Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (15): 2444-2452.doi: 10.3969/j.issn.2095-4344.2017.15.026
Previous Articles Next Articles
Mid- and long-term outcomes of cervical disc arthroplasty versus anterior cervical discectomy and fusion for single-level cervical spondylosis: a meta-analysis
Chen Bo1, Qu Xia2, Tao Yuan1, Luo Cheng1, Yang Lin1, Zou Yong-gen1
- 1Department of Traumatic Orthopedics, 2Department of Nephropathy, Traditional Chinese Medicine Hospital Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China
-
Online:2017-05-28Published:2017-06-07 -
Contact:Zou Yong-gen, Department of Traumatic Orthopedics, Traditional Chinese Medicine Hospital Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China -
About author:Chen Bo, Master, Attending physician, Department of Traumatic Orthopedics, Traditional Chinese Medicine Hospital Affiliated to Southwest Medical University, Luzhou 646000, Sichuan Province, China
CLC Number:
Cite this article
Chen Bo, Qu Xia, Tao Yuan, Luo Cheng, Yang Lin, Zou Yong-gen. Mid- and long-term outcomes of cervical disc arthroplasty versus anterior cervical discectomy and fusion for single-level cervical spondylosis: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(15): 2444-2452.
share this article

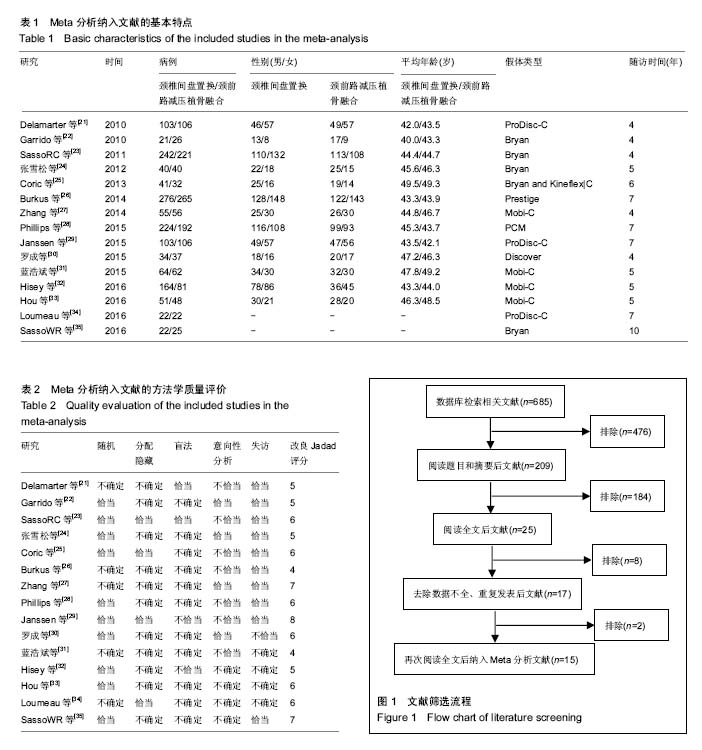
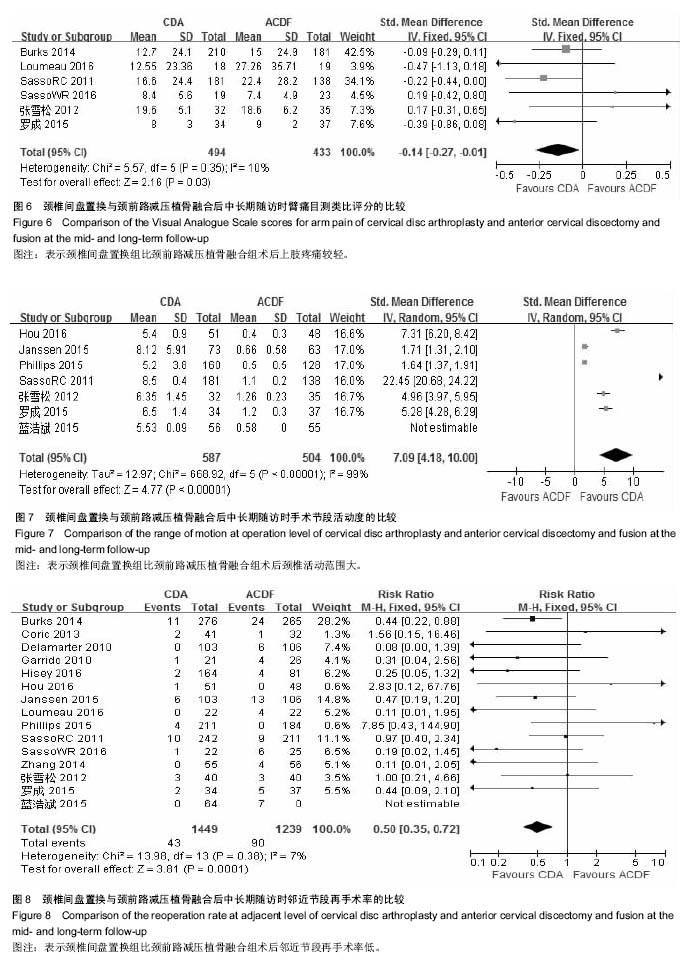
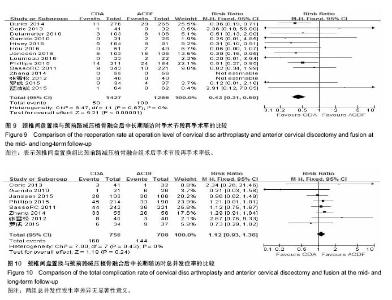
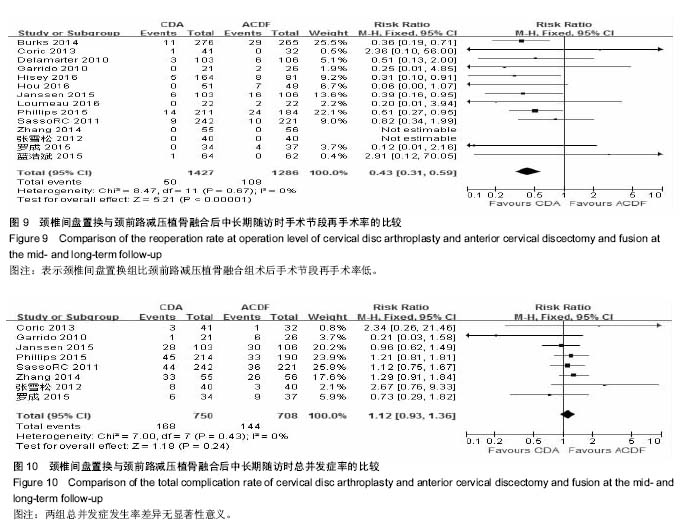
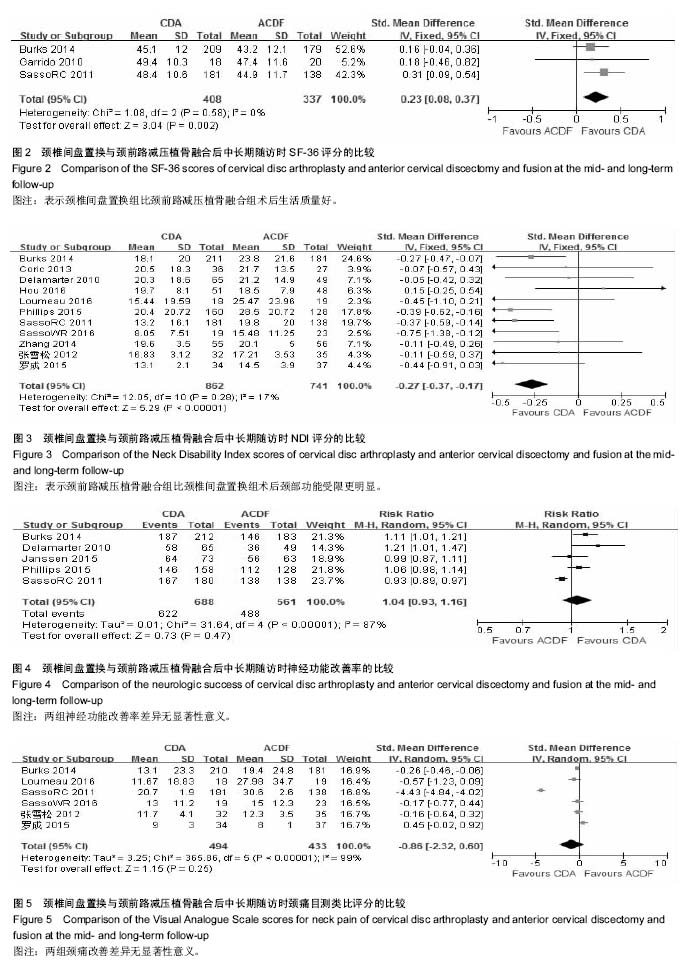
2.2 Meta分析结果 2.2.1 SF-36评分 纳入3项研究[22-23,26],各研究间无统计学异质性(P=0.58,I2=0%),采用固定效应模型。两组差异有显著性意义(SMD= 0.23,95% CI:0.08-0.37,P=0.002),表示颈椎间盘置换组比颈前路减压植骨融合组术后生活质量好,见图2。 2.2.2 NDI评分 纳入11项研究[21,23-28,30,33-35],各研究间无统计学异质性(P=0.59,I2=0%),采用固定效应模型。两组差异有显著性意义(SMD=-0.27,95% CI:-0.37至-0.17,P < 0.000 01),表示颈前路减压植骨融合组比颈椎间盘置换组术后颈部功能受限更明显,见图3。 2.2.3 神经功能改善率 纳入5项研究[21。23。26。28-29],各研究间有统计学异质性(P < 0.000 01,I2=87%),采用随机效应模型。两组差异无显著性意义(RR=1.04,95% CI:0.93-1.16,P=0.47),见图4。 2.2.4 颈痛目测类比评 纳入6项研究[23-24,26,30,34-35],各研究间有统计学异质性(P < 0.000 01,I2=99%),采用随机效应模型。两组差异无显著性意义(RR=-0.86,95% CI:-2.32-0.60,P=0.25),见图5。 2.2.5 臂痛目测类比评分 纳入6项研究[23-24,26。30。34-35],各研究间无统计学异质性(P=0.35,I2=10%),采用固定效应模型。两组差异有显著性意义(SMD=-0.14,95% CI:-0.27至-0.01,P=0.03),表示颈椎间盘置换组比颈前路减压植骨融合组术后上肢疼痛较轻,见图6。 2.2.6 手术节段活动度 纳入7项研究[23-24,28-31,33],各研究间有统计学异质性(P < 0.000 01,I2=99%),采用随机效应模型。两组差异有显著性意义(RR=7.09,95% C:4.18-10.00,P < 0.000 1),表示颈椎间盘置换组比颈前路减压植骨融合组术后颈椎活动范围大,见图7。 2.2.7 邻近节段再手术率 纳入15项研究[21-35],各研究间无统计学异质性(P=0.38,I2=7%),采用固定效应模型。两组差异有显著性意义(RR=0.50,95% CI:0.35-0.72,P < 0.000 1),表示颈椎间盘置换组比颈前路减压植骨融合组术后邻近节段再手术率低,见图8。 2.2.8 手术节段再手术率 纳入14项研究[21-34],各研究间无统计学异质性(P=0.67,I2=0%),采用固定效应模型。两组差异有显著性意义(RR=0.43,95% CI:0.31-0.59,P < 0.000 01),表示颈椎间盘置换组比颈前路减压植骨融合组术后手术节段再手术率低,见图9。 2.2.9 总并发症率 纳入8项研究[22-25,27-30],各研究间无统计学异质性(P=0.43,I2=0%),采用固定效应模型。两组差异无显著性意义(RR=1.12,95% CI:0.93-1.36,P=0.24),见图10。"
| [1] Goffin J,Geusens E,Vantomme N,et al.Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech.2004;17(2):79-85.[2] Buchowski JM, Anderson PA, Sekhon L,et al.Cervical disc arthroplasty compared with arthrodesis for the treatment of myelopathy. Surgical technique. J Bone Joint Surg Am.2009; 91 Suppl 2:223-232.[3] Rao RD, Currier BL, Albert TJ, et al. Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management.J Bone Joint Surg Am.2007; 89(6):1360-1378.[4] Bohlman HH, Emery SE, Goodfellow DB,et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients.J Bone Joint Surg Am.1993; 75(9): 1298-1307.[5] Shriver MF,Lewis DJ,Kshettry VR,et al.Pseudoarthrosis rates in anterior cervical discectomy and fusion: a meta-analysis. Spine J.2015; 15(9): 2016-2027. [6] Hilibrand AS, Robbins M.Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J.2004; 4(6 Suppl): 190S-194S. [7] Wigfield C, Gill S, Nelson R,et al.Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease. J Neurosurg. 2002; 96(1 Suppl): 17-21. [8] Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am.1999; 81(4): 519-528. [9] Fernstrom U.Arthroplasty with intercorporal endoprothesis in herniated disc and in painful disc. Acts Chir Scand Suppl. 1966(357):154-159.[10] Dmitriev AE, Cunningham BW, Hu N,et al. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine.2005; 30(10): 1165-1172.[11] Gandhi AA, Kode S, DeVries NA, et al. Biomechanical Analysis of Cervical Disc Replacement and Fusion Using Single Level, Two level and Hybrid Constructs. Spine. 2015; 40(10):1578-1585.[12] Lee JH, Kim JS, Lee JH, et al. Comparison of cervical kinematics between patients with cervical artificial disc replacement and anterior cervical discectomy and fusion for cervical disc herniation. Spine J.2014; 14(7):1199-1204.[13] Anakwenze OA, Auerbach JD, Milby AH, et al. Sagittal cervical alignment after cervical disc arthroplasty and anterior cervical discectomy and fusion: results of a prospective, randomized, controlled trial. Spine.2009; 34(19):2001-2007. [14] Chen J,Wang X,Bai W,et al.Prevalence of heterotopic ossification after cervical total disc arthroplasty: a meta-analysis. Eur Spine J.2012; 21(4): 674-680. [15] Leung C,Casey AT,Goffin J,et al.Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery.2005; 57(4):759-763. [16] Zechmeister I, Winkler R, Mad P. Artificial total disc replacement versus fusion for the cervical spine: a systematic review. Eur Spine J.2011; 20(2): 177-184.[17] Ganbat D, Kim K, Jin YJ,et al. Heterotopic ossification in cervical total disk replacement: a finite element analysis. Proc Inst Mech Eng H. 2014; 228(2): 200-205.[18] Grob D,Porchet F,Jeszenszky D,et al. A comparison of outcomes of cervical disc arthroplasty and fusion in everyday CIinical practice: surgical and methodological aspects. Eur Spine J.2010;19(2):297-306.[19] Yu L, Song Y, Yang X,et al. Systematic Review and Meta-analysis of Randomized Controlled Trials:Comparison of Total Disk Replacement With Anterior Cervical Decompression and Fusion. Orthopedics.2011;34(10): 651-657.[20] Jadad AR,Moore RA,Carroll D,et al.Assessing the quality of reports of randomized CIinical trials: is blinding necessary? Control Clin Trials.1996;17(1): 1-12.[21] Delamarter R,Murrey DB,Janssen ME,et al.Results at 24 months from the prospective,randomized,multicenter Investigational Device Exemption Trial of ProDisc-C versus anterior cervical discectomy and fusion with 4-year follow-up and continued access patients. SAS Journal. 2010;4(1):122-128.[22] Garrido BJ,Taha TA,Sasso RC.CIinical Outcomes of Bryan Cervical Disc Arthroplasty A Prospective,Randomized, Controlled,Single Site Trial With 48-Month Follow-up. J Spinal Disord Tech. 2010;23(6):367-371.[23] Sasso RC,Anderson PA,Riew KD,et al. Results of cervical arthroplasty compared with anterior discectomy and fusion:four-year CIinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011; 93(18):1684-1692.[24] 张雪松,张永刚,王岩,等.单节段人工椎间盘置换治疗颈椎病的中长期疗效[J]. 中国脊柱脊髓杂志,2012,22(10):879-883.[25] Coric D,Kim P,CIemente JD,et al. Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up:results in 74 patients from a single site. J Neurosurg Spine.2013;18(1):36-42. [26] Burkus JK,Traynelis VC,Haid RW Jr,et al. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up fromthe Prestige prospectiverandomized controlled clinical trial: Clinical article.J Neurosurg Spine.2014;21(4): 516-28. [27] Zhang HX, Shao YD, Chen Y, et al. A prospective, randomised, controlled multicentre study comparing cervical disc replacement with anteriorcervical decompression and fusion. Int Orthop.2014; 38(12): 2533-2541.[28] Phillips FM, Geisler FH, Gilder KM,et al.Long-term Outcomes of the US FDA IDE Prospective, Randomized Controlled Clinical Trial Comparing PCMCervical Disc Arthroplasty With Anterior Cervical Discectomy and Fusion.Spine (Phila Pa 1976).2015;40(10):674-683.[29] Janssen ME,Zigler JE,Spivak JM,et al.ProDisc-C Total Disc Replacement Versus Anterior Cervical Discectomy and Fusion for Single-LevelSymptomatic Cervical Disc Disease: Seven-Year Follow-up of the Prospective Randomized U.S. Food and Drug Administration Investigational Device Exemption Study. J Bone Joint Surg Am. 2015 ;97(21):1738-1747. [30] 罗成,瞿霞,陈波,等.颈椎间盘置换和椎间盘切除植骨融合修复单节段颈椎病:随机对照中期随访[J]. 中国组织工程研究, 2015, 19(9):1358-1364.[31] 蓝浩斌,苏红英,王涛.人工颈椎间盘治疗颈椎间盘脱出症的有效性和安全性:5年随机对照研究[J].微创医学,2015,10(6): 743-755.[32] Hisey MS,Zigler JE,Jackson R,et al. Prospective, randomized comparison of one-level Mobi-C cervical total disc replacement vs.anterior cervical discectomy and fusion: results at 5-year follow-up.Int J Spine Surg.2016;10(1):1-10.[33] Hou Y, Nie L, Pan X, et al. Effectiveness and safety of Mobi-C for treatment of single-level cervical disc spondylosis: a randomised control trial with a minimum of five years of follow-up. Bone Joint J.2016;98-B(6):829-833.[34] Loumeau TP, Darden BV, Kesman TJ, et al. A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease(SCDD) following ProDisc-C total disc arthroplasty(TDA) versus anterior cervical discectomy and fusion(ACDF). Eur Spine J.2016;25(7):2263-2270.[35] Sasso WR, Smucker JD, Sasso MP, et al. Long-Term Clinical Outcomes of Cervical Disc Arthroplasty: A prospective, randomized, controlled trial. Spine. 2016. [Epub ahead of print].[36] Jawahar A,Cavanaugh DA,Birdsong EM,et al. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized CIinical trials. Spine J .2010; 10(12):1043-1048.[37] Steinmetz MP,Patel R,Traynelis V,et al. Cervical disc arthroplasty compared with fusion in a workers’compensation population. Neurosurgery.2008;63(4):741-747.[38] Phillips FM, Lee JY, Geisler FH, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. 2-year results from the US FDA IDE clinical trial. Spine.2013; 38(15): E907-18.[39] Luo J, Gong M, Huang S, et al.Incidence of adjacent segment degeneration in cervical disc arthroplasty versus anterior cervical decompression and fusion meta-analysis of prospective studies.Arch Orthop Trauma Surg.2015; 135(2): 155-160.[40] Jawahar A,Cavanaugh DA,Birdsong EM,et al.Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized CIinical trials. Spine J.2010; 10(12):1043-1048.[41] Nunley PD,Jawahar A,Gordon CJ,et al.Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4- year follow-up of 3 prospective randomized trials. Spine.2012;37(6):445-451.[42] Yin Si,Yu Xiao,Zhou Shuangli,et al. Is Cervical Disc Arthroplasty Superior to Fusion for Treatment of Symptomatic Cervical Disc Disease? A Meta-Analysis. CIin Orthop Relat Res.2013;471(6):1904-1919.[43] Jackson RJ, Davis RJ, Hoffman GA,et al. Subsequent surgery rates after cervical total disc replacement using a Mobi-C Cervical Disc Prosthesis versus anterior cervical discectomy and fusion: a prospective randomized clinical trial with 5-year follow-up. J Neurosurg Spine.2016; 24(5): 734-745.[44] Anderson PA,Sasso RC,Riew KD. Comparison of adverse events between the Bryan artificial cervical disc and anterior cervical arthrodesis. Spine.2008;33(12):1305-1312.[45] Campbell PG, Yadla S, Malone J, et al.Early complications related to approach in cervical spine surgery: single-center prospective study. World Neurosurg.2010; 74(2-3):363-368.[46] Skeppholm M,Ingebro C,Olerud C, et al.The Dysphagia Short Questionnaire: an instrument for evaluation of dysphagia: a validation study with 12 months’ follow-up after anterior cervical spine surgery. Spine.2012;37(11):996-1002.[47] Park DK,Lin EL,Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion: in vivo quantitative radiographic analysis. Spine.2011;36(9): 721-730.[48] Chen J,Wang X,Bai W,et al. Prevalence of heterotopic ossification after cervical total disc arthroplasty: a meta-analysis. Eur Spine J.2012;21(4):674-680. [49] 田伟,吕艳伟,刘亚军,等.中国大陆人工颈椎间盘置换术后异位骨化发生率的Meta分析[J]. 中华骨科杂志,2013,33(8):785-791. |
| [1] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [2] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [3] | Zhang Jinglin, Leng Min, Zhu Boheng, Wang Hong. Mechanism and application of stem cell-derived exosomes in promoting diabetic wound healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1113-1118. |
| [4] | He Yunying, Li Lingjie, Zhang Shuqi, Li Yuzhou, Yang Sheng, Ji Ping. Method of constructing cell spheroids based on agarose and polyacrylic molds [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 553-559. |
| [5] | He Guanyu, Xu Baoshan, Du Lilong, Zhang Tongxing, Huo Zhenxin, Shen Li. Biomimetic orientated microchannel annulus fibrosus scaffold constructed by silk fibroin [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 560-566. |
| [6] | Chen Xiaoxu, Luo Yaxin, Bi Haoran, Yang Kun. Preparation and application of acellular scaffold in tissue engineering and regenerative medicine [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 591-596. |
| [7] | Kang Kunlong, Wang Xintao. Research hotspot of biological scaffold materials promoting osteogenic differentiation of bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 597-603. |
| [8] | Shen Jiahua, Fu Yong. Application of graphene-based nanomaterials in stem cells [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 604-609. |
| [9] | Zhang Tong, Cai Jinchi, Yuan Zhifa, Zhao Haiyan, Han Xingwen, Wang Wenji. Hyaluronic acid-based composite hydrogel in cartilage injury caused by osteoarthritis: application and mechanism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 617-625. |
| [10] | Li Hui, Chen Lianglong. Application and characteristics of bone graft materials in the treatment of spinal tuberculosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 626-630. |
| [11] | Gao Cangjian, Yang Zhen, Liu Shuyun, Li Hao, Fu Liwei, Zhao Tianyuan, Chen Wei, Liao Zhiyao, Li Pinxue, Sui Xiang, Guo Quanyi. Electrospinning for rotator cuff repair [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(4): 637-642. |
| [12] | Guan Jian, Jia Yanfei, Zhang Baoxin , Zhao Guozhong. Application of 4D bioprinting in tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(3): 446-455. |
| [13] | Liu Jiali, Suo Hairui, Yang Han, Wang Ling, Xu Mingen. Influence of lay-down angles on mechanical properties of three-dimensional printed polycaprolactone scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2612-2617. |
| [14] | Huang Bo, Chen Mingxue, Peng Liqing, Luo Xujiang, Li Huo, Wang Hao, Tian Qinyu, Lu Xiaobo, Liu Shuyun, Guo Quanyi . Fabrication and biocompatibility of injectable gelatin-methacryloyl/cartilage-derived matrix particles composite hydrogel scaffold [J]. Chinese Journal of Tissue Engineering Research, 2022, 10(16): 2600-2606. |
| [15] | Fang Xiaoyang, Tang Tian, Wang Nan, Qian Yuzhang, Xie Lin. Repair and regenerative therapies of the annulus fibrosus [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(10): 1582-1587. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||