Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (12): 3134-3144.doi: 10.12307/2026.702
Previous Articles Next Articles
Different inspiratory muscle training methods improve exercise and cardiopulmonary function of patients after cardiac surgery: a network meta-analysis
Chen Ping1, Du Jinchao2, Wang Hongying2, Zhang Hui2, Wang Haixia3
- 1Rehabilitation Medicine Center, 3Department of Traditional Chinese Medicine, Affiliated Hospital of Shandong Second Medical University, Weifang 261053, Shandong Province, China; 2School of Rehabilitation Medicine, Shandong Second Medical University, Weifang 261053, Shandong Province, China
-
Received:2025-04-12Accepted:2025-08-13Online:2026-04-28Published:2025-09-30 -
Contact:Wang Haixia, PhD, Associate professor, Department of Traditional Chinese Medicine, Affiliated Hospital of Shandong Second Medical University, Weifang 261053, Shandong Province, China -
About author:Chen Ping, MS candidate, Technician in charge, Rehabilitation Medicine Center, Affiliated Hospital of Shandong Second Medical University, Weifang 261053, Shandong Province, China -
Supported by:Joint Science and Technology Project Task Book of Science and Technology Department, National Administration of Traditional Chinese Medicine, No. GZY-KJS-SD-2023-080 (to WHX)
CLC Number:
Cite this article
Chen Ping, Du Jinchao, Wang Hongying, Zhang Hui, Wang Haixia. Different inspiratory muscle training methods improve exercise and cardiopulmonary function of patients after cardiac surgery: a network meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3134-3144.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
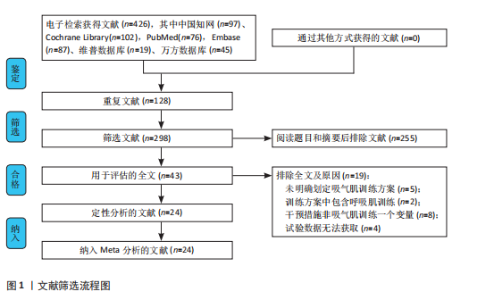
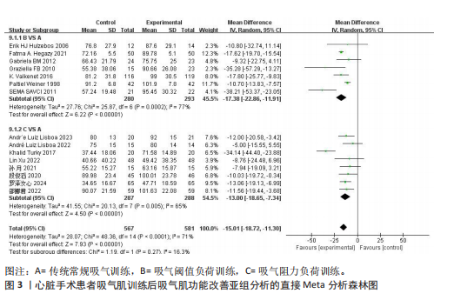
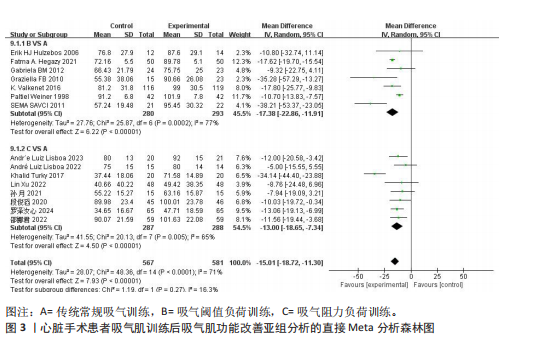
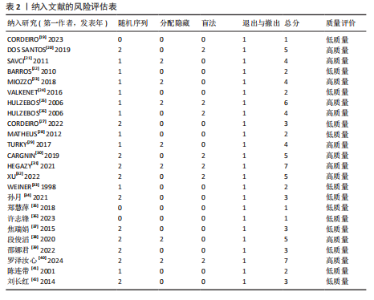
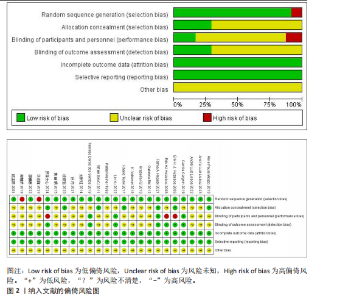
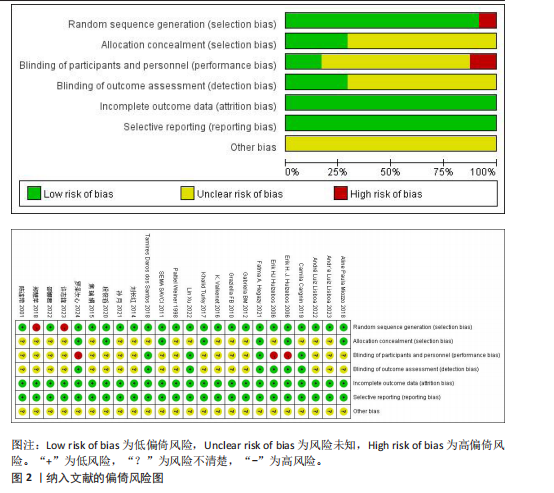
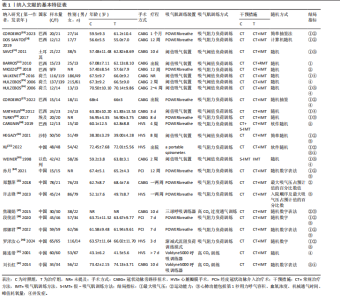
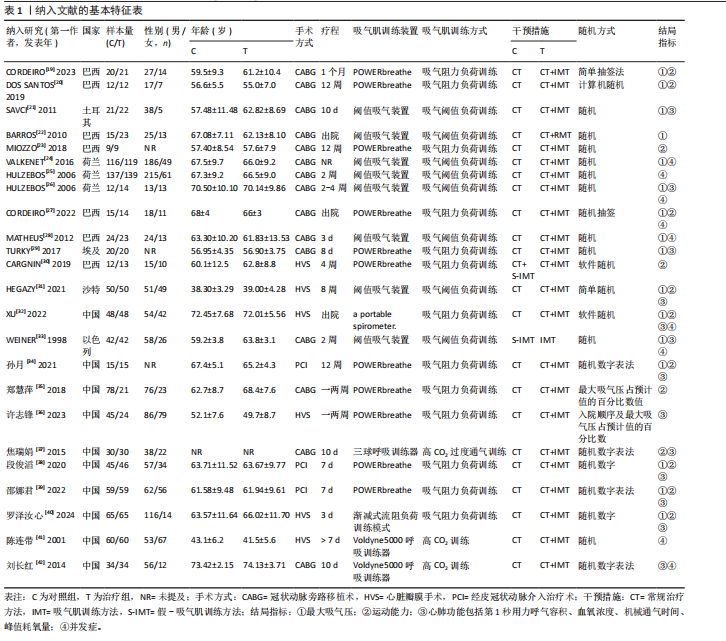
2.1 文献检索结果 初步检索得到426篇文献,经过阅读筛选后共纳入24篇文献[19-42]。具体筛选流程见图1。 2.2 纳入文献的基本特征与质量评估 2.2.1 纳入文献的基本特征 此次研究共纳入24篇随机对照试验,其中15篇为英文文献,9篇为中文文献。另外,此次研究共纳入1 907例研究对象,其中对照组984例,干预组923例。涉及6种吸气肌训练仪器,分别为POWER breathe呼吸训练器,阈值吸气装置,低阻力吸气肌训练,呼吸机内置训练模式,渐减式流阻负荷训练模式,Voldyne5000呼吸训练器。6种呼吸训练仪器按照训练机制共分为4种呼吸训练模式,分别为传统常规吸气肌训练、吸气阈值负荷训练、吸气阻力负荷训练、高CO2吸气训练。详见表1。 2.2.2 纳入文献的方法学质量评价 24篇文献均报道了分组方式,其中13篇文献报道了具体的随机方式[19-20,27,30-32,34-38,40,42],2篇采用随机抽签法[19,27],1篇文献以最大吸气压占预计值的百分比数值分组[35],1篇文献以入院顺序以及最大吸气压占预计值的百分比数值分组[36]。7篇文献报告了盲法的使用情况[20,25-26,30-32,40],其中4篇实施了双盲[20,30-32],3篇实施了单盲[25-26,40],所有随机对照试验均未报道其他偏倚。见图2。 根据修订版 Jadad 量表进行质量评价结果,1-3 分为低质量,4-7 分为高质量,结果显示高质量文献11篇[20-21,23,25-26,28,30-32,38,40],低质量文献13篇[19,22,24,27-28,33-37,39,41-42],平均3.54分,纳入文献总体质量较高。见表2。 2.3 吸气肌功能改善的Meta分析结果 2.3.1 直接Meta分析及异质性检验 共有15篇文献报道了最大吸气压的评分结果[19,21-22,24,26-29,31-34,38-40],共"
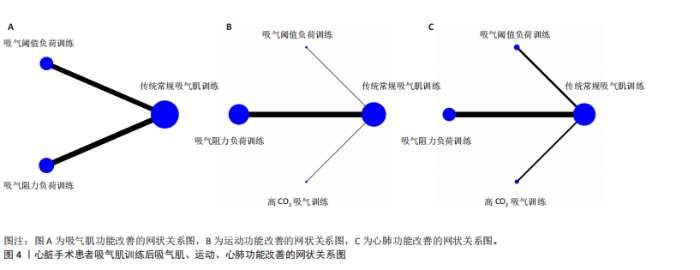
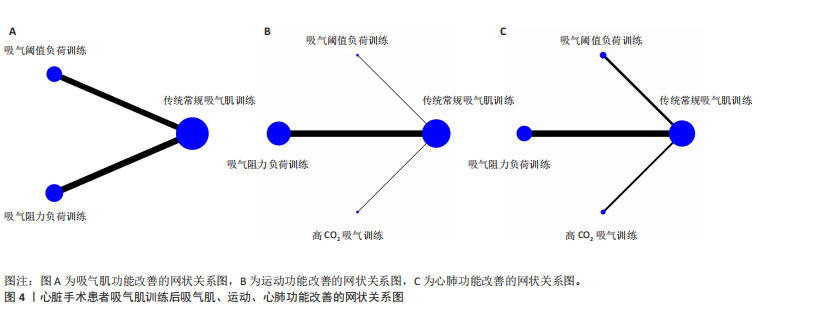
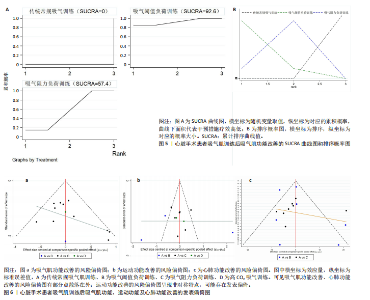
1 157例患者,各研究间异质性较高(I2=71%,P < 0.01),通过逐篇剔除文献的方法进行敏感性分析,异质性未发生明显改变,显示结果较为稳定,故对结果进行描述性分析,吸气肌功能训练能显著提高患者的吸气肌功能[MD=-15.01,95%CI(-18.72,-11.30),P < 0.01]。根据不同吸气肌训练模式进行亚组分析,与传统常规吸气肌训练相比,吸气阈值负荷训练[MD=-17.38,95%CI(-22.86,-11.91)]、吸气阻力负荷训练[MD=-13.00,95%CI(-18.65,-7.43)]均能够显著改善患者的吸气肌功能,且吸气阈值负荷训练的效应量优于吸气阻力负荷训练。见图3。 2.3.2 网状关系图 网状关系图包含3种吸气肌训练模式,分别为传统常规吸气肌训练方式、吸气阈值负荷训练方式7篇、吸气阻力负荷训练方式8篇,未形成闭环,见图4A。 2.3.3 网状Meta分析结果 在吸气肌功能改善方面,直接比较与间接比较共有3种结果,其中吸气阈值负荷训练、吸气阻力负荷训练与传统常规吸气训练疗效相比差异有显著性意义(P < 0.05);吸气阈值负荷训练与吸气阻力负荷训练疗效相比差异无显著性意义(P > 0.05)。见表3。 2.3.4 累积概率排序 在吸气肌功能改善方面,SUCRA值排序依次为吸气阈值负荷训练(92.6) > 吸气阻力负荷训练(57.4) > 传统常规吸气训练(0);概率高低依次为吸气阈值负荷训练、吸气阻力负荷训练、传统常规吸气训练。排序概率图显示吸气阈值负荷训练排序最高的概率最大,吸气阻力负荷训练次之,传统常规吸气训练再次之。见图5。 2.3.5 风险偏倚图 漏斗图显示,15篇文献分布呈非对称,3篇文献落于95%CI外。同时,Egger回归检验(P=0.16),提示纳入文章未存在明显的发表偏倚,见图6a。 2.4 运动功能改善的Meta分析结果 2.4.1 直接Meta分析及异质性检验 共有13篇文献报道了患者的运动能力[19-20,23,27,30-32,34-35,37-40],包含848例患者,各研究间异质性较高(I2=93%,"
P < 0.01),通过逐篇剔除文献的方法进行敏感性分析,发现异质性无明显降低,显示结果较为稳定,故采用随机效应模型对结果进行描述性分析,对照组与干预组间差异有显著性意义[SMD=-0.60,95%CI(-0.82,-0.38),P < 0.01]。根据吸气肌训练模式进行亚组分析,与传统常规吸气肌训练相比,3种吸气肌训练模式均能够显著改善患者的运动功能,且吸气阈值负荷训练效应量优于高CO2吸气训练优于吸气阻力负荷训练[SMD=-7.08,95%CI(-8.16,-6.01);SMD=-1.20,95%CI(-1.76,-0.65);SMD=-0.51,95%CI(-0.72,-0.31)]。见图7。 2.4.2 网状关系图 网状Meta分析共纳入13篇文献,包含4种吸气肌训练模式,分别为传统常规吸气肌训练"
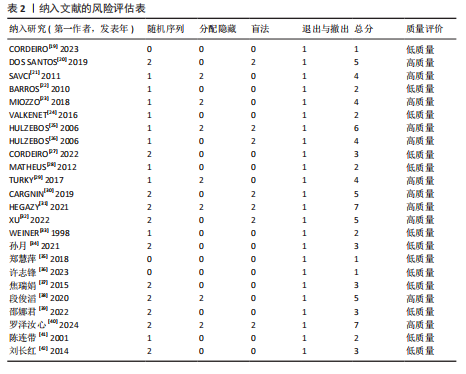
方式、吸气阈值负荷训练方式1篇、吸气阻力负荷训练方式11篇、高CO2吸气训练1篇,未形成闭环,见图4B。 2.4.3 网状Meta分析结果 在运动功能改善方面,直接比较与间接比较共有6种结果,其中吸气阈值负荷训练、吸气阻力负荷训练、高CO2吸气训练均与传统常规吸气训练相比疗效差异有显著性意义(P < 0.05);吸气阈值负荷训练与吸气阻力负荷训练相比、吸气阈值负荷训练与高CO2吸气训练相比、吸气阻力负荷训练与高CO2吸气训练相比疗效差异均有显著性意义(P < 0.05)。见表3。 2.4.4 累积概率排序 在运动功能改善方面,SUCRA值排序依次为吸气阈值负荷训练(100) > 高CO2吸气训练(66.4) > 吸气阻力负荷训练(33.6) > 传"
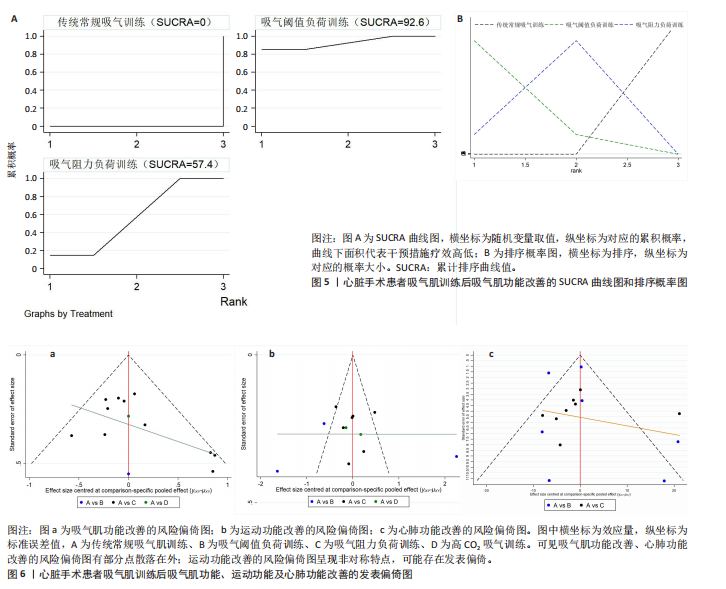
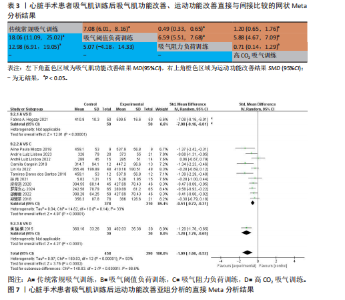
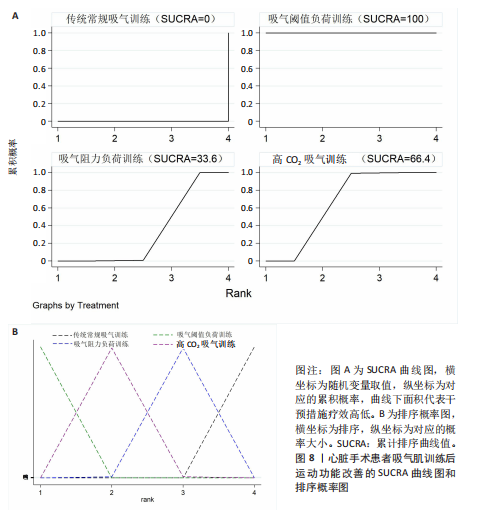
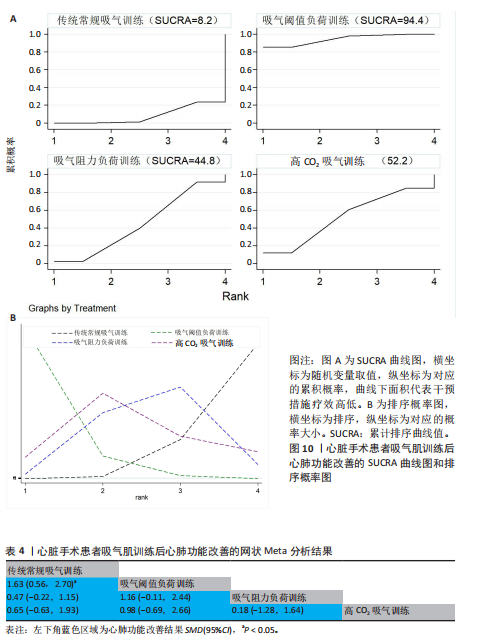
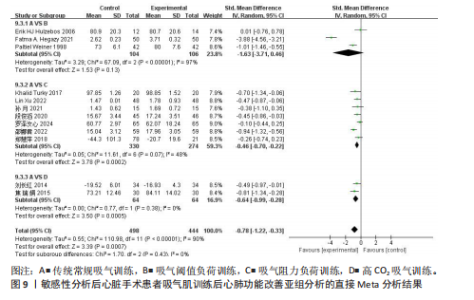
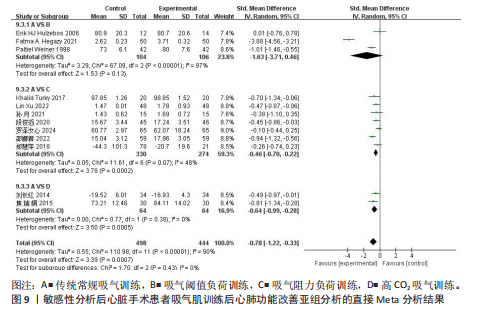
统常规吸气训练(0);概率高低依次为吸气阈值负荷训练、高CO2吸气训练、吸气阻力负荷训练、传统常规吸气训练。排序概率图显示吸气阈值负荷训练排序最高的概率最大,高CO2吸气训练、吸气阻力负荷训练、传统常规吸气训练次之。见图8。 2.4.5 风险偏倚图 漏斗图显示,13篇文献均位于漏斗内、呈非对称性。同时,Egger回归检验(P=0.04),提示纳入文章可能存在发表偏倚。见图6b。 2.5 心肺功能改善的Meta分析结果 2.5.1 直接Meta分析及异质性检验 共有13篇文献报道了患者的心肺功能情况[21,26,29,31-35,37-40,42],由于机械通气时间与其他3种数据的评分方向相反,故将机械通气时间的结果赋予“-”来表示。13篇文献包含942例患者,研究间异质性较高(I2=94%,P < 0.05),故选用随机效应模型合并分析,结果发现研究间的数据差异无显著性意义。通过逐篇剔除文献的方法进行敏感性分析,发现剔除SAVCI等[21]的文献后,对照组与干预组间差异有显著性意义[SMD=-0.66,95%CI(-1.26,-0.07),P=0.03],但是异质性仍较高(I2=94%,P < 0.05),因此根据吸气肌训练模式进行亚组分析,与传统常规吸气肌训练相比,吸气阻力负荷训练[SMD=-0.46,95%CI (-0.70,-0.22)]、高CO2吸气训练[SMD=-0.64,95%CI(-0.99,-0.28)]能够显著提高患者的心肺功能,而吸气阈值负荷训练的疗效改善无统计学意义。见图9。 2.5.2 网状关系图 剔除1篇文献后,网状Meta分析共纳入12篇文献,包含4种吸气肌训练方式,分别为传统常规吸气肌训练方式、吸气阈值负荷训练方式3篇、吸气阻力负荷训练方式7篇、高CO2吸气训练2篇,未形成闭环,见图4C。 2.5.3 网状Meta分析结果 在心肺功能改善方面,直接比较与间接比较共有6种结果,除吸气阈值负荷训练与传统常规吸气训练相比疗效差异有显著性意义外(P < 0.05),其余5种比较结"
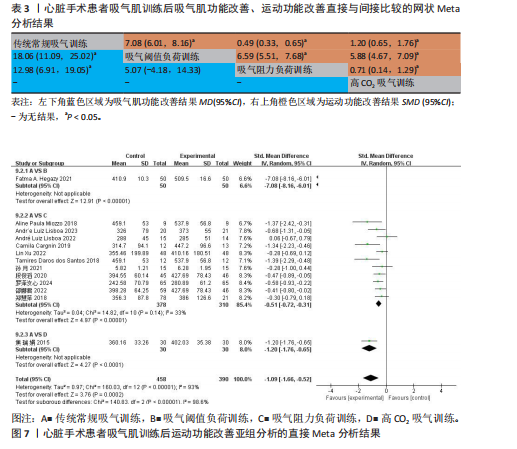
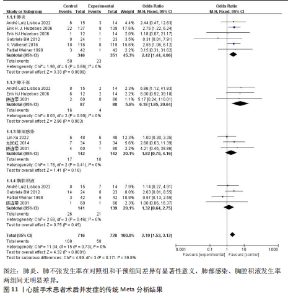
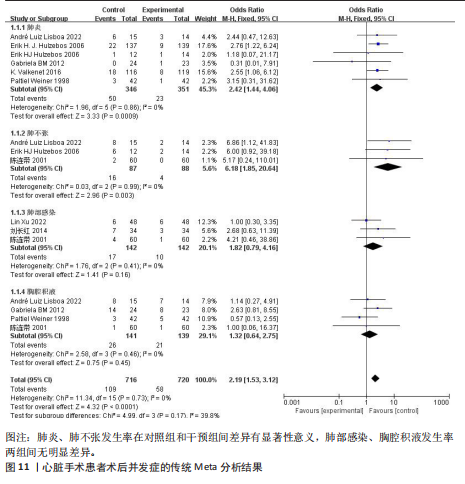
果均无统计学意义(P > 0.05)。见表4。 2.5.4 累积概率排序 在心肺功能改善方面,SUCRA值排序依次为吸气阈值负荷训练(94.4) > 高CO2吸气训练(52.2) > 吸气阻力负荷训练(44.8) > 传统常规吸气训练(8.2);概率高低依次为吸气阈值负荷训练、高CO2吸气训练、吸气阻力负荷训练、传统常规吸气训练。排序概率图显示吸气阈值负荷训练排序最高的概率最大,高CO2吸气训练、吸气阻力负荷训练、传统常规吸气训练次之。见图10。 2.5.5 风险偏倚图 漏斗图显示,5篇文献落于95%CI外,且12篇研究分布非对称。Egger回归检验(P=0.27),提示纳入文章未存在明显的发表偏倚,见图6c。 2.6 术后并发症的Meta分析结果 6篇文章报道了肺炎发生率[24-28,33],异质性分析结果为I2=0%,采用固定效应模型,干预组发生率低于对照组[OR=2.42,95%CI(1.44,4.06)],且差异有显著性意义(P < 0.01)。 4篇文献报道了肺不张发生率[26-28,41],异质性分析结果为I2=75%,通过逐篇剔除文献进行敏感性分析发现异质性来源于MATHEUS等[28]的文献,剔除后异质性显著降低(I2=0%),这可能是由于该研究的肺不张发生率差异无显著性意义。采用固定效应模型,干预组发生率低于对照组[OR=6.18,95%CI(1.85,20.64)],且差异有显著性意义(P < 0.01)。 3篇文章报道了肺部感染发生率[32,41-42],异质性分析结果为I2=0%,采用固定效应模型,干预组与对照组间差异无显著性意义[P=0.16,OR=1.82,95%CI(0.79,4.16)]。 4篇文章报道了胸腔积液发生率[27-28,33,41],异质性分析结果为I2=0%,采用固定效应模型,干预组与对照组间差异无显著性意义[P=0.45,OR=1.32,95%CI(0.64,2.75)]。见图11。"
| [1] ROTH GA, MENSAH GA, JOHNSON CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982-3021. [2] World Health Organization (WHO). Cardiovascular Disease [Internet]. 2018. [cited 2019 Mar. 1]. Available from:http://www.who.int/en/ news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). [3] PARK JW, OH JC, LEE JW, et al. The effect of 5Hz high-frequency rTMS over contralesional pharyngeal motor cortex in post-stroke oropharyngeal dysphagia: a randomized controlled study. Neurogastroenterol Motil. 2013;25(4): 250-324. [4] LAOHACHAI K, WINLAW D, SELVADURAI H, et al. Inspiratory muscle training is associated with improved inspiratory muscle strength, resting cardiac output, and the ventilatory efficiency of exercise in patients with a fontan circulation. J Am Heart Assoc. 2017;6(8): e005750 [5] NISSINEN J, BIANCARI F, WISTBACKA JO, et al. Safe time limits of aortic cross-clamping and cardiopulmonary bypass in adult cardiac surgery. Perfusion. 2009;24(5):297-305. [6] GUIZILINI S, GOMES WJ, FARESIN SM, et al. Evaluation of pulmonary function in patients following on and off-pump coronary artery bypass grafting. Braz J Cardiovasc Surg. 2005;20(3). doi: 10.1590/s1678-97412005000300013. [7] MISKOVIC A, LUMB AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118(3):317-334. [8] 冯梦月. 吸气肌训练对肺移植患者肺功能、膈肌功能和运动能力的影响[D]. 南京:南京体育学院,2023. [9] STEIN R, MAIA CP, SILVEIRA AD, et al. Inspiratory muscle strength as a determinant of functional capacity early after coronary artery bypass graft surgery. Arch Phys Med Rehabil. 2009;90(10):1685-1691. [10] 罗泽汝心, 王渝强, 周亚馨, 等. 术前吸气肌训练预防成人心脏手术患者术后肺部并发症的最新进展[J]. 中国胸心血管外科临床杂志,2023,30(10):1519-1523. [11] 郑静, 李宝宝, 杨丽娟. 吸气肌训练预防心脏手术后患者肺部并发症的研究进展[J]. 上海护理,2020,20(9):62-65. [12] KENDALL F, OLIVEIRA J, PELETEIRO B, et al. Inspiratory muscle training is effective to reduce postoperative pulmonary complications and length of hospital stay: a systematic review and meta-analysis. Disabil Rehabil. 2018;40(8):864-882. [13] ZHANG S, LI B, MENG X, et al. The Effects of Inspiratory Muscle Training (IMT) on Patients Undergoing Coronary Artery Bypass Graft (CABG) Surgery: A Systematic Review and Meta-Analysis. Rev Cardiovasc Med. 2023;24(1):16. [14] XIANG Y, ZHAO Q, LUO T, et al. Inspiratory muscle training to reduce risk of pulmonary complications after coronary artery bypass grafting: a systematic review and meta-analysis. Front Cardiovasc Med. 2023;10: 1223619. [15] AQUINO TN, PRADO JP, CRISAFULLI E, et al. Efficacy of Respiratory Muscle Training in the Immediate Postoperative Period of Cardiac Surgery: A Systematic Review and Meta-Analysis. Braz J Cardiovasc Surg. 2024;39(1):e20220165. [16] LISBOA CAL, OLIVEIRA SL, MANSUETO G, et al. Inspiratory Muscle Training in Patients in the Postoperative Phase of Cardiac Surgery: A Systematic Review and Meta-Analysis. Ann Rehabil Med. 2023;47(3):162-172. [17] Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [18] 柳青, 翟伟, 谭亚芹, 等. 临床研究文献质量评价工具浅析[J]. 中国针灸,2014, 34(9):919-922. [19] CORDEIRO ALL, ALMEIDA DE BRITO J, RODRIGUES PEREIRA L, et al. Inspiratory muscle training on quality of life and functional capacity after hospital discharge in patients submitted to coronary artery bypass grafting: A controlled clinical trial. J Bodyw Mov Ther. 2023;35:202-207. [20] DOS SANTOS TD, PEREIRA SN, PORTELA LOC, et al. Moderate-to-high intensity inspiratory muscle training improves the effects of combined training on exercise capacity in patients after coronary artery bypass graft surgery: A randomized clinical trial. Int J Cardiol. 2019;279:40-46. [21] SAVCI S, DEGIRMENCI B, SAGLAM M, et al. Short-term effects of inspiratory muscle training in coronary artery bypass graft surgery: a randomized controlled trial. Scand Cardiovasc J. 2011;45(5):286-293. [22] BARROS GF, SANTOS CDA S, GRANADO FB, et al. Respiratory muscle training in patients submitted to coronary arterial bypass graft. Rev Bras Cir Cardiovasc. 2010;25(4):483-490. [23] MIOZZO AP, STEIN C, MARCOLINO MZ, et al. Effects of High-Intensity Inspiratory Muscle Training Associated with Aerobic Exercise in Patients Undergoing CABG: Randomized Clinical Trial. Braz J Cardiovasc Surg. 2018; 33(4):376-383. [24] VALKENET K, TRAPPENBURG JCA, HULZEBOS EH, et al. Effects of a pre-operative home-based inspiratory muscle training programme on perceived health-related quality of life in patients undergoing coronary artery bypass graft surgery. Physiotherapy. 2017;103(3):276-282. [25] HULZEBOS EH, HELDERS PJ, FAVIÉ NJ, et al. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA. 2006;296(15): 1851-1857. [26] HULZEBOS EH, VAN MEETEREN NL, VAN DEN BUIJS BJ, et al. Feasibility of preoperative inspiratory muscle training in patients undergoing coronary artery bypass surgery with a high risk of postoperative pulmonary complications: a randomized controlled pilot study. Clin Rehabil. 2006;20(11):949-959. [27] CORDEIRO ALL, CARVALHO BSC, SILVA EGD, et al. Inspiratory muscle training and functional capacity following coronary artery bypass grafting in high-risk patients: A pilot randomized and controlled trial. J Clin Transl Res. 2022;8(4):266-271. [28] MATHEUS GB, DRAGOSAVAC D, TREVISAN P, et al. Treinamento muscular melhora o volume corrente e a capacidade vital no pós-operatório de revascularização do miocárdio Inspiratory muscle training improves tidal volume and vital capacity after CABG surgery. Braz J Cardiovasc Surg. 2012;27(3):362-369. [29] TURKY K, AFIFY AMA. Effect of Preoperative Inspiratory Muscle Training on Alveolar-Arterial Oxygen Gradients After Coronary Artery Bypass Surgery. J Cardiopulm Rehabil Prev. 2017;37(4):290-294. [30] CARGNIN C, KARSTEN M, GUARAGNA JCVDC, et al. Inspiratory Muscle Training After Heart Valve Replacement Surgery Improves Inspiratory Muscle Strength, Lung Function, and Functional Capacity: A randomized controlled trial. J Cardiopulm Rehabil Prev. 2019;39(5):E1-E7. [31] HEGAZY FA, MOHAMED KAMEL SM, ABDELHAMID AS, et al. Effect of postoperative high load long duration inspiratory muscle training on pulmonary function and functional capacity after mitral valve replacement surgery: A randomized controlled trial with follow-up. PLoS One. 2021;16(8):e0256609. [32] XU L, WEI J, LIU J, et al. Inspiratory muscle training improves cardiopulmonary function in patients after transcatheter aortic valve replacement: a randomized clinical trial. Eur J Prev Cardiol. 2023;30(2):191-202. [33] WEINER P, ZEIDAN F, ZAMIR D, et al. Prophylactic inspiratory muscle training in patients undergoing coronary artery bypass graft. World J Surg. 1998;22(5):427-431. [34] 孙月, 田妍卉, 林碧莹, 等. 使用POWER-breathe进行吸气肌训练对PCI术后患者心肺功能的影响[J]. 中国老年保健医学, 2021,19(3):21-23. [35] 郑慧萍, 鲁胜男, 张喆. 术前呼吸肌训练对吸气肌无力者冠状动脉旁路移植术预后的影响[J]. 临床心血管病杂志,2018, 34(3):272-275. [36] 许志锋, 吴桂琴, 吴永前, 等. 术前呼吸肌训练对心脏瓣膜置换术吸气肌无力患者预后的影响[J]. 岭南心血管病杂志, 2023,29(4):380-384. [37] 焦瑞娟, 马亚飞, 史素玲, 等. 吸气肌训练对冠状动脉旁路移植术后心肺功能和生活质量的影响: 中国转化医学和整合医学学术交流会(上海站),中国上海, 2015[C]. [38] 段俊滔, 刘聪颖, 于桂香, 等. 吸气肌训练对经皮冠状动脉介入治疗术后患者的影响研究[J]. 中华护理杂志,2020,55(4): 519-523. [39] 邵娜君, 吴惠霞, 黄贞敏, 等. 吸气肌训练在经皮冠状动脉介入治疗术患者中的应用效果[J]. 当代护士(上旬刊),2022, 29(6):123-126. [40] 罗泽汝心, 王渝强, 周亚馨, 等. 有限资源下创新性吸气肌训练方案对心脏瓣膜疾病患者术后肺部并发症的影响[J]. 中国康复医学杂志,2024,39(1):39-44. [41] 陈连带,叶庆新. 呼吸训练器对心脏瓣膜置换术后康复作用的探讨[J]. 现代康复,2001(8):151. [42] 刘长红, 张一明. 深呼吸训练器在高龄冠状动脉旁路移植术患者围术期中的应用[J]. 中国康复医学杂志,2014,29(11):1077-1078. [43] 郭佳宝, 朱毅. 吸气肌训练的临床研究进展[J]. 中国康复医学杂志, 2014,29(9): 888-892. [44] 岳明叶, 王慧华, 胡玉婷, 等. 吸气肌训练促进心脏手术病人肺康复的研究进展[J]. 护理研究,2022,36(5):858-863. [45] CAVAYAS YA, ELJAIEK R, RODRIGUE É, et al. Preoperative Diaphragm Function Is Associated With Postoperative Pulmonary Complications After Cardiac Surgery. Crit Care Med. 2019;47(12):e966-e974. [46] 王一木, 王灵雨, 刘靖宇, 等. 吸气肌训练对心脏外科手术患者干预效果的Meta分析[J]. 实用心脑肺血管病杂志, 2025,33(5):101-109. [47] MONERUZZAMAN M, SUN WZ, CHANGWE GJ, et al. Efficacy of Multiple Exercise Therapy after Coronary Artery Bypass Graft: A Systematic Review of Randomized Control Trials. Rev Cardiovasc Med. 2023;24(5):141. [48] 梅桃桃, 刘扣英. 慢性阻塞性肺疾病患者吸气肌训练的研究进展[J]. 护理学杂志, 2013,28(23):72-75. [49] GEDDES EL, O’BRIEN K, REID WD, et al. Inspiratory muscle training in adults with chronic obstructive pulmonary disease: an update of a systematic review. Respir Med. 2008;102(12):1715-1729. [50] 常影, 刘泽雄, 季晓鹏, 等. 体外循环肺损伤机制与肺保护策略研究进展[J]. 长春中医药大学学报,2023,39(7):817-821. [51] MONERUZZAMAN M, SUN WZ, CHANGWE GJ, et al. Efficacy of Multiple Exercise Therapy after Coronary Artery Bypass Graft: A Systematic Review of Randomized Control Trials. Rev Cardiovasc Med. 2023;24(5):141. [52] SAMEED M, CHOI H, AURON M, et al. Preoperative Pulmonary Risk Assessment. Respir Care. 2021;66(7):1150-1166. [53] JEONG BH, SHIN B, EOM JS, et al. Development of a prediction rule for estimating postoperative pulmonary complications. PLoS One. 2014;9(12): e113656. [54] WINKELMANN ER, STEFFENS É, WINDMÖLLER P, et al. Preoperative expiratory and inspiratory muscle weakness to predict postoperative outcomes in patients undergoing elective cardiac surgery. J Card Surg. 2020;35(1):128-134. |
| [1] | Cao Xinyan, Yu Zifu, Leng Xiaoxuan, Gao Shiai, Chen Jinhui, Liu Xihua. Effect of repetitive transcranial magnetic stimulation and transcranial direct current stimulation on motor function and gait in children with cerebral palsy: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(6): 1539-1548. |
| [2] | Chen Qiang, Wu Wenjuan, Jiang Shuhua, Huang Da. Physical exercise improves physical function in burn patients: a systematic review and meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(5): 1269-1281. |
| [3] | Hou Bing, Zhao Hongfei, Che Pengcheng, Wang Ziyi, Gao Zan, Chen Linyu, Wang Jinzhi, Dou Na. Analysis of upper limb motor function and brain function immediately and 3 weeks after transcranial direct current stimulation [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3066-3074. |
| [4] | Ma Shanxin, Zheng Jianling, Cheng Jian, Lin Xi, Li Qiuyuan, Wang Li, Zeng Yangkang, Song Luping. Early intelligent active assistance in walking for hemiplegic patients under suspension protection: #br# a randomized controlled trial [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3075-3082. |
| [5] | Hu Xin, Wan Haili, Du Liang, Li Yongjie, Xia Yuan. Theta-stimulation for the treatment of motor function and daily activity ability in the lower extremities of stroke patients: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(10): 2576-2583. |
| [6] | Tao Zihan, Saijilafu. Cycloastragenol promotes motor function recovery and cortical neuron regeneration in mice with spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(20): 4258-4265. |
| [7] | Liu Xingzhao, Hu Tong, Ma Yan, Wang Qian, Wei Xiaohui, Chang Wanpeng, Yu Shaohong. Efficacy of rehabilitation robots on lower limb motor function in patients with cerebral palsy: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(18): 3925-3933. |
| [8] | Wang Ke, Wang Lei, Li Wenshan, Gong Weijun . Application prospect of brain-computer interface technology in the rehabilitation of lower limb function in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(14): 3027-3033. |
| [9] | Song Haiwang, Jiang Guanhua, Mu Yingying, Fu Shanyu, Sun Baofei, Li Yumei, Yu Zijiang, Yang Dan. Repetitive trans-spinal magnetic stimulation promotes motor function recovery in mice after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(11): 2252-2260. |
| [10] | Zhou Bangyu, Li Jie, Ruan Yushang, Geng Funeng, Li Shaobo. Effects of Periplaneta americana powder on motor function and autophagic protein Beclin-1 in rats undergoing spinal cord hemisection [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1223-1228. |
| [11] | Zhang Ming, Wang Bin, Jia Fan, Chen Jie, Tang Wei. Application of brain-computer interface technology based on electroencephalogram in upper limb motor function rehabilitation of stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 581-586. |
| [12] | Chang Wanpeng, Zhang Zhongwen, Yang Yulin, Zi Yang, Yang Mengqi, Du Bingyu, Wang Nan, Yu Shaohong. Efficacy of rehabilitation exoskeleton robots on post-stroke lower limb motor dysfunction: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(2): 321-328. |
| [13] | Yang Yulin, Chang Wanpeng, Ding Jiangtao, Xu Hongli, Wu Xiao, Xiao Boheng, Ma Lihong. Transcranial direct current stimulation at different targets for Parkinson’s disease: a network Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(11): 1797-1804. |
| [14] | Du Kairan, Deng Qiang, Guo Tiefeng, Zhang Yanjun, Peng Randong, Li Junjie, Wang Yurong, Zhang Kaidong, Luo Linzhao. Improved laminectomy for constructing a rat model of spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(32): 5173-5177. |
| [15] | Liu Xinhao, Ma Xinran, Yang Shengyong, Wang Yanyu, Ma Shujie. Influence of Tuina manipulation on walking dysfunction in rats with sciatic nerve injury [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(26): 4101-4106. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||