Chinese Journal of Tissue Engineering Research ›› 2015, Vol. 19 ›› Issue (17): 2683-2687.doi: 10.3969/j.issn.2095-4344.2015.17.011
Previous Articles Next Articles
Anatomic measurements of internal fixation-related implantation points of inferior thoracic spinal latero-anterior vertebral screws
Sun Xiang-xin, Wang Zhi-jie
- Department of Spine Surgery, Affiliated Hospital of Qingdao University, Qingdao 266000, Shandong Province, China
-
Online:2015-04-23Published:2015-04-23 -
Contact:Wang Zhi-jie, Chief physician, Professor, Department of Spine Surgery, Affiliated Hospital of Qingdao University, Qingdao 266000, Shandong Province, China -
About author:Sun Xiang-xin, Master, Department of Spine Surgery, Affiliated Hospital of Qingdao University, Qingdao 266000, Shandong Province, China
CLC Number:
Cite this article
Sun Xiang-xin, Wang Zhi-jie. Anatomic measurements of internal fixation-related implantation points of inferior thoracic spinal latero-anterior vertebral screws[J]. Chinese Journal of Tissue Engineering Research, 2015, 19(17): 2683-2687.
share this article
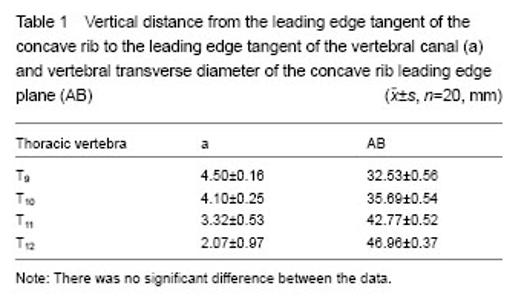
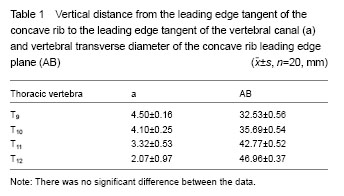
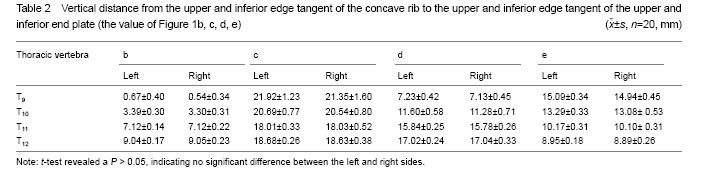
Measurement results of anatomical data Vertical distance from the leading edge tangent of the concave rib to the leading edge tangent of the vertebral canal and vertebral transverse diameter of the concave rib leading edge plane was measured (Figure 1). The distance between the anterior edge of the concave rib and anterior edge of the vertebral canal (the value of a) decreased from T9 (4.50±0.16) mm to T12 (2.07±0.97) mm. The vertebral transverse diameter of the concave rib leading edge plane (the value of AB) increased from T9 (32.53±0.56) mm to T12 (46.96±0.37) mm. There was no significant difference between the left and right sides (Table 1). Vertical distance from the upper and inferior edge tangent of the concave rib to the upper and inferior edge tangent of the upper and inferior end plate The distance of the left side between the upper edge tangent of the concave rib and the upper edge tangent of the upper end plate increased from T9 (0.67±0.40) mm to T12 (9.04±0.17) mm and the right side increased from T9 (0.54±0.34) mm to T12 (9.05±0.23) mm (the value of Figure 1b). The distance of the left side between the upper edge tangent of the concave rib and the inferior edge tangent of the inferior end plate decreased from T9 (21.92±1.23) mm to T12 (18.68±0.26) and the right side decreased from T9 (21.35±1.60) mm to T12 (18.63±0.38) mm (the value of Figure 1c). The distance of the left side between the inferior edge tangent of the concave rib and the upper edge tangent of the upper end plate increased from T9 (7.23±0.42) mm to T12 (17.02±0.24) mm and the right side increased from T9 (7.13±0.45) mm to T12 (17.04±0.33) mm (the value of Figure 1d)."
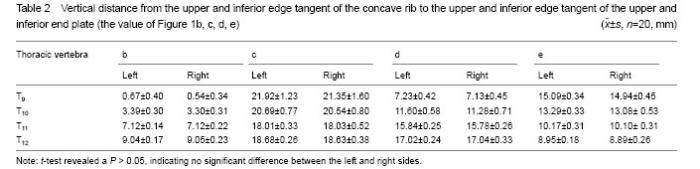
The distance of the left side between the inferior edge tangent of the concave rib and the inferior edge tangent of the inferior end plate decreased from T9 (15.09±0.34) to T12 (8.95±0.18) and the right side decreased from T9 (14.94±0.45) to T12 (8.89±0.26) (the value of Figure 1e). P more than 0.05, it was no significant difference between the left and right sides (Table 2)."
| [1]Liu J, Xiang BL, Wang Q, et al. Posterior screw-rod system fixation combined with anterolateral decompression and bone graft for severe thoracolumbar burst fracture in 12 cases. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2011;15(35):6536-6539. [2]Hei L, Yuan HF, Zhao HN, et al. Removal of intraosseous cartilaginous node originated from thoracic vertebrae via anterolateral extrapleural approach. Zhongguo Jizhui Jisui Zazhi. 2014;24(7):616-620. [3]Wang YP, Wang XC, Xiong CL, et al. One stage posterior transpedicle fixation and debridement with bone graft to treat thoracic spinal tuberculosis. Linchuang Guke Zazhi. 2014; 17(1):8-10. [4]Herring JA, Bradford DS. The Spine. American: Mc-Graw-HillInc. 2001:353-354. [5]Ghanayem AJ. Anterior instrumentation in the management of thoracolumbar burst fractures. Clin Orthop Res.1997;33(5): 89-100. [6]Sucato DJ, Flohr R. Accurate preoperative rod length measurement for thoracoscopic anterior instrumentation and fusion for idiopathic scoliosis. J Spinal Disord Tech. 2005; Suppl:S96-S100. [7]Qiu Y, Rui BY, Zhu ZZ, et al. Nutrient artery entrance on the posterolateral wall of thoracic vertebral bodies: another potential landmark for vertebral screw insertion. Zhonghua Waike Zazhi. 2007;45(16):1105-1107. [8]Jin DD, Zeng DB, Chen JT, et al. Analysis of failures in thoracic waist spinal injury surgery. Zhongguo Jiaoxing Waike Zazhi. 2003;11(14):952-954. [9]Li ZJ, Li XH, Cai YQ, et al. Anatomy of costal fovea for costal head on vertebrae and its clinical significance. Jeipouxue Zazhi. 2006;29(3):351-354. [10]Zhu HT, Zhu YL, Zhang F, et al. Anatomic and radiographic study of the rib head associated with spinal canal and Vertebral body in adult. Zhongguo Jizhui Jisui Zazhi. 2011; 21(9):774-777. [11]Jin DD. Primary report of Z plate inner fixation system towards anterior approach of thoracic waist. Zhonghua Guke Zazhi. 1999;19(4):201-204. [12]Zhang H, Sucato DJ. Regional differences in anatomical landmarks for placing anterior instrumentation of the thoracic spine in both normal patients and patients with adolescent idiopathic scoliosis. Spine. 2006;31(2):183-189. [13]Li XH, Xu DC, Li ZJ, et al. An anatomical study in a Chinese population of the position of the rib head for placing anterior vertebral body screws. Morphol (Wamz). 2010;69(4): 232-240. [14]Li XH, Xu DC, Li ZJ, et al. Anatomical study of position of the rib head for placing anterior vertebral body screws in a Chinese population. Orthopedics. 2010;33(12);884-894. [15]Zhao TB, Fan QY, Li YQ, et al. Measurement of Chinese vertebrae in skeleton and X-ray photograph and its clinical significance. Zhongguo Linchuang Jiepouxue Zazhi. 2001; 19(4):302-304. [16]Li ZJ, Li Y, Shi CD, et al. Measurement on vertebral body morphology of adults in north. Zhongguo Zuzhi Gongcheng Yanjiu yu Linchuang Kangfu. 2008;12(28):5531-5540. [17]Beisse R. Endoscopic surgery on the thoracolumbar junction of the spine. Eur Spine J. 2006;15(6):687-704. [18]Newton PO. Thoracoscopic anterior instrumentation for idiopathic scoliosis. Spine J. 2009;9(7):595-598. [19]Lonner BS, Auerbach JD, Levin R, et al. Thoracoscopic anterior instrumented fusion for adolescent idiopathic scoliosis with emphasis on the sagittal plane. Spine J. 2009; 9(7):523-529. [20]Bis?evi? M, Bis?evi? S, Ljuca F, et al. The radiological estimation of vertebral body volumes on the thoracic and lumbal spine. Coll Antropol. 2014;38(2):505-509. [21]Oon Tan C, Botha C, Weinberg L, et al. Computerized tomographic anatomic relationships of the thoracic paravertebral space. J Cardiothorac Vasc Anesth. 2013; 27(6):1315-1320. [22]Ali AH, Cowan AB, Gregory JS, et al. The accuracy of active shape modelling and end-plate measurements for characterising the shape of the lumbar spine in the sagittal plane. Comput Methods Biomech Biomed Engin. 2012; 15(2):167-172. [23]Abuzayed B, Tutunculer B, Kucukyuruk B, et al. Anatomic basis of anterior and posterior instrumentation of the spine: morphometric study. Surg Radiol Anat. 2010;32(1):75-85. [24]Lonner BS, Auerbach JD, Levin R, et al. Thoracoscopic anterior instrumented fusion for adolescent idiopathic scoliosis with emphasis on the sagittal plane. Spine J. 2009; 9(7):523-529. [25]Sucato DJ, Kassab F, Dempsey M. et al. Analyis of screw placement relative to the aorta and spinal canal following anterior instrumentation for thoracic idiopathic scoliosis. Spine. 2004;29(5):554-559. [26]Li XH, Li ZJ, Wang HY, et al. Digital measurement of the vertebral body during lateral anterior internal fixation of middle and lower thoracic vertebrae. Zhongguo Zuzhi Gongcheng Yanjiu. 2013;17(22):4042-4046. [27]Bullmann V, Fallenberg EM, Meier N, et al. Anterior dual rod instrumentation in idiopathic thoracic scoliosis: a computed tomography analysis of screw placement relative to the aorta and the spinal canal. Spine. 2005;30(18):2078-2083. [28]D’Aliberti G, Talamonti G, Villa F, et al. Anterior approach to thoracic and lumbar spine lesions: results in 145 consecutive cases. J Neurosurg Spine. 2008;9(5):466-482. [29]Dai LY, Jiang LS, Jiang SD. Anterior-only stabilization using plating with bone structural autograft versus titanium mesh cages for two- or three-column thoracolumbar burst fractures: a prospective randomized study. Spine. 2009;34(14): 1429-1435. [30]Wu Y, Hou SX, Wu WW, et al. Studying the influence of age and short or long segments of pedicle screw instrumentation to the clinical efficacy of early single thoracolumbar fracture. Zhonghua Wai Ke Za Zhi. 2009;47(23):1790-1793. [31]Hu X, Siemionow KB, Lieberman IH. Thoracic and lumbar vertebrae morphology in Lenke type 1 female adolescent idiopathic scoliosis patients. Int J Spine Surg. 2014;8. doi: 10.14444/1030. [32]Cho W, Le JT, Shimer AL, et al. The insertion technique of translaminar screws in the thoracic spine: computed tomography and cadaveric validation. Spine J. 2015;15(2): 309-313. [33]Matsukawa K, Yato Y, Hynes RA, et al. Cortical bone trajectory for thoracic pedicle screws: a Technical note. J Spinal Disord Tech. 2014. [34]Qiu XS, Jiang H, Qian BP, et al. Influence of prone positioning on potential risk of aorta injury from pedicle screw misplacement in adolescent idiopathic scoliosis patients. J Spinal Disord Tech. 2014;27(5):E162-E167. [35]Vallefuoco R, Bedu AS, Manassero M, et al. Computed tomographic study of the optimal safe implantation corridors in feline thoraco-lumbar vertebrae. Vet Comp Orthop Traumatol. 2013;26(5):372-378. [36]Weaver J, Seipel S, Eubanks J. T1 intralaminar screws: an anatomic, morphologic study.Orthopedics. 2013; 36(4): e473-e477. [37]Cho W, Le JT, Shimer AL, Werner BC, et al. The insertion technique of translaminar screws in the thoracic spine: computed tomography and cadaveric validation. Spine J. 2015;15(2):309-313. [38]Qiu XS, Jiang H, Qian BP, et al. Influence of prone positioning on potential risk of aorta injury from pedicle screw misplacement in adolescent idiopathic scoliosis patients. J Spinal Disord Tech. 2014;27(5):E162-E167. [39]Cho W, Le JT, Shimer AL, et al. The insertion technique of translaminar screws in the thoracic spine: computed tomography and cadaveric validation. Spine J. 2015; 15(2): 309-313. [40]Qiu XS, Jiang H, Qian BP, et al. Influence of prone positioning on potential risk of aorta injury from pedicle screw misplacement in adolescent idiopathic scoliosis patients. J Spinal Disord Tech. 2014;27(5):E162-E167. [41]Shaikh KA, Bennett GM, White IK, et al. Computed-tomography-based anatomical study to assess feasibility of pedicle screw placement in the lumbar and lower thoracic pediatric spine. Childs Nerv Syst. 2012;28(10): 1743-1754. [42]Zhuang Z, Xie Z, Ding S, et al. Evaluation of thoracic pedicle morphometry in a Chinese population using 3D reformatted CT. Clin Anat. 2012;25(4):461-467. |
| [1] | Zhang Tongtong, Wang Zhonghua, Wen Jie, Song Yuxin, Liu Lin. Application of three-dimensional printing model in surgical resection and reconstruction of cervical tumor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1335-1339. |
| [2] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [3] | Zeng Yanhua, Hao Yanlei. In vitro culture and purification of Schwann cells: a systematic review [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1135-1141. |
| [4] | Xu Dongzi, Zhang Ting, Ouyang Zhaolian. The global competitive situation of cardiac tissue engineering based on patent analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 807-812. |
| [5] | Wu Zijian, Hu Zhaoduan, Xie Youqiong, Wang Feng, Li Jia, Li Bocun, Cai Guowei, Peng Rui. Three-dimensional printing technology and bone tissue engineering research: literature metrology and visual analysis of research hotspots [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 564-569. |
| [6] | Chang Wenliao, Zhao Jie, Sun Xiaoliang, Wang Kun, Wu Guofeng, Zhou Jian, Li Shuxiang, Sun Han. Material selection, theoretical design and biomimetic function of artificial periosteum [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 600-606. |
| [7] | Liu Fei, Cui Yutao, Liu He. Advantages and problems of local antibiotic delivery system in the treatment of osteomyelitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 614-620. |
| [8] | Li Xiaozhuang, Duan Hao, Wang Weizhou, Tang Zhihong, Wang Yanghao, He Fei. Application of bone tissue engineering materials in the treatment of bone defect diseases in vivo [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 626-631. |
| [9] | Zhang Zhenkun, Li Zhe, Li Ya, Wang Yingying, Wang Yaping, Zhou Xinkui, Ma Shanshan, Guan Fangxia. Application of alginate based hydrogels/dressings in wound healing: sustained, dynamic and sequential release [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 638-643. |
| [10] | Chen Jiana, Qiu Yanling, Nie Minhai, Liu Xuqian. Tissue engineering scaffolds in repairing oral and maxillofacial soft tissue defects [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(4): 644-650. |
| [11] | Xing Hao, Zhang Yonghong, Wang Dong. Advantages and disadvantages of repairing large-segment bone defect [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(3): 426-430. |
| [12] | Chen Siqi, Xian Debin, Xu Rongsheng, Qin Zhongjie, Zhang Lei, Xia Delin. Effects of bone marrow mesenchymal stem cells and human umbilical vein endothelial cells combined with hydroxyapatite-tricalcium phosphate scaffolds on early angiogenesis in skull defect repair in rats [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3458-3465. |
| [13] | Wang Hao, Chen Mingxue, Li Junkang, Luo Xujiang, Peng Liqing, Li Huo, Huang Bo, Tian Guangzhao, Liu Shuyun, Sui Xiang, Huang Jingxiang, Guo Quanyi, Lu Xiaobo. Decellularized porcine skin matrix for tissue-engineered meniscus scaffold [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3473-3478. |
| [14] | Mo Jianling, He Shaoru, Feng Bowen, Jian Minqiao, Zhang Xiaohui, Liu Caisheng, Liang Yijing, Liu Yumei, Chen Liang, Zhou Haiyu, Liu Yanhui. Forming prevascularized cell sheets and the expression of angiogenesis-related factors [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3479-3486. |
| [15] | Liu Chang, Li Datong, Liu Yuan, Kong Lingbo, Guo Rui, Yang Lixue, Hao Dingjun, He Baorong. Poor efficacy after vertebral augmentation surgery of acute symptomatic thoracolumbar osteoporotic compression fracture: relationship with bone cement, bone mineral density, and adjacent fractures [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(22): 3510-3516. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||