Chinese Journal of Tissue Engineering Research ›› 2016, Vol. 20 ›› Issue (20): 2964-2971.doi: 10.3969/j.issn.2095-4344.2016.20.011
Previous Articles Next Articles
Mechanisms underlying the promotion of wound healing by bletilla carrying exogenous recombinant human epidermal growth factor
Wang Xiao, Cui Ping, Wu Ran, Wang Bei, Qiu Shu-lin
- Department of Medical Cosmetology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China
-
Received:2016-03-16Online:2016-05-13Published:2016-05-13 -
Contact:Qiu Shu-lin, Chief physician, Department of Medical Cosmetology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China -
About author:Wang Xiao, Master, Attending physician, Department of Medical Cosmetology, Hebei General Hospital, Shijiazhuang 050051, Hebei Province, China -
Supported by:the Key Science and Technology Program of Hebei Province, China, No. 062761220
CLC Number:
Cite this article
Wang Xiao, Cui Ping, Wu Ran, Wang Bei, Qiu Shu-lin. Mechanisms underlying the promotion of wound healing by bletilla carrying exogenous recombinant human epidermal growth factor[J]. Chinese Journal of Tissue Engineering Research, 2016, 20(20): 2964-2971.
share this article
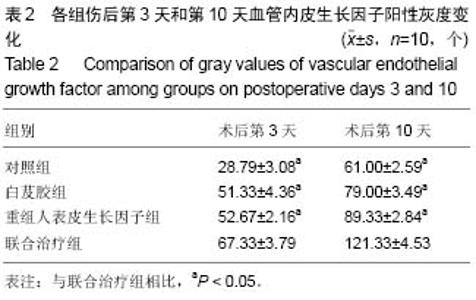
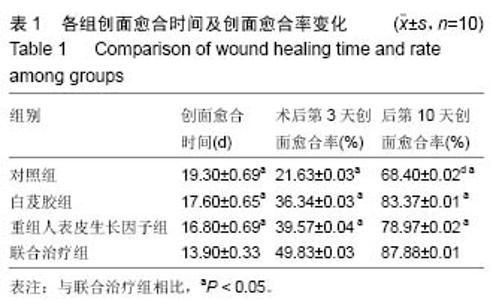
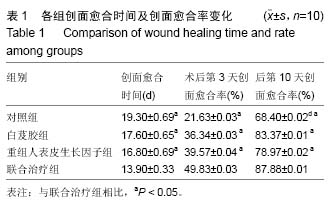
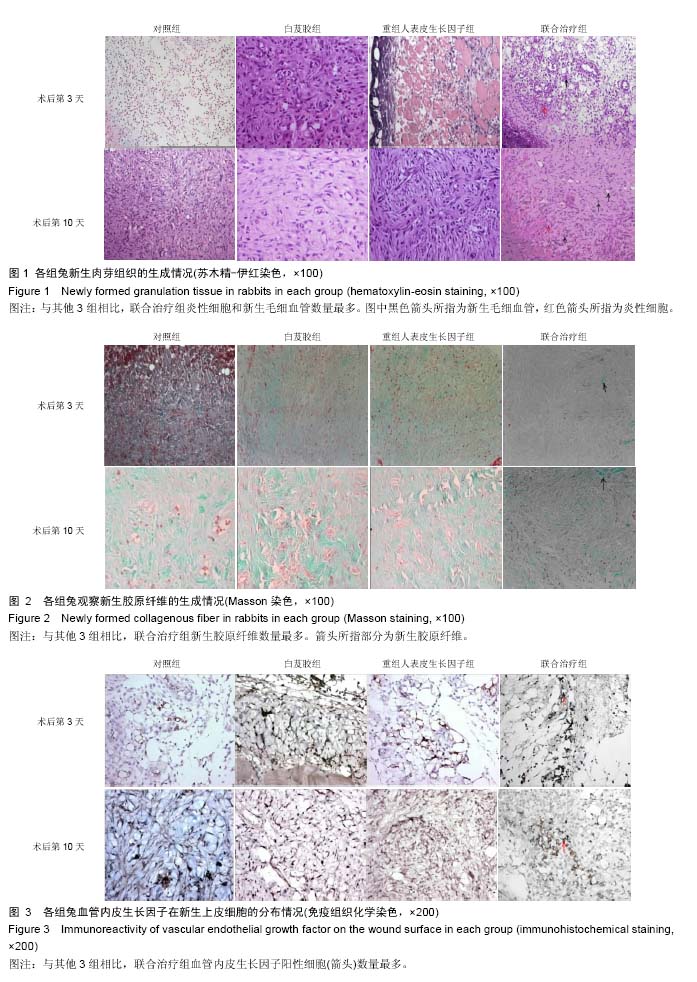
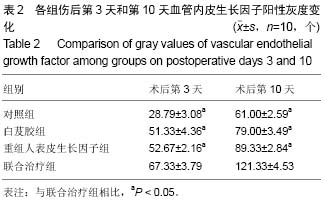
2.3 兔创面愈合率变化 从表1可见,术后第3,10天,联合治疗组伤口愈合率最高,与其他3组比较均差异有显著性意义(P < 0.05)。 2.4 兔创面组织形态变化 术后第3天,各组中性粒细胞、淋巴细胞等渗出较多,白芨胶、重组人表皮生长因子和联合治疗组可见少量新生毛细血管。联合治疗组巨噬细胞、成纤维细胞和新生毛细血管最多,对照组最少(图1)。术后第10天,4组肉芽组织均较术后第3天更致密,细胞渗出以淋巴细胞和巨噬细胞为主。联合治疗组淋巴细胞、巨噬细胞、成细纤维细胞和新生毛细血管数量最多,对照组最少(图1)。 2.5 兔创面组织的Masson染色结果 Masson氏三色染色将结缔组织和胶原纤维染成绿色,平滑肌染成红色,细胞核染成褐色。术后第3,10天,联合治疗组胶原纤维数量最多,对照组最少(图2)。 2.6 兔创面组织血管内皮生长因子表达变化 术后第3,10天,免疫组织化学染色显示,各组中联合治疗组血管内皮生长因子阳性细胞灰度值最大,对照组最少(图3,表2)。"
| [1] Werdin F, Tenenhaus M, Rennekampff HO. Chronicwound care. Lancet. 2008;372(9653):1860-1862.[2] Stephanie R, Robert F. Wound healing primer. Crit Care Nurs Clin North Am. 2012;24(2):165-178.[3] Savk O, Savk E. Reverse sural artery flap for distal lower extremity defects. J Dermatol. 2006;33(10): 700-704.[4] Saito T, Izumi K, Shiomi A, et al. Zoledronic acid impairsre-epithelialization through down-regulation of integrin αvβ6 and transforming growth factor beta signalling in a three-dimensional in vitro wound healing model. Int J Oral Maxillofac Surg. 2014;43(3):373-380.[5] 刘宸,章宏伟.富血小板血浆促进慢性创面愈合研究进展[J].中华烧伤杂志,2014,30(5):433-436.[6] Greaves NS, lqbal SA, Morris J, et al. Acute cutaneous wounds treated with human decellularised dermis show enhanced angiogenesis during healing. PLoS One. 2015;10(1):e0113209.[7] Yuan T, Zhang CQ, Tang MJ, et al. Autologous Platelet-rich Plasma Enhances Healing of Chronic Wounds. Wounds. 2009;21(10):280-285.[8] Eagan MJ, ZukPA, ZhaoKW, et al. The suitability of human adipose-derived stem cells for the engineering of ligament tissue. J Tissue Eng Regen Med. 2012; 6(9):702-709.[9] Nie C, Yang D, Xu J, et al. Locally administered adipose-derivedstem cells acceleratewound healing through differentiation and vasculogenesis. Cell Transplant. 2011;20(2):205-216.[10] Caruana G, Bertozzi N, Boschi E, et al. Role of adipose-derived stem cells in chronic cutaneous wound healing. Ann Ital Chir. 2015;86(1):1-4.[11] Zonari A , Martins TM , Paula AC, et al. Polyhydroxybutyrate-co-hydroxyvalerate structures loaded with adipose stem cells promote skin healing with reduced scarring. Acta Biomaterialia. 2015; 17(15):170-181.[12] Marino G, Moraci M, Armenia E, et al. Therapy with autologous adipose-derived regenerative cells for the care of chronic ulcer of lower limbs in patients with peripheral arterial disease. J Surg Res. 2013;185(1): 36-44.[13] Bura A, Planat-Benard V, Bourin P, et al. Phase I trial:the use of autologous cultured adipose-derived stroma/stem cells to treat patients with non-revascularizable critical limb ischemia. Cytotherapy. 2014;16(2):245-257.[14] Cobos Campos R, Parraza Diez N, Aizpuru Barandiaran F. Platelet-rich plasma in skin ulcer treatment. Wounds. 2013;25(9):256-262.[15] Yotsu RR, Hagiwara S, Okochi H, et al. Case series of patients with chronic foot ulcers treated with autologous platelet-rich plasma. J Dermatol. 2015; 42(3): 288-295.[16] Orig R, Singleton J. A non-comparative evaluation of a chitosan gelling fibre. Br J Nurs. 2016;25(3):162-170. [17] Fan L, Cheng C, Qiao Y, et al. GNPs-CS/KGMas hemostaticfirstaid wound dressingwith antibioticeffect: in vitro and in vivo study. PLoS One. 2013;8(7):e66890.[18] Hooper SJ, Williams DW, Thomas DW, et al. An in vitro comparison of two silver-containingantimicrobial wound dressings. Ostomy Wound Manage. 2012; 58(1):16-22.[19] Phaechamud T, Yodkhum K, Charoenteeraboon J, et al. Chitosan-aluminummonostearate composite sponge dressingcontaining asiaticoside for wound healing and angiogenesis promotionin chronic wound. Mater Sci Eng C Mater Biol Appl. 2015;50:210-225.[20] Meuleneire F. A vapour-permeable film dressing used on superficial wounds. Br J Nurs. 2014;23(15):S36-S43.[21] 蔡东岭,陈锦钊,曾巧,等.聚氨酯中药敷料治疗感染创面的实验研究[J].中国民族民间医药杂志,2013,22(3):24-25.[22] 秦丹青,徐何朝夫,王俭锋.加入中药的敷贴在外科手术术后促进切口愈合的作用[J].中国保健营养,2012,22(10) 4120-4121.[23] 曹永清,何春梅,陆金根,等.温脾健胃方对大鼠慢性创面愈合的影响[J].中西医结合学报,2005,3(3):220-224.[24] Lau TW, Lam FF, Lau KM, et al. Pharmacologicalinvestigationon the wound healingeffects of Radix Rehmanniae in an animal model of diabetic foot ulcer. J Ethnopharmacol. 2009; 123(1):155-162.[25] 杨素清,张瀚月.白芨在常见皮肤疾病外治法中的应用[J].中国临床研究,2014,6(10):33-35.[26] 邱红梅,张颖,周岐新,等.白芨多糖对小鼠免疫功能的调节作用[J].中国生物制品学杂志,2011,24(6):676-678.[27] 董莉,董永喜,刘星星,等.白芨多糖对大鼠血小板聚集、疑血功能及TXB2、6-keto-PGF1α表达的影响[J].贵阳医学院学报,2014,39(4):459-462.[28] 任华忠,何毓敏,杨丽.白芨化学成分及其药理活性研究进展[J].亚太传统医药,2009,5(2):134-140.[29] 彭锐,李胜利,邹阳,等.明胶白芨胶/纳米血竭多孔材料对大鼠创面组织血管内皮生长因子表达的影响[J].中国中医骨伤科杂志,2007,15(6):15-16.[30] 王红英.白芨甘露聚糖抗胃溃疡及抗炎、镇痛作用的实验研究[J].浙江中医药大学学报,2009,33(1):119-121.[31] 悦随士,田河林,李丽鸣,等.白芨甘露聚糖胶浆治疗上消化道出血的临床观察[J].中国现代医学杂志,2007,17(19): 2375-2377.[32] 张晓玲,张宝林.rhEGF对人皮肤成纤维细胞的促增殖作用[J].山西医科大学学报,2008,39(7):624-626.[33] 彭艳阳,吴伟,曾丽娜,等.重组人表皮生长因子和碱性成纤维生长因子促进人角膜上皮细胞的增殖[J].中国组织工程研究,2014,18(7):1045-1050.[34] 李姗姗,朱晓美,鲍岩岩.等.重组人表皮生长因子的构建与表达[J].哈尔滨医科大学学报,2011,45(4):297-300.[35] 刘如俊,赵文志,张路,等.表皮生长因子在糖尿病足溃疡创面愈合过程中的作用观察及其机制探讨[J].大连医科大学学报,2014,36(4):322-327.[36] 杨伯明.重组人表皮细胞生长因子促进深Ⅱ度烧伤创面愈合的临床观察[J].中国当代医学,2013,20(24):99-100.[37] 王晓红,赵欣美,赵正娟.重组人表皮生长因子在创面美容修复中的应用[J].中国美容医学,2014,23(3):175-176.[38] 鞠梅,郑志菊,张小华,等.重组人表皮生长因子促进创面愈合的临床观察[J].中华皮肤科杂志,2002,35(3):237.[39] 过云,虞俊杰,吕国忠.外用重组人表皮生长因子凝胶治疗浅Ⅱ度烧伤创面的临床观察[J].中华损伤与修复杂志(电子版),2009,4(6):683-687.[40] 宗守凯,梁自乾,纪雪亮.表皮生长因子联合血糖控制对糖尿病创面愈合的影响:成纤维细胞生长因子蛋白芨其mRNA表达的变化[J].中国组织工程研究与临床康复, 2010,14(37):6882-6886.[41] 付小兵,程飚,盛志勇.生长因子应用于临床创伤修复—十年的主要进展与展望[J].中国修复重建外科杂志, 2004, 18(6):508-512.[42] Xing B, Wu F, Li T, et al. Experimental study of comparing rhEGFwith rhβFGF on improving the quality of woundhealing. Int J Clin Exp Med. 2013;6(8):655-661.[43] Zhu JX , Zhang YM. Application of recombinant human epidermal growth factor on chronic ulcer wound. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2002; 16(1): 42-43. [44] Fernández-Montequín JI, Valenzuela-Silva CM, Díaz OG, et al. Intra-lesional injections of recombinant human epidermal growth factor promote granulation and healing in advanced diabetic foot ulcers: multicenter, randomised, placebo-controlled, double-blind study. Int Wound J. 2009;6(6):432-443.[45] 谷廷敏,隋志甫,石成方.EGF和EGFr基因在临床供皮区创面愈合中表达的研究[J].中国美容医学,2012,21(15): 1985-1986.[46] 罗江孝.中药油纱辅助重组人表皮生长因子凝胶治疗慢性体表溃疡的临床研究[J].中医学报,2014,29(1):129-131.[47] 马培耕,廖建中,庄雪芬.白芨胶载高分子神经生长因子治疗深度压疮的研究[J].中国现代医生,2014,52(14):50-52.[48] 郑军,黄晓元,韦星.重组人表皮生长因子促进大鼠皮肤创面愈合的研究[J].中华整形外科杂志,2005,21(5):379-383.[49] 王世岭,马建丽,柴家科,等.重组人表皮生长因子软膏对烧伤创面修复的促进作用[J],中国修复重建外科外杂志, 2002,16(3):173-176.[50] Jia MM, Li YS, Pei LJ, el at. Effect of San-huang- sheng-fu oil on wounds of full-thickness scald in rabbits. Zhonghua Shao Shang Za Zhi. 2013;29(1):50-54.[51] 侯量,吴旭,王武军.蜕皮甾酮对伤口促愈作用的初步研究[J],南方医科大学学报,2007,27(3):312-314.[52] 王志刚,窦科峰,李海民,等.致康胶囊促进大鼠伤口愈合及与转化生长因子-β表达的关系[J].中华实验外科杂志, 2004,21(10):1197-1198.[53] Yu N, Zhai X, Xin C. An experimental study of rabbits' wound repair by amniotic carrier complex membrane containing bFGF and vitamin C and loaded with BMSCs, Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2008,22(12): 1495-1500.[54] Hemmati AA, Aghel N, Rashidi I, et al. Topical grape (Vitis vinifera) seed extract promotes repair of full thickness wound in rabbit. Int Wound J. 2011;8(5): 514-520.[55] 林子洪,许环亲,胡婧晔,等.复方中药促进家兔皮肤创伤愈合的实验研究[J].实用医学杂志,2007,23(14):2129-2131.[56] 付小兵,孙同柱,盛志勇.几种用于创伤修复研究的动物模型[J].中华实验外科杂志,1999,16(5):479-480.[57] 李凌川,李玲,郝平.重组人表皮生长因子促进兔创面愈合及其量效关系的实验研究[J].中国美容医学, 2011,20(12): 1926-1928.[58] 邱彦,鲁毅,段靖,等.血余炭纳米纤维膜促进家兔创面愈合的实验研究[J],药学实践杂志,2013,31(6):438-441, 458.[59] Zimny S, Schatz H, Pfohl U. The effects of applied felted foam on wound healing and healing times in the therapy of neuropathic diabetic foot ulcers. Diabet Med. 2003;20(8):622-625.[60] Jessup RL. What is the best method for assessing the rate of wound healing? A comparison of 3 mathematical formulas. Adv Skin Wound Care. 2006; 19(3):138-147 .[61] 杨廷.高压氧对兔耳增生性瘢痕形成过程中HIF-1Q、VEGF及TGFβ1表达的影响[D].青岛:青岛大学,2014.[62] 付小兵.现代创伤修复学[M].北京:人民军医出版社,1999.[63] Dale PD, Sherratt JA, Maini PK. Role of fibroblast migration in collagen fiber formation during fetal and adult dermal wound healing. Bull Math Biol. 1997; 59(6):1077-1100.[64] Moyer KE, Davis A, Saggers GC, et al. Wound healing: the role of gap junctional communication in rat granulation tissue maturation. Exp Mol Pathol. 2002; 72(1):10-16.[65] Chereddy KK, Lopes A, Koussoroplis S, et al. Combined effects of PLGA and vascular endothelial growth factor promote the healing of non-diabetic and diabetic wounds. Nanomedicine. 2015;11(8): 1975-1984. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [3] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [4] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [5] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [6] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [7] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [8] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [9] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [10] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [11] | Chen Siqi, Xian Debin, Xu Rongsheng, Qin Zhongjie, Zhang Lei, Xia Delin. Effects of bone marrow mesenchymal stem cells and human umbilical vein endothelial cells combined with hydroxyapatite-tricalcium phosphate scaffolds on early angiogenesis in skull defect repair in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3458-3465. |
| [12] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [13] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| [14] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| [15] | Liu Liyong, Zhou Lei. Research and development status and development trend of hydrogel in tissue engineering based on patent information [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3527-3533. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||