Chinese Journal of Tissue Engineering Research ›› 2026, Vol. 30 ›› Issue (12): 3075-3082.doi: 10.12307/2026.664
Previous Articles Next Articles
Early intelligent active assistance in walking for hemiplegic patients under suspension protection: #br# a randomized controlled trial
Ma Shanxin1, Zheng Jianling2, Cheng Jian1, Lin Xi1, Li Qiuyuan1, Wang Li1, Zeng Yangkang1, Song Luping3
- 1Department of Rehabilitation Medicine, Shenzhen University General Hospital, Shenzhen 518055, Guangdong Province, China; 2Department of Physical Therapy, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing 100068, China; 3Department of Rehabilitation Medicine, Shenzhen Nanshan People’s Hospital, Shenzhen 518300, Guangdong Province, China
Ma Shanxin, MS, Associate chief physician, Department of Rehabilitation Medicine, Shenzhen University General Hospital, Shenzhen 518055, Guangdong Province, China
-
Received:2025-04-02Accepted:2025-08-06Online:2026-04-28Published:2025-09-30 -
Contact:Song Luping, PhD, Chief physician, Department of Rehabilitation Medicine, Shenzhen Nanshan People’s Hospital, Shenzhen 518300, Guangdong Province, China -
About author:Zheng Jianling, Department of Physical Therapy, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing 100068, China Ma Shanxin and Zheng Jianling contributed equally to this work. -
Supported by:Shenzhen Nanshan District Science and Technology Development Plan Project, No. NS2022150 (to MSX)
CLC Number:
Cite this article
Ma Shanxin, Zheng Jianling, Cheng Jian, Lin Xi, Li Qiuyuan, Wang Li, Zeng Yangkang, Song Luping. Early intelligent active assistance in walking for hemiplegic patients under suspension protection: #br# a randomized controlled trial[J]. Chinese Journal of Tissue Engineering Research, 2026, 30(12): 3075-3082.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
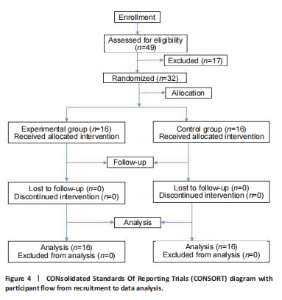
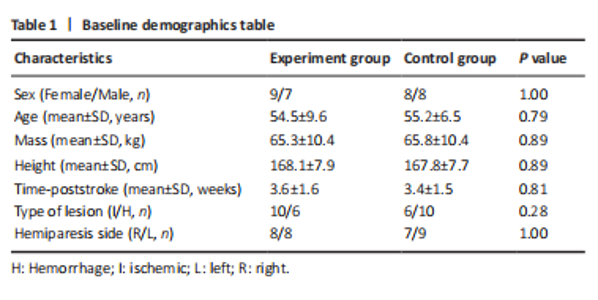
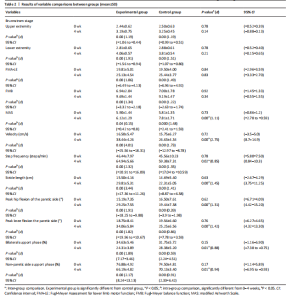
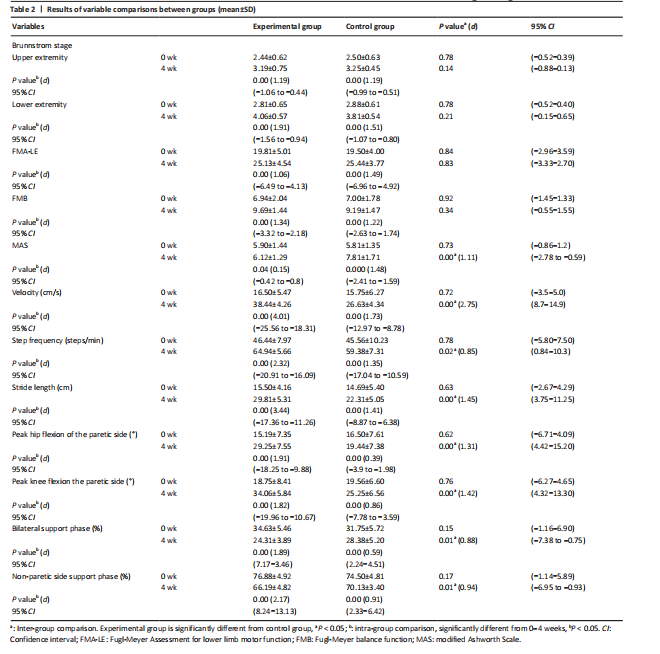
Results The number of subjects included in the study A total of 49 patients with early-stage stroke were screened, of whom 32 met the eligibility criteria and were randomized to undergo the intervention, as illustrated in Figure 4. A comparison of baseline characteristics, presented in Tables 1 and 2, revealed no statistically significant differences in demographic or clinical features among the participants (P > 0.05). "
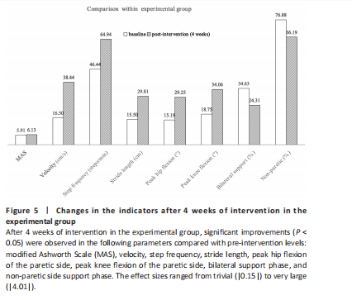
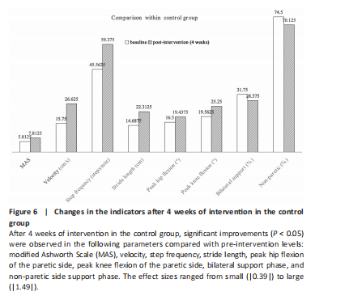
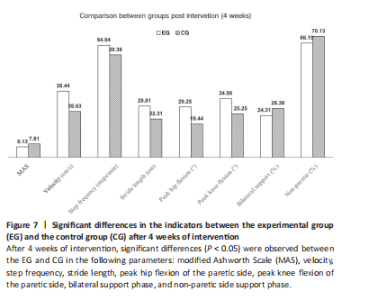
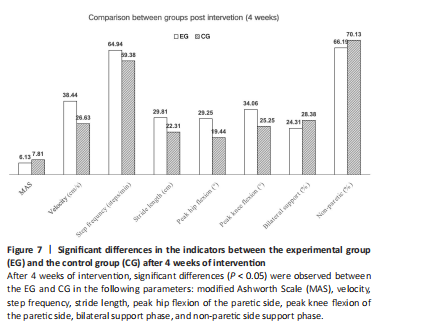
Analysis of differences in outcome indicators among groups of subjects Changes in the indicators after 4 weeks of intervention in the control group and experimental group are shown in Figures 5–7. After 4 weeks, the MAS scores exhibited minimal changes in both groups. The experimental group showed a slight but statistically significant increase (from 5.91 to 6.13, P < 0.05, d=|0.15|), whereas the control group demonstrated a substantial increase (from 5.81 to 7.81, P < 0.05, d=|1.48|). Post-intervention, the MAS scores in the control group were significantly higher than those in the experimental group (7.81 vs. 6.13, P < 0.05, d=|1.11|). Among the spatiotemporal gait parameters assessed, the experimental group displayed highly significant and clinically meaningful improvements in gait velocity (from 16.5 to 38.44 cm/s, P < 0.05, effect size d=|4.01|), step frequency (from 46.44 to 64.94 steps/min, P < 0.05, d=|2.32|), and stride length (from 15.50 to 29.81 cm, P < 0.05, d=|3.44|). In contrast, the control group exhibited changes of greater magnitude but with moderate effect sizes (d=|1.35| to |1.73|) for the same parameters post-intervention."
Both groups demonstrated statistically significant improvements in peak flexion angles of the hip and knee joints (P < 0.05), along with significant reductions in both bilateral and non-paretic support phases (P 0.05). Following a 4-week intervention, the EG demonstrated statistically significant improvements in gait parameters compared to the CG. Specifically, EG exhibited a 28.6% increase in walking velocity (from 26.63 cm/s to 38.44 cm/s; P < 0.05), with a very large treatment effect size (d=|2.75|). Additionally, EG showed significant and substantial increases in other kinematic outcomes: Stride length increased by 25.3% (from 22.31 cm to 29.81 cm; P < 0.05, d=|1.45|), peak hip flexion improved by 33.5% (from 19.44° to 29.25°; P < 0.05, d=|1.31|), and peak knee flexion increased by 25.9% (from 25.25° to 34.06°; P < 0.05, d = 1.42). Moderate yet statistically significant differences were observed in temporal-spatial parameters. Specifically, step frequency exhibited a significant increase (64.94 steps/min vs. 59.38 steps/min; P < 0.05, d=|0.85|). Concurrently, the support phase decreased significantly: bilaterally, it was reduced from 28.375% to 24.31% (P < 0.05, d=|0.88|), and in the non-paretic side, it decreased from 70.13% to 66.19% (P < 0.05, d=|0.94|). Adverse reaction analysis None of the test subjects experienced adverse reactions during the trial."

| [1] FEIGIN VL, BRAININ M, NORRVING B, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022;17(1):18-23. [2] MALIK AN, TARIQ H, AFRIDI A, et al. Technological advancements in stroke rehabilitation. J Pak Med Assoc. 2022;72(8):1672-1674. [3] MORI H, TAMARI M, MARUYAMA H. Relationship between walking ability of patients with stroke and effect of body weight-supported treadmill training. J Phys Ther Sci. 2020;32(3):206-209. [4] MEHRHOLZ J, T HOMAS S, KUGLER J, et al. Electromechanical-assisted training for walking after stroke. Cochrane Database Syst Rev. 2020;10(10):CD006185. [5] HSU CY, CHENG YH, LAI CH, et al. Clinical non-superiority of technology-assisted gait training with body weight support in patients with subacute stroke: a meta-analysis. Ann Phys Rehabil Med. 2020;63(6):535-542. [6] GIOYANNINI S, IACOVELLI C, BRAE F, et al. Robotic-assisted rehabilitation for balance and gait in stroke patients (ROAR-S): study protocol for a preliminary randomized controlled trial. Trials. 2022;23(1):872. [7] DE MIGUEL-FERNÁNDEZ J, LOBO-PRAT J, PRINSEN E, et al. Control strategies used in lower limb exoskeletons for gait rehabilitation after brain injury: a systematic review and analysis of clinical effectiveness. J Neuroeng Rehabil. 2023;(20):23. [8] NAKAJIMA T, SANKAI Y, TAKATA S, et al. Cybernic treatment with wearable cyborg Hybrid Assistive Limb (HAL) improves ambulatory function in patients with slowly progressive rare neuromuscular diseases: a multicentre, randomised, controlled crossover trial for efficacy and safety (NCY-3001). Orphanet J Rare Dis. 2021;16(1):304. [9] NADOERF F, WRIGHT MA, LOPEZ-MATAS H, et al. User-centered design of a personal-use exoskeleton: a clinical investigation on the feasibility and usability of the ABLE exoskeleton device for individuals with spinal cord injury to perform skills for home and community environments. Front Neurosci. 2024;18:1437358. [10] BATTAGLIA M, BORG MB, LORO A, et al. post-stroke spasticity: follow-up and functional implications of chronic long-term treatment with botulinum toxin. Eur J Phys Rehabil Med. 2024;60(4):581-590. [11] BAYLE N, MAISONOBE P, RAYMOND R, et al. Composite active range of motion (CXA) and relationship with active function in upper and lower limb spastic paresis. Clin Rehabil. 2020;34(6):803-811. [12] CHERNI Y, HAJIZADEH M, DAL MASO F, et al. Effects of body weight support and guidance force settings on muscle synergy during Lokomat walking. Eur J Appl Physiol. 2021;121(11):2967-2980. [13] Förster A, Gass A, Kern R, et al. Brain imaging in patients with transient ischemic attack: a comparison of computed tomography and magnetic resonance imaging. Eur Neurol. 2012;67(3):136-141. [14] RIZVI MR, SHARNMA A, MALKI A, et al. Enhancing cardiovascular health and functional recovery in stroke survivors: a randomized controlled trial of stroke-specific and cardiac rehabilitation protocols for optimized rehabilitation. J Clin Med. 2023;12(20):6589. [15] LI L, LIU R, HE J, et al. Effects of threshold respiratory muscle training on respiratory muscle strength, pulmonary function and exercise endurance after stroke: a meta-analysis. J Stroke Cerebrovasc Dis. 2024:33(8):107837. [16] SCHRODER J, TRUIJERN S, VANRIEKNGE T, et al. Feasibility and effectiveness of repetitive gait training early after stroke: a systematic review and meta-analysis. J Rehabil Med. 2019;51(2):78-88. [17] LIANG S, HONG ZQ, CAI Q, et al. Effects of robot-assisted gait training on motor performance of lower limb in poststroke survivors: a systematic review with meta-analysis. Eur Rev Med Pharmacol Sci. 2024;28(3):879-898. [18] JOHNSTON TE, KELLER S, DENZER-WEILER C, et al. A clinical practice guideline for the use of ankle-foot orthoses and functional electrical stimulation post-stroke. J Neurol Phys Ther. 2021;45:112-196. [19] LEE Y, KIM GB, SHIN S. Association between lower limb strength asymmetry and gait asymmetry: implications for gait variability in stroke survivors. J Clin Med. 2025;14(2):380. [20] SEO JW, KANG GH, KIM CH, et al. Characteristics of gait event and muscle activation parameters of the lower limb on the affected side in patients with hemiplegia after stroke: a pilot study. Arch Rehabil Res Clin Transl. 2023;5(4): 100274. [21] SENDA J, ITO K, KOTAKE T, et al. Investigation of inpatient convalescent rehabilitation outcomes in branch atheromatous disease. J Stroke Cerebrovasc Dis. 2023;32(3):106937. [22] ZHIYAN H, NIN L, BAOYUN C, et al. Rehabilitation nursing for cerebral stroke patients within a suitable recovery empty period. Iran J Public Health. 2017; 46(2):180-185. [23] MAO HF, HSUEH IP, Tang PF, et al. Analysis and comparison of the psychometric properties of three balance measures for stroke patients. Stroke. 2002;33(4):1022-1027. [24] HERNAN ED, FORERO SM, GALEANO CP, et al. Intra and inter-rater reliability of Fugl-Meyer assessment of lower extremity early after stroke. Braz J Phys Ther. 2021;25(6):709-718. [25] BOHANNON RW, SMITH MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206-207. [26] PISCITELLI D, PELLICCIARI L, VIDMAR T, et al. Is it time to go beyond the modified ashworth scale? Letter to the editor on “reliability of the modified Ashworth scale after stroke for 13 muscle groups”. Arch Phys Med Rehabil. 2023;104(10): 1735-1736. [27] VIDMAR T, GOLJAR KN, PUH U. Reliability of the modified ashworth scale after stroke for 13 muscle groups. Arch Phys Med Rehabil. 2023; 104(10):1606-1611. [28] GILLESPIE J, ARNOLD D, TRAMMELL M, et al. Utilization of overground exoskeleton gait training during inpatient rehabilitation: a descriptive analysis. J Neuroeng Rehabil. 2023;20(1):102. [29] BATTERHAM AM, HOPKINS WG. Making meaningful inferences about magnitudes. Int J Sports Physiol Perform. 2006;1(1):50-57. [30] SKVORTSOV DV, KAURKIN SN, IVANOVA GE. Targeted biofeedback training to improve gait parameters in subacute stroke patients: a single-blind randomized controlled trial. Sensors (Basel). 2024;24(22):7212. [31] MAZZUCCHELLI M, MAZZOLENI D, CAMPANINI I, et al. Evidence-based improvement of gait in post-stroke patients following robot-assisted training: a systematic review. NeuroRehabilitation. 2022;51(4):595-608. [32] HUBER J, ELWERTl N, POWELL ES, et al. Effects of dynamic body weight support on functional independence measures in acute ischemic stroke: a retrospective cohort study. J Neuroeng Rehabil. 2023;20(1):6. [33] MEYER A, H RDLICKA HC, CUTLER E, et al. A novel body weight-supported postural perturbation module for gait and balance rehabilitation after stroke: preliminary evaluation study. JMIR Rehabil Assist Technol. 2022; 9(1):e31504. [34] NAGHDI S, A NSARI NN, RASTGOO M, et al. A pilot study on the effects of low frequency repetitive transcranial magnetic stimulation on lower extremity spasticity and motor neuron excitability in patients after stroke. J Bodyw Mov Ther. 2015;19(4):616-623. [35] CHEN S, Z HANGh W, WANG D, et al. How robot-assisted gait training affects gait ability, balance and kinematic parameters after stroke: a systematic review and meta-analysis. Eur J Phys Rehabil Med. 2024;60(3):400-411. [36] XU P, HUANG Y, WANG J, et al. Repetitive transcranial magnetic stimulation as an alternative therapy for stroke with spasticity: a systematic review and meta-analysis. J Neurol. 2021;268(11):4013-4022. [37] KOLDAS D OGAN Ş. Robot-assisted gait training in stroke. Turk J Phys Med Rehabil. 2024;70(3):293-299. [38] MA ZZ, WU JJ, HUA XY, et al. Evidence of neuroplasticity with brain-computer interface in a randomized trial for post-stroke rehabilitation: a graph-theoretic study of subnetwork analysis. Front Neurol. 2023;14: 1135466. [39] DELUCA C, MORETTO G, DI MATTEO A, et al. Hemi-and monoataxia in cerebellar hemispheres and peduncles stroke lesions: topographical correlations. Cerebellum. 2012;11(4):917-924. [40] KAYABINAR B, ALEMDAROGLU-GURBUZ İ, YILMAZ Ö. The effects of virtual reality augmented robot-assisted gait training on dual-task performance and functional measures in chronic stroke: a randomized controlled single-blind trial. Eur J Phys Rehabil Med. 2021;57(2):227-237. [41] DATTOLA R, GIRLANDA P, VITA G, et al. Muscle rearrangement in patients with hemiparesis after stroke: an electrophysiological and morphological study. Eur Neurol. 1993;33(2):109-114. [42] HERING GO, BERTSCHINGER R, STEOPAN J. A quadriceps femoris motor pattern for efficient cycling. PLoS One. 2023;18(3):e0282391. [43] WLODARCZYK L, CICHON N, SALUK-BIJAK J, et al. Neuroimaging techniques as potential tools for assessment of angiogenesis and neuroplasticity processes after stroke and their clinical implications for rehabilitation and stroke recovery prognosis. J Clin Med. 2022;11(9):2473. [44] RUFF J, UDEH B, LINDER S. Cardiac rehabilitation for persons with stroke: a cost-effectiveness analysis. Clin Rehabil. 2025;39(2):153-160. |
| [1] | Haonan Yang, Zhengwei Yuan, Junpeng Xu, Zhiqi Mao, Jianning Zhang. Preliminary study on the mechanisms and efficacy of deep brain stimulation in treating depression [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(在线): 1-9. |
| [2] | Zhu Xiaolong, Zhang Wei, Yang Yang. Visualization analysis of research hotspots and cutting-edge information in the field of intervertebral disc regeneration and repair [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2391-2402. |
| [3] | Wen Fayan, Li Yan, Qiang Tianming, Yang Chen, Shen Linming, Li Yadong, Liu Yongming. Unilateral biportal endoscopic technology for treatment of lumbar degenerative diseases: global research status and changing trends [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2380-2390. |
| [4] | Xinjiang Branch of China Trauma Rescue & Treatment Association, Infectious Diseases Committee of Xinjiang Medical Association, Orthopedics Committee of Xinjiang Medical Association. Expert consensus on diagnosis and treatment of brucellar osteoarthritis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2403-2412. |
| [5] | Wang Nan, Chen Shuang, Xi Zhipeng, Qian Yuzhang, Zhang Xiaoyu, Gu Jun, Kang Ran, Xie Lin. MRI evaluation of nerve root subsidence sign affecting efficacy of percutaneous endoscopic decompression in lumbar spinal stenosis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2262-2268. |
| [6] | Li Zhifei, Han Bin, Liu Qiuli, Zhang Zhanming, Wei Haokai, Zuo Kuangshi, Zhang Yisheng. Cervical motion characteristics in patients with cervical spondylotic radiculopathy based on motion capture technology [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(9): 2286-2293. |
| [7] | Yang Xuetao, Zhu Menghan, Zhang Chenxi, Sun Yimin, Ye Ling. Applications and limitations of antioxidant nanomaterials in oral cavity [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2044-2053. |
| [8] | Chen Haojie, Wang Dai, Shen Shan. Immune inflammatory microenvironment mechanisms in peri-implantitis [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2054-2062. |
| [9] | Yang Qiongqiong, Liu Wei. Comparison of performance and clinical effects of zirconia and titanium implants [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2063-2071. |
| [10] | Liu Yang, Liu Donghui , Xu Lei, Zhan Xu, Sun Haobo, Kang Kai. Role and trend of stimuli-responsive injectable hydrogels in precise myocardial infarction therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2072-2080. |
| [11] | Wang Zheng, Cheng Ji, Yu Jinlong, Liu Wenhong, Wang Zhaohong, Zhou Luxing. Progress and future perspectives on the application of hydrogel materials in stroke therapy [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2081-2090. |
| [12] | Guo Yuchao, Ni Qianwei, Yin Chen, Jigeer·Saiyilihan, Gao Zhan . Quaternized chitosan hemostatic materials: synthesis, mechanism, and application [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2091-2100. |
| [13] | Liu Dawei, Cui Yingying, Wang Fanghui, Wang Zixuan, Chen Yuhan, Li Yourui, Zhang Ronghe. Epigallocatechin gallate-mediated bidirectional regulation of reactive oxygen species and its application in nanomaterials [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2101-2112. |
| [14] | Lai Yu, Chen Yueping, Zhang Xiaoyun. Research hotspots and frontier trends of bioactive materials in treating bone infections [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 2132-2144. |
| [15] | Sun Lei, Zhang Qi, Zhang Yu. Pro-osteoblastic effect of chlorogenic acid protein microsphere/polycaprolactone electrospinning membrane [J]. Chinese Journal of Tissue Engineering Research, 2026, 30(8): 1877-1884. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||