Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (17): 2647-2652.doi: 10.12307/2024.471
Previous Articles Next Articles
Application of different grafts in anterior cruciate ligament revision
Liu Guoli, Li Liang, Xie Kunnan, Yin Xianghui, Zhang Yanrui, Yi Fan, Dai Shifeng
- Department of Joint and Sports Medicine, The Second Hospital of Tangshan, Tangshan 063000, Hebei Province, China
-
Received:2023-06-05Accepted:2023-07-22Online:2024-06-18Published:2023-12-14 -
About author:Liu Guoli, Master, Attending physician, Department of Joint and Sports Medicine, The Second Hospital of Tangshan, Tangshan 063000, Hebei Province, China -
Supported by:Hebei Provincial Health Scientific Research Fund Project, No. 20221731 (to LGL)
CLC Number:
Cite this article
Liu Guoli, Li Liang, Xie Kunnan, Yin Xianghui, Zhang Yanrui, Yi Fan, Dai Shifeng. Application of different grafts in anterior cruciate ligament revision[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(17): 2647-2652.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
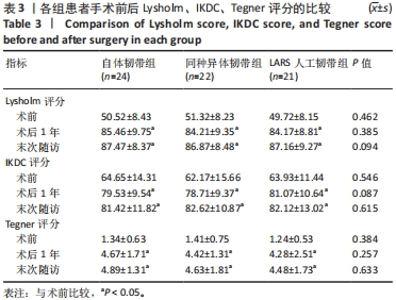
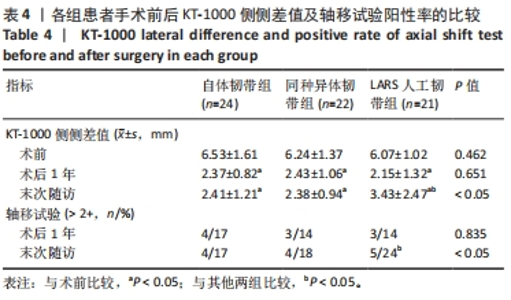
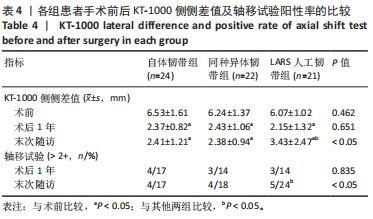
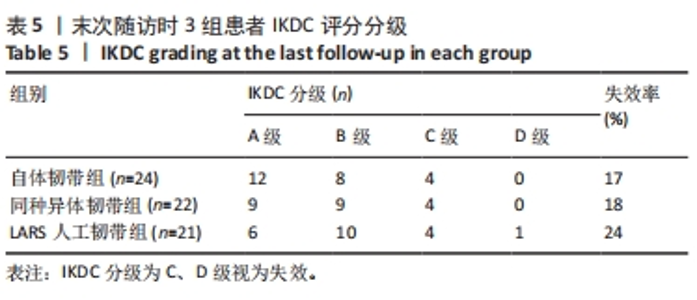
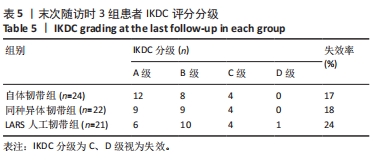
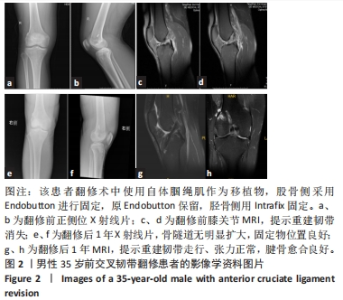
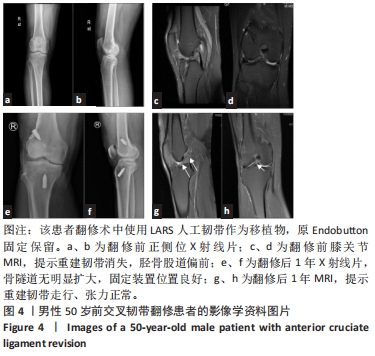
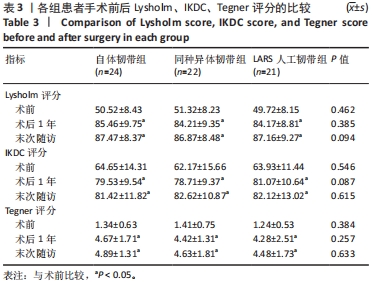
2.4 并发症与材料生物相容性 所有患者伤口均一期愈合,未发现感染病例。67例患者中,有3例(自体韧带组2例,同种异体韧带组1例)患者术后两三天内出现膝关节腔内血肿,该3例患者股骨侧固定均为横穿钉固定,给予抽出淤血处置,后期完全吸收。所有患者按照康复计划功能锻炼,术后无关节僵直、关节腔内感染等并发症出现,部分患者术后出现膝前疼痛症状,指导患者加强股四头肌肌力训练,逐渐恢复正常活动后膝前疼痛逐渐缓解。3组患者均未发生与植入物相关的不良反应。 2.5 各组患者主观指标评估结果 3组患者术后1年与末次随访的国际膝关节文献委员会(IKDC)评分、Lysholm膝关节评分、Tegner运动评分均高于术前(P < 0.05),3组组内术后1年与末次随访的IKDC评分、Lysholm膝关节评分、Tegner运动评分比较差异均无显著性意义(P > 0.05),3组间术后1年及末次随访的IKDC评分、Lysholm膝关节评分、Tegner运动评分比较差异均无显著性意义(P > 0.05),见表3。"
| [1] WRIGHT RW, HUSTON LJ, HAAS AK, et al. Association Between Graft Choice and 6-Year Outcomes of Revision Anterior Cruciate Ligament Reconstruction in the MARS Cohort. Am J Sports Med. 2021;49(10):2589-2598. [2] RAHARDJA R, ZHU M, LOVE H, et al. No difference in revision rates between anteromedial portal and transtibialdrilling of the femoral graft tunnel in primary anterior cruciate ligament reconstruction: early results from the New Zealand ACL Registry. Knee. Surg Sports Traumatol Arthrosc. 2020;28:3631-3638. [3] DING DY, ZHANG AL, ALLEN CR, et al. Subsequent Surgery After Revision Anterior Cruciate Ligament Reconstruction: Rates and Risk Factors From a Multicenter Cohort. Am J Sports Med. 2017;45(9):2068-2076. [4] KANAKAMEDALA AC, EDGAR CM, FANELLI GC, et al. Surgical Considerations in Revision Anterior Cruciate Ligament Reconstruction. Instr Course Lect. 2022;71: 475-487. [5] MIAO S, LI S, WU Z, et al. The Clinical Efficacy and Risk Factors after Revision and Reconstruction of Anterior Cruciate Ligament. J Healthc Eng. 2021;2021:6606492. [6] 蒋艳芳,王健,王永健,等.前交叉韧带翻修重建术后中长期临床疗效及影响因素[J].北京大学学报(医学版),2021,53(5):857-864. [7] TULLOCH SJ, DEVITT BM, PORTER T, et al. Primary ACL reconstruction using the LARS device is associated with a high failure rate at minimum of 6-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3626-3632. [8] JANSSEN RP, SCHEFFLER SU. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2102-2108. [9] 李韬,朱彦霖,林唐棣,等.同种异体肌腱重建膝关节前交叉韧带的研究进展与临床应用[J].中国组织工程研究,2019,23(10):1605-1610. [10] MARS Group. Meniscal and Articular Cartilage Predictors of Clinical Outcome After Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(7):1671-1679. [11] GROSSMAN MG, ELATTRACHE NS, SHIELDS CL, et al. Revision anterior cruciate ligament reconstruction: three- to nine-year follow-up. Arthroscopy. 2005;21(4): 418-423. [12] AHN JH, LEE YS, HA HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med. 2008;36(10):1889-1895. [13] 运行,魏钰,李众利,等.前交叉韧带翻修术中期疗效研究[J].中国修复重建外科杂志,2021,35(1):58-63. [14] 马勇,敖英芳,崔国庆,等.前交叉韧带重建后翻修的临床研究[J].中华外科杂志,2008,46(9):650-653. [15] CRISTIANI R, ENGSTROM B, EDMAN G, et al. Revision anterior cruciate ligament reconstruction restores knee laxity but shows inferior functional knee outcome compared with primary reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):137-145. [16] WRIGHT RW, JOHNSON L, BROPHY RH, et al. Revision Anterior Cruciate Ligament Reconstruction Outcomes at a Minimum of 5-Year Follow-Up: A Systematic Review. J Knee Surg. 2019;32(3):218-221. [17] WRIGHT RW, HUSTON LJ, HAAS AK, et al. Predictors of Patient-Reported Outcomes at 2 Years After Revision Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2019;47(10):2394-2401. [18] LIEN-IVERSEN T, MORGAN DB, JENSEN C, et al. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? A systematic review and meta-analysis. Br J Sports Med. 2020;54(10):592-598. [19] GRASSI A, ZAFFAGNINI S, MARCHEGGIANI MG, et al. After revision anterior cruciate ligament reconstruction, who returns to sport? A systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1295-1304. [20] KUECHLE DK, PEARSON SE, BEACH WR, et al. Allograft anterior cruciate ligament reconstruction in patients over 40 years of age. Arthroscopy. 2002;18(8):845-853. [21] YU SB, YANG RH, ZUO ZN, et al. Histological characteristics and ultrastructure of polyethylene terephthalate LARS ligament after the reconstruction of anterior cruciate ligament in rabbits. Int J Clin Exp Med. 2014;7(9):2511-2518. [22] JIA Z, XUE C, WANG W, et al. Clinical outcomes of anterior cruciate ligament reconstruction using LARS artificial graft with an at least 7-year follow-up. Medicine (Baltimore). 2017;96(14):e6568. [23] YU A, PRENTICE HA, BURFEIND WE, et al. Risk of Infection After Allograft Anterior Cruciate Ligament Reconstruction: Are Nonprocessed Allografts More Likely to Get Infected? A Cohort Study of Over 10,000 Allografts. Am J Sports Med. 2018;46(4):846-851. [24] GUO L, YANG L, DUAN XJ, et al. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft: comparison of autograft, fresh-frozen allograft, and gamma-irradiated allograft. Arthroscopy. 2012;28(2):211-217. [25] CRISTIANI R, ENGSTROM B, EDMAN G, et al. Revision anterior cruciate ligament reconstruction restores knee laxity but shows inferior functional knee outcome compared with primary reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):137-145. [26] O’NEILL DB. Revision arthroscopically assisted anterior cruciate ligament reconstruction with previously unharvested ipsilateral autografts. Am J Sports Med. 2004;32(8):1833-1841. [27] YUMASHEV AV, BALTINA TV, BABASKIN DV. Outcomes after arthroscopic revision surgery for anterior cruciate ligament injuries. Acta Orthop. 2021;92(4):443-447. [28] MARTIN RK, WASTVEDT S, PAREEK A, et al. Predicting anterior cruciate ligament reconstruction revision: a machine learning analysis utilizing the Norwegian Knee Ligament Register. J Bone Joint Surg Am. 2022;104:145-153. [29] WOLFSON TS, MANNINO B, OWENS BD, et al. Tunnel Management in Revision Anterior Cruciate Ligament Reconstruction: Current Concepts. Am J Sports Med. 2023;51(2):545-556. [30] AHN JH, SON DW, AHN JH, et al. Remnant Preservation of the Primary Vertical Graft in Revision Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med. 2023;11(3):951749052. [31] BELK JW, LITTLEFIELD CP, SMITH JH, et al. Autograft Demonstrates Superior Outcomes for Revision Anterior Cruciate Ligament Reconstruction When Compared With Allograft: A Systematic Review. Am J Sports Med. 2023:3635465231152232. doi: 10.1177/03635465231152232. [32] HEFFNER M, CHANG RN, ROYSE KE, et al. Association Between Graft Type and Risk of Repeat Revision Anterior Cruciate Ligament Reconstruction: A Cohort Study of 1747 Patients. Am J Sports Med. 2023;51(6):1434-1440. [33] HELITO CP, SOBRADO MF, MOREIRA DSA, et al. The Addition of Either an Anterolateral Ligament Reconstruction or an Iliotibial Band Tenodesis Is Associated With a Lower Failure Rate After Revision Anterior Cruciate Ligament Reconstruction: A Retrospective Comparative Trial. Arthroscopy. 2023;39(2):308-319. [34] PAUDEL YR, SOMMERFELDT M, VOAKLANDER D. Incidence and risk factors for revision and contralateral anterior cruciate ligament reconstruction: A population-based retrospective cohort study. Medicine (Baltimore). 2023;102(20):e33669. [35] LEON J, FLANIGAN DC, COLATRUGLIO M, et al. Larger Prior Tibial Tunnel Size Is Associated with Increased Failure Risk following Revision Anterior Cruciate Ligament Reconstruction. J Knee Surg. 2023;36(8):820-826. [36] PENG Y, XU JC, FU DJ, et al. [Efficacy comparison between a new generation of artificial ligaments and bone-patellar tendon-bone autograft for anterior cruciate ligament revision]. Zhonghua Yi Xue Za Zhi. 2023;103(11):822-828. [37] SASAKI E, KIMURA Y, SASAKI S, et al. Influence of hamstring tendon and bone-patellar tendon-bone autografts on worsened patient reported outcome measurements in revision anterior cruciate ligament reconstruction: Comparing outcomes between primary and revision reconstructions. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2022;29:1-8. [38] GLASBRENNER J, FISCHER M, RASCHKE MJ, et al. Primary stability of single-stage revision reconstruction of the anterior cruciate ligament in case of failure of dynamic intraligamentary stabilization depends on implant position during ACL repair. Arch Orthop Trauma Surg. 2022;142(7):1589-1595. [39] ROSSO F, ROSSI R, FALETTI R, et al. Transepicondylar distance measured on MRI can predict the length of the graft required for different anterior cruciate ligament reconstruction (ACLR) techniques useful for revision surgery. J Orthop Traumatol. 2022;23(1):50. [40] HAFFAR A, ALI R, MEHTA N, et al. Prior Anterior Cruciate Ligament Reconstruction Does Not Compromise the Functional Outcomes of Medial Unicompartmental Knee Arthroplasty Although Revision for Progressive Arthritis May Occur Earlier. J Arthroplasty. 2022;37(2):238-242. |
| [1] | Chen Kaijia, Liu Jingyun, Cao Ning, Sun Jianbo, Zhou Yan, Mei Jianguo, Ren Qiang. Application and prospect of tissue engineering in treatment of osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1450-1456. |
| [2] | Bai Chen, Yang Wenqian, Meng Zhichao, Wang Yuze. Strategies for repairing injured anterior cruciate ligament and promoting graft healing [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1457-1463. |
| [3] | Wang Juan, Wang Ling, Zuo Huiwu, Zheng Cheng, Wang Guanglan, Chen Peng. Rehabilitative efficacy of kinesio taping following anterior cruciate ligament reconstruction: a Meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(4): 651-656. |
| [4] | Long Jundong, Shi Yehong, Wang Cheng, Chen Shijiu. Effects of different freezing techniques on the rejection of allogeneic vascular transplantation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(3): 433-438. |
| [5] | Tu Meijuan, Zhang Chunli, Deng Li, Fang Bing, Sun Guangyu, Zhu Xiaoyu, Zhang Xinqiong. Characteristics of acute graft-versus-host disease of the intestine after unrelated cord blood transplantation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(25): 3955-3959. |
| [6] | Zhang Lianpeng, Julaiti•Maitirouzi, Zhang Zhihao, Zhang Rui, Abulikemu·Maimaiti, Paerhati·Rexiti. Mechanical analysis of cortical bone trajectory screw placement in lumbar revision [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(24): 3783-3788. |
| [7] | Huang Jie, Shi Yanghua, Tan Zhen, Bo Zhandong. Free vascularized fibular grafting in treatment of femoral head osteonecrosis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3373-3379. |
| [8] | Zheng Xuejing, Mei Wei, Zhu Yanyu, Bao Xiaoxiao, Zhang Zhenhui, Wang Qingde. Stage III Kümmell’s disease treated with injured-vertebra screw placement combined with transpedicular impaction bone grafting: quick restoration of spinal stability [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2865-2870. |
| [9] | Li Luyi, Li Xiaojie, Hei Zeming, Liu Hua. Effect of graft type on knee function after anterior cruciate ligament reconstruction [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(17): 2753-2758. |
| [10] | Wang Ling, Jiang Xia, Chen Peng, Zheng Cheng, Xu Jinrong. Biomechanical characteristics of the lower limbs of athletes after anterior cruciate ligament reconstruction during bilateral vertical jumping [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2215-2220. |
| [11] | Xiong Bohan, Lu Xiaojun, Xue Wenqiang, Liu Jinrui, Gao Xianling, Yu Hong, Li Yajuan, Liu Haolong, Li Yanlin. Protective effect of anterior cruciate ligament reconstruction assisted by internal tension-reduction technique on the articular cartilage of southern Yunnan small-ear pigs [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(14): 2221-2226. |
| [12] | Gao Siyu, Yao Lihong, Bian Zhilei, Zhang Suping, Li Li, Fan Jinpeng, Qin Jing, Peng Yingnan, Wan Dingming. Analysis of risk factors for short-term death after allogeneic hematopoietic stem cell transplantation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 2009-2016. |
| [13] | Zhang Wenhui, Pei Xiaohang, Kong Dai, Liu Zhongwen. Efficacy of umbilical cord mesenchymal stem cells replacing donor bone marrow cells in haploidentical hematopoietic stem cell transplantation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(13): 2042-2046. |
| [14] | Zuo Huiwu, Geng Zhizhong, Chen Peng, Lin Xikai, Chen Jian. Knee function recovery in patients with anterior cruciate ligament reconstruction after blood flow restriction training: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(12): 1962-1968. |
| [15] | Li Hui, Zhang Kun, Hao Yangquan, Feng Lei, Yang Zhi, Xu Peng, Lu Chao. Robot-assisted core decompression and bone grafting for ARCO II osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(4): 547-551. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||