节损伤杂志, 2017, 32(5):464-467.[13] 周毅,海涌,苏庆军,等.影响椎体后凸成形术椎体高度恢复的相关因素及临床意义[J].中国骨与关节外科, 2011,4(4):288-293.[14] Phillips FM,Ho E,Campbell Hupp M,et al.Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fracture.Spine J. 2003; 28(19):2260-2265.[15] Joyce CR,Zutshi DW,Hrubes V,et al.Comparison of fixed interval and visual analogue scales for rating chronic pain.Eur J Clin Pharmacol. 1975;8(6):415-420.[16] Roland M, Fairbank J. The Roland Morris disability questionnaire and the Oswestry disability questionnaire. Spine (Phila Pa 1976). 2000;25(24):3115-3124.[17] 曾森炎,季卫锋,董玉鹏,等.高粘度与低粘度骨水泥PVP治疗骨质疏松性椎体压缩骨折的Meta分析[J].中国骨与关节损伤杂志, 2018, 33(3):240-243.[18] 张晓刚,赵希云,宋敏,等.骨质疏松性椎体压缩骨折的生物力学研究进展[J].医用生物力学,2017,32(2): 199-204.[19] 朱智敏,钟华,黄艳,等.PVP治疗骨质疏松性椎体压缩骨折预防相邻椎体骨折的随机对照研究[J].中国骨与关节损伤杂志, 2016, 31(9):919-922.[20] 车晓明,陈亮,顾勇,等.茶多酚治疗骨质疏松症的研究进展[J].中国骨质疏松杂志,2015,21(2):235-240.[21] Ohtori S,Inoue G,Orita S,et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective.Spine(Phila Pa 1976). 2013;38(8):E487-E492.[22] 吕晓双,王晓丽,孙侃,等.老年女性血HCY水平与骨密度的相关性研究[J].中国骨质疏松杂志,2018,24(4): 454-457.[23] Hansen EJ,Simony A,Carreon L,et al. Rate of Unsuspected Malignancy in Patients With Vertebral Compression Fracture Undergoing Percutaneous Vertebroplasty.Spine(Phila Pa 1976). 2016;41(6): 549-552.[24] Takahara K,Kamimura M,Moriya H,et al.Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women.BMC Musculoskelet Disord.2016;17:12.[25] 杨惠林,刘昊,殷国勇,等.我国经皮椎体后凸成形术治疗骨质疏松性椎体骨折现状与创新[J].中华骨质疏松和骨矿盐疾病杂志, 2017,10(1):12-19.[26] 盛朝辉,李田珂,王健军,等.单侧与双侧穿刺后凸成形术治疗骨质疏松性胸腰椎骨折的比较[J].中国矫形外科杂志, 2018,26(12): 1094-1097.[27] 张彤童,任龙喜,郭函,等.高粘度骨水泥椎体成形术在骨质疏松性椎体压缩性骨折中临床应用价值研究[J].创伤与急危重病医学, 2018,6(2):71-74.[28] Zhang ZF,Huang H,Chen S,et al.Comparison of high- and low-viscosity cement in the treatment of vertebral compression fractures: A systematic review and meta-analysis. Medicine. 2018;97(12): e0184.[29] Chevalier Y,Pahr D,Charlebois M,et al.Cement distributin, volume, and compliance in vertebroplasty: some answers from an anatomy-based nonlinear finite element study. Spine(Phila Pa 1976). 2008;33(16):1722-1730.[30] 田伟,韩骁,刘波,等.经皮椎体后凸成形术后骨水泥分布与手术椎体再骨折的关系[J].中华创伤骨科杂志, 2012,14(3):211-215.[31] 唐冲,吴四军,刘正,等.高粘度骨水泥在单侧经皮椎体成形术中的弥散分布特点[J].实用骨科杂志,2017, 23(10):884-887.[32] 余博臣,张亮,高梁斌.PVP/PKP术后手术椎体再发骨折的研究进展[J].中国脊柱脊髓杂志,2012,22(2): 183-185.[33] 李亮,聂艳,姜保恩,等.经皮椎体成形术后手术椎体再发骨折的相关因素分析[J].实用骨科杂志,2014, 20(4):339-343.[34] 梅贤忠,刘修华,甘学文,等.椎体成形术中高粘度骨水泥与普通骨水泥渗漏的比较[J].中国中医骨伤科杂志,2017,25(6):57-60.[35] 王想福,范有福,石瑞芳,等.单侧穿刺椎体后凸成形术骨水泥分布与穿刺角度的关系[J].中国骨伤,2015, 28(8):704-707.[36] Steinmann J,Tingey CT,Cruz G,et al.Biomechanical comparison of unipedicular versus bipedicular kyphoplasty. Spine(Phila Pa 1976). 2005;30(2):201-205.[37] 左华,黄永辉,李大鹏,等.经皮椎体成形术及经皮后凸成形术治疗老年骨质疏松性椎体压缩性骨折的长期临床疗效比较[J].中国矫形外科杂志, 2015,23(22):2021-2025. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [3] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [4] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [5] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [6] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [7] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [8] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [9] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [10] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [11] | Zhong Yuanming, Wan Tong, Zhong Xifeng, Wu Zhuotan, He Bingkun, Wu Sixian. Meta-analysis of the efficacy and safety of percutaneous curved vertebroplasty and unilateral pedicle approach percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 456-462. |
| [12] | Feng Guancheng, Fang Jianming, Lü Haoran, Zhang Dongsheng, Wei Jiadong, Yu Bingbing. How does bone cement dispersion affect the early outcome of percutaneous vertebroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3450-3457. |
| [13] | Chen Siqi, Xian Debin, Xu Rongsheng, Qin Zhongjie, Zhang Lei, Xia Delin. Effects of bone marrow mesenchymal stem cells and human umbilical vein endothelial cells combined with hydroxyapatite-tricalcium phosphate scaffolds on early angiogenesis in skull defect repair in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3458-3465. |
| [14] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [15] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||