Chinese Journal of Tissue Engineering Research ›› 2025, Vol. 29 ›› Issue (18): 3925-3933.doi: 10.12307/2025.654
Previous Articles Next Articles
Efficacy of rehabilitation robots on lower limb motor function in patients with cerebral palsy: a Meta-analysis
Liu Xingzhao1, Hu Tong1, Ma Yan1, Wang Qian1, Wei Xiaohui1, Chang Wanpeng1, Yu Shaohong2, 3
- 1College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China; 2The Second Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250001, Shandong Province, China; 3College of Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China
-
Received:2024-06-05Accepted:2024-07-26Online:2025-06-28Published:2024-11-29 -
Contact:Yu Shaohong, Professor, The Second Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan 250001, Shandong Province, China; College of Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
About author:Liu Xingzhao, Master candidate, College of Rehabilitation Medicine, Shandong University of Traditional Chinese Medicine, Jinan 250355, Shandong Province, China -
Supported by:Humanities and Social Sciences Subjects in Shandong Province, No. 2023-JKZX-02 (to YSH)
CLC Number:
Cite this article
Liu Xingzhao, Hu Tong, Ma Yan, Wang Qian, Wei Xiaohui, Chang Wanpeng, Yu Shaohong. Efficacy of rehabilitation robots on lower limb motor function in patients with cerebral palsy: a Meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2025, 29(18): 3925-3933.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
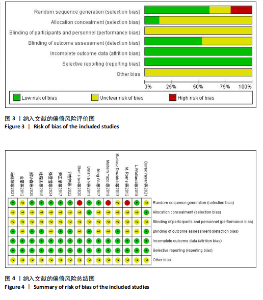
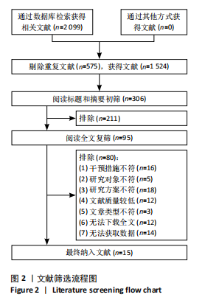
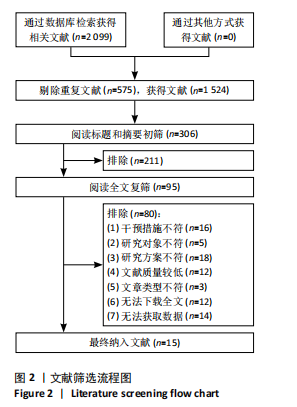
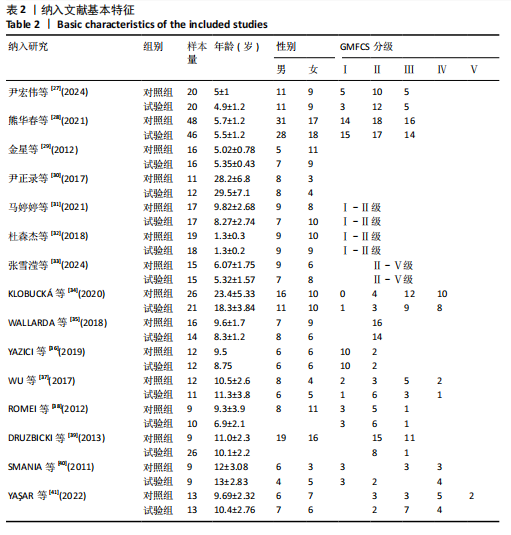
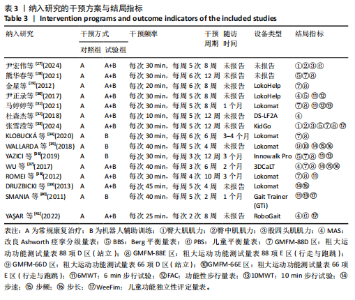
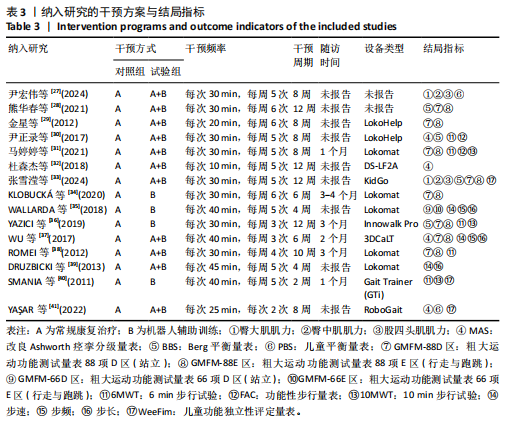
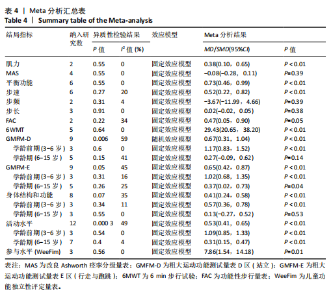
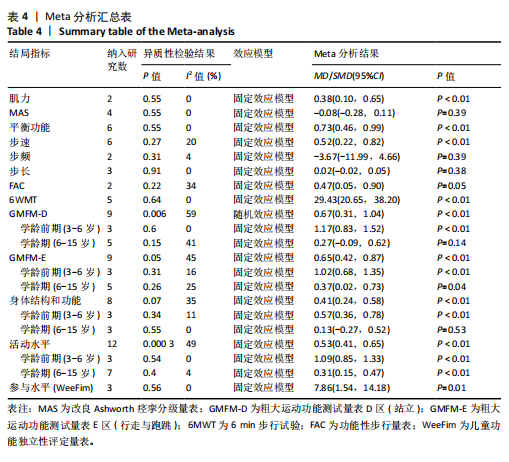
2.3 文献质量评价 所纳入15篇文献中9篇报告了具体随机方法[27-28,30-33,35,37,40],如随机数字表法和随机抽签法(低风险);3篇文献仅报告随机分配[29,39,41],未提供具体随机方法(中风险);3篇文献按照治疗类型、治疗方法和招募时间分配(高风险) [34,36,38]。2篇文献对研究使用分配隐藏(低风险) [40-41];7篇文献对结果测评使用了盲法(低风险) [28,30-32,39-41];15篇文献结果数据完整、无选择性报道、其他偏倚风险情况均不清楚[27-41]。具体评价见图3,4。 2.4 Meta分析结果 2.4.1 两组肌力差异 2篇文献共70例患者进行下肢肌肉力量评定[27,33],各研究间异质性不显著(I2=0%,P > 0.1),采用固定效应模型,两组肌力评分具有显著差异(SMD=0.38,95%CI:0.10-0.65,P < 0.05),见表4。 2.4.2 两组MAS评分差异 4篇文献共109例患者采用MAS评分进行肌张力评定[30,32,37,41]。各研究间异质性不显著(I2=0%,P > 0.1),采用固定效应模型,两组MAS评分差异无显著性意义(MD=-0.08,95%CI:-0.28-0.11,P > 0.05),见表4。 2.4.3 两组平衡功能差异 6篇文献共338例患者采用BBS或PBS进行平衡功能评定[27-28,30,33,36,41]。各研究间异质性不显著(I2=0%,P > 0.1),采用固定效应模型,两组平衡功能评分具有显著差异(SMD=0.73,95%CI:0.46-0.99,P < 0.05),见表4。 2.4.4 两组步速差异 6篇文献共160例患者采用10MWT或步态速度进行步速评定[31,35-37,39-40]。各研究间异质性不显著(I2=20%,P > 0.1),采用固定效应模型,两组步速评分具有显著差异(SMD=0.52,95%CI:0.22-0.82,P < 0.05),见表4。 2.4.5 两种步频差异 2篇文献共53例患者进行步频评定[35,37]。各研究间异质性不显著(I2=4%,P > 0.1),采用固定效应模型,两组步频差异无显著性意义(MD=-3.67,95%CI:-11.99-4.66,P > 0.05),见表4。 2.4.6 两组步长差异 3篇文献共88例患者进行步长评定[35,37,39]。各研究间异质性不显著(I2=0%,P > 0.1),采用固定效应模型,两组步长差异无显著性意义(MD=0.02,95%CI:-0.02-0.05,P > 0.05),见表4。 2.4.7 两组FAC评分差异 2篇文献共53例患者采用FAC评分进行步行功能评定[30-31]。各研究间异质性不显著(I2=34%,P > 0.1),采用固定效应模型,两组FAC评分具有显著差异(MD=0.47,95%CI:0.05-0.90,P=0.05),见表4。"

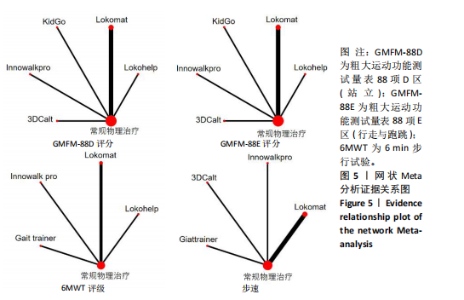
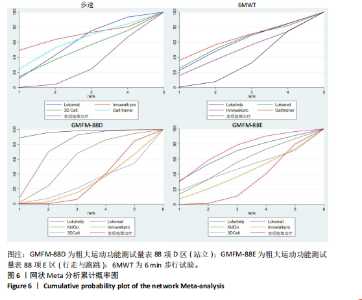
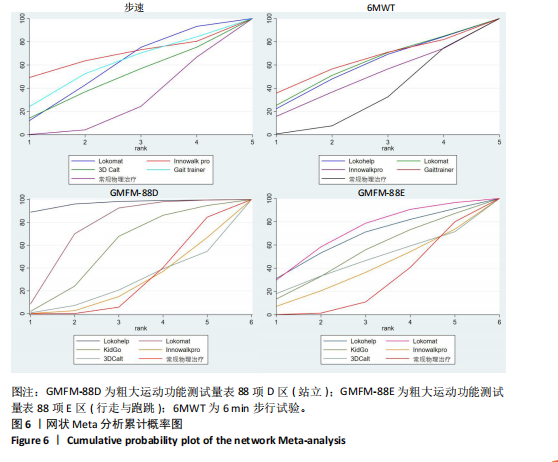
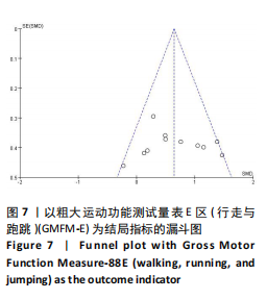
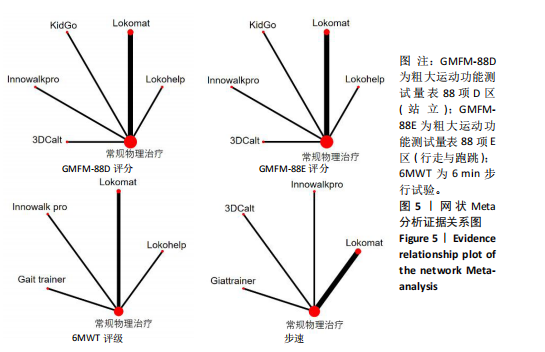
2.4.8 两组6MWT评级差异 5篇文献共114例患者采用6MWT评级进行步行距离评定[30-31,36,38,40]。各研究间异质性不显著(I2=0%,P > 0.1),采用固定效应模型,两组6MWT评级具有显著差异(MD=29.43,95%CI:20.65-38.20,P < 0.05),见表4。 2.4.9 两组粗大运动功能(站立) GMFM-D评分差异 9篇文献共329例患者采用GMFM-D评分进行粗大运动功能(站立)评定[28-29,31,33-38]。 各研究间异质性显著(I2=59%,P < 0.1),采用随机效应模型,两组GMFM-D评分具有显著差异(SMD=0.67,95%CI:0.31-1.04,P < 0.05)。根据年龄进行亚组分析,1篇文献不符合年龄要求[34],共8篇文献纳入亚组分析。学龄前期(3-6岁)组:异质性不显著(I2=0%,P > 0.1),两组GMFM-D评分高于对照组(SMD=1.17,95%CI:0.83-1.52,P < 0.05);学龄期(6-15岁)组:异质性不显著(I2=41%,P > 0.1),两组GMFM-D评分差异无显著性意义(SMD=0.27,95%CI:-0.09-0.62,P > 0.05),见表4。 2.4.10 两组粗大运动功能(行走与跑跳)GMFM-E评分差异 9篇文献共329例患者采用GMFM-E评分进行粗大运动功能(行走与跑跳)评定[28-29,31,33-38]。各研究间异质性不显著(I2=45%,P < 0.1),采用固定效应模型,两组GMFM-E评分差异有显著性意义(SMD=0.65,95%CI:0.42-0.87,P < 0.05)。根据年龄进行亚组分析,1篇文献不符合年龄要求[34],共8篇文献纳入亚组分析。学龄前期(3-6岁)组:异质性不显著(I2=16%,P > 0.1),试验组GMFM-E评分高于对照组(SMD=1.02,95%CI:0.68-1.35,P < 0.05);学龄期(6-15岁)组:异质性不显著(I2=25%,P > 0.1),试验组GMFM-E评分高于对照组(SMD=0.37,95%CI:0.02-0.73,P < 0.05),见表4。 2.4.11 两组身体结构与功能差异 8篇文献共297例患者进行身体结构与功能水平评定[27-28,30,32-33,36-37,41]。各研究间异质性不显著(I2=35%,P < 0.1),采用固定效应模型,两组身体结构与功能水平具有显著差异(SMD=0.41,95%CI:0.24-0.58,P < 0.05)。根据年龄进行亚组分析,2篇文献不符合年龄要求[30,32],共6篇文献纳入亚组分析。学龄前期(3-6岁)组:异质性不显著(I2=11%,P > 0.1),试验组身体结构与功能评分高于对照组(SMD=0.57,95%CI:0.36-0.78,P <0.05);学龄期(6-15岁)组:异质性不显著(I2=0%,P > 0.1),两组差异无显著性意义(SMD=0.13,95%CI:-0.27-0.52, P > 0.05),见表4。 2.4.12 两组活动水平差异 12篇文献共405例患者进行活动水平评定[28-31,33-40]。各研究间异质性不显著(I2=49%,P < 0.1),采用固定效应模型,两组活动水平具有显著差异(SMD=0.53,95%CI:0.41-0.65,P < 0.05)。根据年龄进行亚组分析,2篇文献不符合年龄要求[30,34],共10篇文献纳入亚组分析。学龄前期(3-6岁)组:异质性不显著(I2=0%,P > 0.1),试验组活动水平优于对照组(SMD=1.09,95%CI:0.85-1.33,P < 0.05);学龄期(6-15岁)组:异质性不显著(I2=4%,P > 0.1),试验组活动水平优于对照组(SMD=0.31,95%CI:0.15-0.47,P < 0.01),见表4。 2.4.13 两组参与水平差异(WeeFim) 3篇文献共74例患者采用WeeFim进行日常生活能力评定[33,40-41]。各研究间异质性不显著(I2=0%,P > 0.1),采用固定效应模型,两组WeeFim评分具有显著差异(MD=7.86,95%CI:1.54-14.18,P < 0.05),见表4。 2.5 网状Meta分析结果 2.5.1 采用与下肢运动功能密切相关的GMFM-88D、GMFM-88E、6MWT和步速来比较不同机器人的疗效 不同干预措施的网状关系见图5。不同圆点代表不同干预措施,圆点越大,表明此干预措施病例数越多。两圆点之间相连的实线代表二者之间存在直接比较的证据,实线越粗,表明直接比较证据越多。由网状关系图可知,不同干预措施之间不存在三角形闭环,因此无需进行不一致性检验。 2.5.2 概率排名 ①在改善步速方面,不同机器人最佳概率排序为:Innowalkpro (66.9%) > Gait trainer (58.0%) > Lokomat (55.6%) > 3DCalt (45.7%) > 常规康复治疗(23.9%)。②在改善6MWT评级方面,不同机器人最佳概率排序为:Gait trainer(60.8%) > Lokomat(58.1%) > Lokohelp(56.9%) > Innowalkro(45.9%) >常规康复治疗(28.3%)。③在改善GMFM-88D区评分方面,不同机器人最佳概率排序为:Lokohelp(96.3%) > Lokomat(73.3%) > KidGo(55.1%) > 常规康复治疗(26.5%) > Innowalkpro (24.5%) > 3DCalt(24.4%)。④在改善GMFM-88E区评分方面,不同机器人最佳概率排序为:Lokomat (71.2%) > Lokohelp(66.1%) > KidGo(52.6%) > 3DCalt(46.1%) > Innowalkpro(37.4%) > 常规康复治疗(26.7%)。网状Meta分析累计概率见图6。 2.6 不良反应 一项研究报道,少数患者在佩戴机器人装置后,因摩擦大腿内根部皮肤而产生轻微不适,休息后缓解,不影响第2天的治疗[30]。另一项研究报道机器人的耐受性良好,除小腿擦伤等小问题外,无不良事件发生[34]。在其他研究中未发现不良反应。"
| [1] BROMHAM N, DWORZYNSKI K, EUNSON P, et al. Cerebral palsy in adults: summary of NICE guidance. BMJ. 2019;364:l806. [2] COOPER MS, MACDONALD-LAURS E, ANTOLOVICH GC. Cerebral palsy: A neurodevelopmental disorder with motor disability. Dev Med Child Neurol. 2024. doi: 10.1111/dmcn.15960. [3] SEWELL MD, EASTWOOD DM, WIMALASUNDERA N. Managing common symptoms of cerebral palsy in children. BMJ. 2014;349:g5474. [4] SHEKARI Z, SADEGHIAN AFARANI R, FATOREHCHY S, et al. Relationship Between Postural Asymmetry, Balance, and Pain in Children With Spastic Cerebral Palsy. Pediatr Neurol. 2024;155:84-90. [5] BELIZÓN-BRAVO N, ROMERO-GALISTEO RP, CANO-BRAVO F, et al. Effects of Dynamic Suit Orthoses on the Spatio-Temporal Gait Parameters in Children with Cerebral Palsy: A Systematic Review. Children (Basel). 2021;8(11):1016. [6] NOVAK I, MORGAN C, ADDE L, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017;171(9):897-907. [7] BEKTESHI S, MONBALIU E, MCINTYRE S, et al. Towards functional improvement of motor disorders associated with cerebral palsy. Lancet Neurol. 2023;22(3):229-243. [8] KORZENIEWSKI SJ, SLAUGHTER J, LENSKI M, et al. The complex aetiology of cerebral palsy. Nat Rev Neurol. 2018;14(9):528-543. [9] SHIH STF, TONMUKAYAKUL U, IMMS C, et al. Economic evaluation and cost of interventions for cerebral palsy: a systematic review. Dev Med Child Neurol. 2018;60(6):543-558. [10] 李晓捷,邱洪斌,姜志梅,等.中国十二省市小儿脑性瘫痪流行病学特征[J].中华实用儿科临床杂志,2018,33(5):378-383. [11] STATES RA, SALEM Y, KRZAK JJ, et al. Three-Dimensional Instrumented Gait Analysis for Children With Cerebral Palsy: An Evidence-Based Clinical Practice Guideline. Pediatr Phys Ther. 2024;36(2):182-206. [12] DE MIGUEL-FERNÁNDEZ J, LOBO-PRAT J, PRINSEN E, et al. Control strategies used in lower limb exoskeletons for gait rehabilitation after brain injury: a systematic review and analysis of clinical effectiveness. J Neuroeng Rehabil. 2023;20(1):23. [13] VOLPINI M, AQUINO M, HOLANDA AC, et al. Clinical effects of assisted robotic gait training in walking distance, speed, and functionality are maintained over the long term in individuals with cerebral palsy: a systematic review and meta-analysis. Disabil Rehabil. 2022;44(19):5418-5428. [14] BONANNO M, MILITI A, LA FAUCI BELPONER F, et al. Rehabilitation of Gait and Balance in Cerebral Palsy: A Scoping Review on the Use of Robotics with Biomechanical Implications. J Clin Med. 2023;12(9):3278. [15] MANIKOWSKA F, BRAZEVIC S, KRZYŻAŃSKA A, et al. Effects of Robot-Assisted Therapy on Gait Parameters in Pediatric Patients With Spastic Cerebral Palsy. Front Neurol. 2021;12:724009. [16] ABIDIN N, ÜNLÜ AKYÜZ E, CANKURTARAN D, et al. The effect of robotic rehabilitation on posture and trunk control in non-ambulatory cerebral palsy. Assist Technol. 2022. doi: 10.1080/10400435.2022.2059592. [17] KIRTON A, METZLER MJ, CRAIG BT, et al. Perinatal stroke: mapping and modulating developmental plasticity. Nat Rev Neurol. 2021;17(7):415-432. [18] PERPETUINI D, RUSSO EF, CARDONE D, et al. Identification of Functional Cortical Plasticity in Children with Cerebral Palsy Associated to Robotic-Assisted Gait Training: An fNIRS Study. J Clin Med. 2022;11(22):6790. [19] SUCUOGLU H. Effects of robot-assisted gait training alongside conventional therapy on the development of walking in children with cerebral palsy. J Pediatr Rehabil Med. 2020;13(2):127-135. [20] PERI E, TURCONI AC, BIFFI E, et al. Effects of dose and duration of Robot-Assisted Gait Training on walking ability of children affected by cerebral palsy. Technol Health Care. 2017;25(4):671-681. [21] VEZÉR M, GRESITS O, ENGH MA, et al. Evidence for gait improvement with robotic-assisted gait training of children with cerebral palsy remains uncertain. Gait Posture. 2024;107:8-16. [22] 黄信萍,吴娟妹,吴莹莹,等.下肢康复机器人步态训练对脑性瘫痪儿童下肢功能疗效的Meta分析[J].中国儿童保健杂志,2023,31(11):1241-1247. [23] LIM JH, KANG EY, PARK SJ, et al. Effects of robot rehabilitation on the motor function and gait in children with cerebral palsy: a systematic review and meta-analysis. J Exerc Rehabil. 2024;20(3):92-99. [24] AURICH-SCHULER T, WARKEN B, GRASER JV, et al. Practical Recommendations for Robot-Assisted Treadmill Therapy (Lokomat) in Children with Cerebral Palsy: Indications, Goal Setting, and Clinical Implementation within the WHO-ICF Framework. Neuropediatrics. 2015;46(4):248-260. [25] 姜静远,邱卓英,王国祥,等.世界卫生组织国际健康分类家族在康复中系统应用的方案与路线图[J].中国康复理论与实践,2020,26(11):1241-1255. [26] 中国康复医学会儿童康复专业委员会,中国残疾人康复协会小儿脑性瘫痪康复专业委员会,中国医师协会康复医师分会儿童康复专业委员会.中国脑性瘫痪康复指南(2022)第一章:概论[J].中华实用儿科临床杂志,2022,37(12):887-892. [27] 尹宏伟,余永林,杨安琪,等.下肢外骨骼机器人步行训练对痉挛型双瘫脑性瘫痪患儿平衡功能的影响[J].中国康复医学杂志,2024,39(3):340-346. [28] 熊华春,陈精慧,王军,等.下肢康复机器人训练对痉挛型脑瘫患儿粗大运动功能及平衡功能的影响[J].郑州大学学报(医学版),2021,56(3):370-375. [29] 金星,孟兆祥,尹正录,等.康复机器人辅助步行训练对脑瘫患儿步行能力的影响[J].中国康复医学杂志,2012,27(9):822-824. [30] 尹正录,孟兆祥,薛永骥,等.康复机器人辅助步行训练对成年脑性瘫痪患者步行能力的影响[J].中国康复医学杂志, 2017,32(1):97-99. [31] 马婷婷,张皓.机器人辅助步态训练对痉挛型脑性瘫痪患儿运动和步行功能的效果[J].中国康复理论与实践,2021, 27(11):1260-1265. [32] 杜森杰,张跃,李红英,等.儿童爬行促通训练机器人在痉挛型双瘫患儿康复中应用的效果[J].中国康复理论与实践, 2018,24(10):1195-1200. [33] 张雪滢,何娜,黄艳.KidGo外骨骼康复机器人训练对痉挛型脑性瘫痪患儿下肢运动功能的影响[J].中华物理医学与康复杂志,2024,46(2):129-133. [34] KLOBUCKÁ S, KLOBUCKÝ R, KOLLÁR B. Effect of robot-assisted gait training on motor functions in adolescent and young adult patients with bilateral spastic cerebral palsy: A randomized controlled trial. NeuroRehabilitation. 2020;47(4):495-508. [35] WALLARD L, DIETRICH G, KERLIRZIN Y, et al. Effect of robotic-assisted gait rehabilitation on dynamic equilibrium control in the gait of children with cerebral palsy. Gait Posture. 2018;60:55-60. [36] YAZICI M, LIVANELIOĞLU A, GÜCÜYENER K, et al. Effects of robotic rehabilitation on walking and balance in pediatric patients with hemiparetic cerebral palsy. Gait Posture. 2019;70:397-402. [37] WU M, KIM J, ARORA P, et al. Effects of the Integration of Dynamic Weight Shifting Training Into Treadmill Training on Walking Function of Children with Cerebral Palsy: A Randomized Controlled Study. Am J Phys Med Rehabil. 2017;96(11):765-772. [38] ROMEI M, MONTINARO A, PICCININI L, et al. Efficacy of robotic-assisted gait training compared with intensive task-oriented physiotherapy for children with Cerebral Palsy.Physical Therapy. 2012;72(15): 1890-1894. [39] DRUŻBICKI M, RUSEK W, SNELA S, et al. Functional effects of robotic-assisted locomotor treadmill thearapy in children with cerebral palsy. J Rehabil Med. 2013; 45(4):358-363. [40] SMANIA N, BONETTI P, GANDOLFI M, et al. Improved gait after repetitive locomotor training in children with cerebral palsy. Am J Phys Med Rehabil. 2011;90(2):137-149. [41] YAŞAR B, ATICI E, AZIM REZAEI D, et al. Effectiveness of Robot-Assisted Gait Training on Functional Skills in Children with Cerebral Palsy. J Pediatr Neurol. 2022;20(3):164-170. [42] BAX MC, FLODMARK O, TYDEMAN C. Definition and classification of cerebral palsy. From syndrome toward disease. Dev Med Child Neurol Suppl. 2007;109:39-41. [43] GHAI S, HAKIM M, DANNENBAUM E, et al. Prevalence of Vestibular Dysfunction in Children With Neurological Disabilities: A Systematic Review. Front Neurol. 2019; 10:1294. [44] MORGAN P, MURPHY A, OPHEIM A, et al. Gait characteristics, balance performance and falls in ambulant adults with cerebral palsy: An observational study. Gait Posture. 2016;48:243-248. [45] KANASHVILI B, MILLER F, CHURCH C, et al. The change in sagittal plane gait patterns from childhood to maturity in bilateral cerebral palsy. Gait Posture. 2021;90:154-160. [46] 朱志浩,石斌,王晶.脑瘫步态康复机器人研究进展[J].机器人,2023,45(5):626-640. [47] 陶璟,霍宇飞,于随然.面向儿童的下肢康复外骨骼机器人研发进展[J].中国康复医学杂志,2021,36(11):1445-1449. [48] LOBATO GARCIA L, GONZÁLEZ GONZÁLEZ Y, et al. Beneficios de la robótica en la rehabilitación de la marcha en la parálisis cerebral: una revisión sistemática [Benefits of robotics in gait rehabilitation in cerebral palsy: A systematic review]. Rehabilitacion (Madr). 2020;54(2):128-136. [49] CHIU HC, ADA L, BANIA TA. Mechanically assisted walking training for walking, participation, and quality of life in children with cerebral palsy. Cochrane Database Syst Rev. 2020;11(11):CD013114. [50] LAPORTA-HOYOS O, FIORI S, PANNEK K, et al. Longitudinal assessment of brain lesions in children with cerebral palsy and association with motor functioning. Eur J Paediatr Neurol. 2024;49:27-34. [51] HILDERLEY AJ, WRIGHT FV, TAYLOR MJ, et al. Functional Neuroplasticity and Motor Skill Change Following Gross Motor Interventions for Children With Diplegic Cerebral Palsy. Neurorehabil Neural Repair. 2023;37(1):16-26. [52] JULIEN L, MOREAU-PERNET G, ROCHETTE E, et al. Robot-assisted gait training improves walking and cerebral connectivity in children with unilateral cerebral palsy. Pediatr Res. 2024. doi: 10.1038/s41390-024-03240-1. [53] BERGER A, HORST F, STEINBERG F, et al. Increased gait variability during robot-assisted walking is accompanied by increased sensorimotor brain activity in healthy people. J Neuroeng Rehabil. 2019;16(1):161. [54] CRAIG BT, HILDERLEY A, KINNEY-LANG E, et al. Developmental neuroplasticity of the white matter connectome in children with perinatal stroke. Neurology. 2020;95(18):e2476-e2486. [55] DAN B. Intensive repetitive motor training: how does it work in children with cerebral palsy? Dev Med Child Neurol. 2021;63(9):1008. [56] REID LB, PAGNOZZI AM, FIORI S, et al. Measuring neuroplasticity associated with cerebral palsy rehabilitation: An MRI based power analysis. Int J Dev Neurosci. 2017;58:17-25. [57] HANNA SE, ROSENBAUM PL, BARTLETT DJ, et al. Stability and decline in gross motor function among children and youth with cerebral palsy aged 2 to 21 years. Dev Med Child Neurol. 2009;51(4):295-302. [58] CLOODT E, LINDGREN A, RODBY-BOUSQUET E. Knee and ankle range of motion and spasticity from childhood into adulthood: a longitudinal cohort study of 3,223 individuals with cerebral palsy. Acta Orthop. 2024;95:200-205. [59] KLOBUCKÁ S, KLOBUCKÝ R, KOLLÁR B. The effect of patient-specific factors on responsiveness to robot-assisted gait training in patients with bilateral spastic cerebral palsy. NeuroRehabilitation. 2021; 49(3):375-389. [60] DE BENEDICTIS A, ROSSI-ESPAGNET MC, DE PALMA L, et al. Structural networking of the developing brain: from maturation to neurosurgical implications. Front Neuroanat. 2023;17:1242757. [61] KIM M, PARK C, JEON H, et al. Comparative effects of community-based family-child-centered care and conventional pediatric rehabilitation for cerebral palsy. NeuroRehabilitation. 2021;49(4):533-546. [62] DIOT CM, YOUNGBLOOD JL, FRIESEN AH, et al. Robot-Assisted Gait Training with Trexo Home: Users, Usage and Initial Impacts. Children (Basel). 2023;10(3):437. |
| [1] | Zhang Xinxin, Gao Ke, Xie Shidong, Tuo Haowen, Jing Feiyue, Liu Weiguo. Network meta-analysis of non-surgical treatments for foot and ankle ability and dynamic balance in patients with chronic ankle instability [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1931-1944. |
| [2] | Fu Enhong, Yang Hang, Liang Cheng, Zhang Xiaogang, Zhang Yali, Jin Zhongmin. OpenSim-based prediction of lower-limb biomechanical behavior in adolescents with plantarflexor weakness [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(9): 1789-1795. |
| [3] | Wang Juan, Wang Guanglan, Zuo Huiwu. Efficacy of exercise therapy in the treatment of anterior cruciate ligament reconstruction patients: #br# a network meta-analysis #br# [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(8): 1714-1726. |
| [4] | Wen Zixing, Xu Xin, Zhu Shengqun. Correlations between gastrocnemius morphology parameters and physical activity capacity in elderly females under high-frequency ultrasound [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(5): 1058-1063. |
| [5] | Li Zhe, Li Ping, Zhang Chao, Guo Guangling. A network meta-analysis of efficacy of mesenchymal stem cells from different sources in treatment of premature ovarian failure animal models [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(36): 7898-7908. |
| [6] | Tian Jinxin, Zhao Yuxin, Hu Tong, Cui Tiantian, Ma Lihong. Effects of different transcranial magnetic stimulation modes on refractory depression in adults: a network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(35): 7639-7648. |
| [7] | Wang Kaigang, Hao Dongsheng, Ma Pei, Zhou Shuo, Li Ruimin. Comparison of efficacy of different biological scaffolds for pulp regeneration therapy in immature permanent teeth: a Bayesian network meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(34): 7447-7460. |
| [8] | Liu Mengling, Li Yongjie, Liu Hongju. Effect of increased stride length on knee kinematics and dynamics of asymmetric gait after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7109-7115. |
| [9] | Yuan Yingjia, Yi Yanzi, Li Jin, Wang Ke, Wang Yu, Lin Tianye, Zhang Qingwen, He Wei, Wei Qiushi. Effect of hip abductor muscle exercise on three-dimensional gait and collapse rate in patients with non-traumatic femoral head necrosis [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(33): 7211-7216. |
| [10] | Zhang Jian, Cai Feng, Li Tingwen, Ren Pengbo. Fatigue gait recognition of athletes based on fish swarm algorithm [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6489-6498. |
| [11] | Wang He, Yu Shaohong, . Meta-analysis of transcranial direct current stimulation in improving lower limb motor dysfunction in stroke patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(30): 6556-6565. |
| [12] | Gou Yanyun, Hou Meijin, Jiang Zheng, Chen Shaoqing, Chen Xiang, Gao Yuzhan, Wang Xiangbin. Biomechanical characteristics of walking in patients with idiopathic scoliosis: cross-sectional analysis of three-dimensional motion capture [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 471-477. |
| [13] | Li Jia, Liu Qianru, Xing Mengnan, Chen Bo, Jiao Wei, Meng Zhaoxiang. A network meta-analysis on therapeutic effect of different types of exercise on knee osteoarthritis patients [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 609-616. |
| [14] | Zheng Xiang, Zhang Mingxing, Huang Ya, Shan Sharui. Improvement of lower limb walking function in patients with chronic non-specific low back pain by biofeedback assisted electrical stimulation [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(3): 547-553. |
| [15] | Chen Jiayong, Tang Meiling, Lu Jianqi, Pang Yan, Yang Shangbing, Mao Meiling, Luo Wenkuan, Lu Wei. Causal association between metabolites and sarcopenia: a big data analysis of genome-wide association studies in the European population [J]. Chinese Journal of Tissue Engineering Research, 2025, 29(29): 6369-6380. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||