Chinese Journal of Tissue Engineering Research ›› 2024, Vol. 28 ›› Issue (21): 3373-3379.doi: 10.12307/2024.080
Previous Articles Next Articles
Free vascularized fibular grafting in treatment of femoral head osteonecrosis
Huang Jie1, 2, Shi Yanghua2, 3, Tan Zhen1, Bo Zhandong2
- 1Department of Joint and Sports Medicine Surgery, Second Affiliated Hospital of Guangxi Medical University, Nanning 530007, Guangxi Zhuang Autonomous Region, China; 2Department of Bone and Joint Surgery, First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, China; 3Department of Joint and Sports Medicine Surgery, Tenth Affiliated Hospital of Guangxi Medical University, Qinzhou 535099, Guangxi Zhuang Autonomous Region, China
-
Received:2023-04-20Accepted:2023-06-10Online:2024-07-28Published:2023-09-27 -
Contact:Bo Zhandong, MD, Chief physician, Department of Bone and Joint Surgery, First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, China -
About author:Huang Jie, Master, Attending physician, Department of Joint and Sports Medicine Surgery, Second Affiliated Hospital of Guangxi Medical University, Nanning 530007, Guangxi Zhuang Autonomous Region, China; Department of Bone and Joint Surgery, First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, China Shi Yanghua, Master, Attending physician, Department of Bone and Joint Surgery, First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi Zhuang Autonomous Region, China; Department of Joint and Sports Medicine Surgery, Tenth Affiliated Hospital of Guangxi Medical University, Qinzhou 535099, Guangxi Zhuang Autonomous Region, China -
Supported by:National Natural Science Foundation of China, No. 82160836 (to TZ); Scientific Research Project of Guangxi Zhuang Autonomous Region Health Commission, No. Z-A20220604 (to HJ)
CLC Number:
Cite this article
Huang Jie, Shi Yanghua, Tan Zhen, Bo Zhandong. Free vascularized fibular grafting in treatment of femoral head osteonecrosis[J]. Chinese Journal of Tissue Engineering Research, 2024, 28(21): 3373-3379.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks

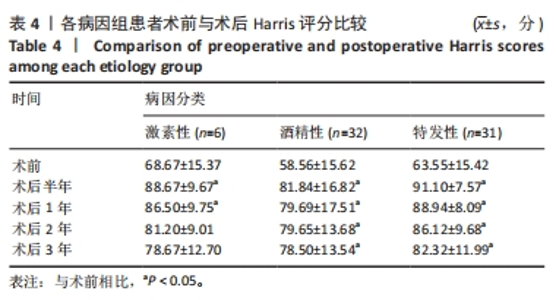
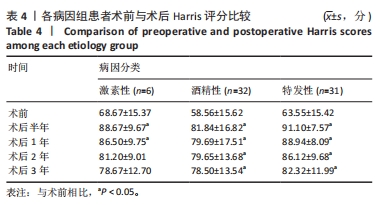
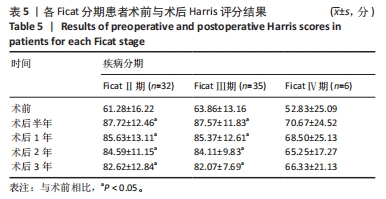
2.6 不良事件 有2例患者术后出现大腿前外侧皮肤浅表感觉减退,术后1年随访时感觉已恢复正常,考虑术中挫伤股前外侧皮神经所致。患者术后均未出现骨折、感染、深静脉血栓等并发症。 2.7 植入物与宿主的生物相容性 经随访,纳入患者均未出现植入物周围感染、过敏反应、免疫反应及排斥反应。 2.8 典型病例 男性患者,49岁,因“双侧髋部疼痛1年余”入院,无基础疾病,否认创伤史及糖皮质激素药物使用史,偶有饮酒;VAS评分左髋4分,右髋4分;Harris评分左髋71分,右髋69分;双髋X射线片检查提示双侧股骨头缺血坏死,左侧Ficat Ⅲ期,右侧Ficat Ⅲ期(图3A)。入院6 d后行双侧吻合血管游离腓骨移植术,术后3 d双髋X射线片检查显示双侧股骨头坏死病灶完整刮除,植骨充分,置入腓骨段位置良好(图3B)。术后3年,VAS评分左髋1分,右髋1分;Harris评分左髋92分,右髋91分;双髋X射线片检查显示双侧股骨头软骨下骨的重塑和愈合良好,关节间隙正常,未见继发性骨折(图3C);患者双髋“4”字位摆放良好(图3D-E),下蹲功能良好(图3F)。"

| [1] SERONG S, HAVERSATH M, JÄGER M, et al. Prevalence of CAM deformity and its influence on therapy success in patients with osteonecrosis of the femoral head. J Tissue Eng Regen Med. 2019; 13(4):546-554. [2] IKEUCHI K, HASEGAWA Y, SEKI T, et al. Epidemiology of nontraumatic osteonecrosis of the femoral head in Japan. Mod Rheumatol. 2015; 25(2):278-281. [3] SATO R, ANDO W, FUKUSHIMA W, et al. Epidemiological study of osteonecrosis of the femoral head using the national registry of designated intractable diseases in Japan. Mod Rheumatol. 2022;32(4): 808-814. [4] ZHAO DW, YU M, HU K, et al. Prevalence of Nontraumatic Osteonecrosis of the Femoral Head and its Associated Risk Factors in the Chinese Population: Results from a Nationally Representative Survey. Chin Med J (Engl). 2015;128(21):2843-2850. [5] MONT MA, CHERIAN JJ, SIERRA RJ, et al. Nontraumatic Osteonecrosis of the Femoral Head: Where Do We Stand Today? A Ten-Year Update. J Bone Joint Surg Am. 2015;97(19):1604-1627. [6] ARBAB D, KÖNIG DP. Atraumatic Femoral Head Necrosis in Adults. Dtsch Arztebl Int. 2016;113(3):31-38. [7] VERONESE N, STUBBS B, SOLMI M, et al. Association between lower limb osteoarthritis and incidence of depressive symptoms: data from the osteoarthritis initiative. Age Ageing. 2017;46(3):470-476. [8] ASSOULINE-DAYAN Y, CHANG C, GREENSPAN A, et al. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32(2): 94-124. [9] OHZONO K, SAITO M, TAKAOKA K, et al. Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1991; 73(1):68-72. [10] KALENDERER Ö, ERKUŞ S, TURGUT A, et al. Preoperative planning of femoral head reduction osteotomy using 3D printing model: A report of two cases. Acta Orthop Traumatol Turc. 2019;53(3):226-229. [11] 顾长源,杜斌,孙光权,等.股骨头坏死保髋治疗常用术式的利与弊[J]. 中国组织工程研究,2020,24(21):3379-3386. [12] 曾祥洪,梁博伟.股骨头坏死保髋治疗的新策略[J]. 中国组织工程研究,2021,25(3):431-437. [13] TAYLOR GI, MILLER GD, HAM FJ. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55(5):533-544. [14] WEILAND AJ, DANIEL RK, RILEY LH JR. Application of the free vascularized bone graft in the treatment of malignant or aggressive bone tumors. Johns Hopkins Med J. 1977;140(3):85-96. [15] JUDET H, JUDET J, GILBERT A. Vascular microsurgery in orthopaedics. Int Orthop. 1981;5(2):61-68. [16] FONTECHA CG, ROCA I, BARBER I, et al. Femoral head bone viability after free vascularized fibular grafting for osteonecrosis: SPECT/CT study. Microsurgery. 2016;36(7):573-577. [17] 中华医学会骨科分会显微修复学组,中国修复重建外科专业委员会骨缺损及骨坏死学组. 成人股骨头坏死诊疗标准专家共识(2012年版)[J]. 中华骨科杂志,2012,32(6):606-610. [18] YOON BH, JONES LC, CHEN CH, et al. Etiologic Classification Criteria of ARCO on Femoral Head Osteonecrosis Part 1: Glucocorticoid-Associated Osteonecrosis. J Arthroplasty. 2019; 34(1):163-168. [19] YOON BH, JONES LC, CHEN CH, et al. Etiologic Classification Criteria of ARCO on Femoral Head Osteonecrosis Part 2: Alcohol-Associated Osteonecrosis. J Arthroplasty. 2019;34(1):169-174. [20] FICAT RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67(1):3-9. [21] MALIZOS KN, KARANTANAS AH, VARITIMIDIS SE, et al. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol. 2007;63(1):16-28. [22] 郝双林. 临床疼痛的测定方法及其评价[J]. 国外医学(麻醉学与复苏分册),1993,14(4):228-230. [23] HARRIS WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737-755. [24] SMITH MV, KLEIN SE, CLOHISY JC, et al. Lower extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(5):468-477. [25] Microsurgery Department of the Orthopedics Branch of the Chinese Medical Doctor Association; Group from the Osteonecrosis and Bone Defect Branch of the Chinese Association of Reparative and Reconstructive Surgery; Microsurgery and Reconstructive Surgery Group of the Orthopedics Branch of the Chinese Medical Association. Chinese Guideline for the Diagnosis and Treatment of Osteonecrosis of the Femoral Head in Adults. Orthop Surg. 2017;9(1):3-12. [26] ZHAO DW. To strengthen the understanding of the pathophysiology in osteonecrosis of femoral head. Chin J Joint Surg. 2014;8(5):560-562. [27] SCHILDHAUER TA, ROBIE B, MUHR G, et al. Bacterial adherence to tantalum versus commonly used orthopedic metallic implant materials. J Orthop Trauma. 2006;20(7):476-484. [28] LIU Y, YAN L, ZHOU S, et al. Tantalum rod implantation for femoral head osteonecrosis: survivorship analysis and determination of prognostic factors for total hip arthroplasty. Int Orthop. 2016;40(7):1397-1407. [29] 李子荣. 骨坏死[M]. 北京: 人民卫生出版社,2012:183-188. [30] CHEN Y, MIAO Y, LIU K, et al. Evolutionary course of the femoral head osteonecrosis: Histopathological - radiologic characteristics and clinical staging systems. J Orthop Translat. 2021;32:28-40. [31] 刘予豪,周驰,陈雷雷,等. 基于股骨头坏死围塌陷期理论的保髋术式总结[J]. 中国修复重建外科杂志,2017,31(8):1010-1015. [32] FICAT RP, ARLET J. Ischemia and necrosis of bone. Williams & Wilkins, 1980:53-74. [33] KOREN L, GINESIN E, MELAMED Y, et al. Hyperbaric oxygen for stage I and II femoral head osteonecrosis. Orthopedics. 2015;38(3):e200-e205. [34] AL OMRAN A. Multiple drilling compared with standard core decompression for avascular necrosis of the femoral head in sickle cell disease patients. Arch Orthop Trauma Surg. 2013;133(5):609-613. [35] PIERCE TP, JAUREGUI JJ, ELMALLAH RK, et al. A current review of core decompression in the treatment of osteonecrosis of the femoral head. Curr Rev Musculoskelet Med. 2015;8(3):228-232. [36] MOON JK, YOON JY, KIM CH, et al. Multiple drilling and multiple matchstick-like bone allografts for large osteonecrotic lesions in the femoral head: an average 3-year follow-up study. Arch Orthop Trauma Surg. 2020;140(11):1655-1663. [37] HAO YQ, GUO H, ZHU T, et al. Core decompression, lesion clearance and bone graft in combination with Tongluo Shenggu decoction for the treatment of osteonecrosis of the femoral head: A retrospective cohort study. Medicine (Baltimore). 2018;97(41):e12674. [38] HUA KC, YANG XG, FENG JT, et al. The efficacy and safety of core decompression for the treatment of femoral head necrosis: a systematic review and meta-analysis. J Orthop Surg Res. 2019; 14(1):306. [39] OKURA T, HASEGAWA Y, MORITA D, et al. What factors predict the failure of curved intertrochanteric varus osteotomy for the osteonecrosis of the femoral head? Arch Orthop Trauma Surg. 2016; 136(12):1647-1655. [40] KAWANO K, MOTOMURA G, IKEMURA S, et al. Long-term hip survival and factors influencing patient-reported outcomes after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head: A minimum 10-year follow-up case series. Mod Rheumatol. 2020;30(1):184-190. [41] MORITA D, HASEGAWA Y, OKURA T, et al. Long-term outcomes of transtrochanteric rotational osteotomy for non-traumatic osteonecrosis of the femoral head. Bone Joint J. 2017;99-B(2):175-183. [42] KARASUYAMA K, MOTOMURA G, IKEMURA S, et al. Risk factor analysis for postoperative complications requiring revision surgery after transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. J Orthop Surg Res. 2018;13(1):6. [43] 吴克亮,冯文俊,李杰,等.游离髂骨瓣联合带血管蒂大转子骨瓣移植对中青年ARCOⅢ期股骨头坏死患者的保髋作用[J].中国组织工程研究,2019,23(31):4921-4926. [44] YOO MC, KIM KI, HAHN CS, et al. Long-term followup of vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res. 2008;466(5):1133-1140. [45] BOSS JH, MISSELEVICH I. Osteonecrosis of the femoral head of laboratory animals: the lessons learned from a comparative study of osteonecrosis in man and experimental animals. Vet Pathol. 2003; 40(4):345-354. [46] SULTAN AA, KHLOPAS A, SURACE P, et al. The use of non-vascularized bone grafts to treat osteonecrosis of the femoral head: indications, techniques, and outcomes. Int Orthop. 2019;43(6):1315-1320. [47] YAO C, YI N, SHEN J, et al. Clinical reports of surgical dislocation of the hip with sequestrum clearance and impacting bone graft for grade IIIA-IIIB aseptic necrosis of femoral head (ANFH) patients. Oncotarget. 2017;8(30):50084-50090. [48] ZHOU G, ZHANG Y, ZENG L, et al. Should thorough Debridement be used in Fibular Allograft with impaction bone grafting to treat Femoral Head Necrosis: a biomechanical evaluation. BMC Musculoskelet Disord. 2015;16:140. [49] WU CT, YEN SH, LIN PC, et al. Long-term outcomes of Phemister bone grafting for patients with non-traumatic osteonecrosis of the femoral head. Int Orthop. 2019;43(3):579-587. [50] GOKHAN M, ULUSAL AE, ATIK A, et al. Descending branch of the lateral circumflex femoral artery as a recipient vessel for vascularized fibular grafts: Clinical case series. Microsurgery. 2014;34(8):633-637. [51] GONZÁLEZ DELLA VALLE A, BATES J, DI CARLO E, et al. Failure of free vascularized fibular graft for osteonecrosis of the femoral head: a histopathologic study of 6 cases. J Arthroplasty. 2005;20(3):331-336. [52] TETIK C, BAŞAR H, BEZER M, et al. Comparison of early results of vascularized and non-vascularized fibular grafting in the treatment of osteonecrosis of the femoral head. Acta Orthop Traumatol Turc. 2011;45(5):326-334. [53] CAO L, GUO C, CHEN J, et al. Free Vascularized Fibular Grafting Improves Vascularity Compared With Core Decompression in Femoral Head Osteonecrosis: A Randomized Clinical Trial. Clin Orthop Relat Res. 2017;475(9):2230-2240. [54] PLAKSEYCHUK AY, KIM SY, PARK BC, et al. Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85(4):589-596. [55] ZHANG CQ, GAO YS, ZHU ZH, et al. Why we choose free vascularized fibular grafting for osteonecrosis of the femoral head? Microsurgery. 2011;31(5):417-418. [56] LIGH CA, NELSON JA, FISCHER JP, et al. The Effectiveness of Free Vascularized Fibular Flaps in Osteonecrosis of the Femoral Head and Neck: A Systematic Review. J Reconstr Microsurg. 2017;33(3):163-172. [57] YOO MC, CHUNG DW, HAHN CS. Free vascularized fibula grafting for the treatment of osteonecrosis of the femoral head. Clin Orthop Relat Res. 1992;(277):128-138. [58] KAWATE K, YAJIMA H, SUGIMOTO K, et al. Indications for free vascularized fibular grafting for the treatment of osteonecrosis of the femoral head. BMC Musculoskelet Disord. 2007;8:78. [59] BEREND KR, GUNNESON EE, URBANIAK JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85(6):987-993. [60] EWARD WC, RINEER CA, URBANIAK JR, et al. The vascularized fibular graft in precollapse osteonecrosis: is long-term hip preservation possible? Clin Orthop Relat Res. 2012;470(10):2819-2826. [61] RICHARD MJ, DIPRINZIO EV, LORENZANA DJ, et al. Outcomes of free vascularized fibular graft for post-traumatic osteonecrosis of the femoral head. Injury. 2021;52(12):3653-3659. |
| [1] | Chen Kaijia, Liu Jingyun, Cao Ning, Sun Jianbo, Zhou Yan, Mei Jianguo, Ren Qiang. Application and prospect of tissue engineering in treatment of osteonecrosis of the femoral head [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(9): 1450-1456. |
| [2] | Zhang Xiaoyun, Liu Hua, Chai Yuan, Chen Feng, Zeng Hao, Gao Zhengang, Huang Yourong. Effect of Yishen Gushu Formula on bone metabolic markers and clinical efficacyn in patients with osteoporosis of kidney deficiency and blood stasis type [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(8): 1155-1160. |
| [3] | Cheng Jinhui, Wu Quan, Peng Min, Huang Changli, Tian Huimin, Li Yang. Preparation and properties of selective laser melting of porous titanium at a low energy density [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 664-668. |
| [4] | Wang Jianchun, Yang Shuqing, Su Xin, Wang Hongyuan. Different contents of B2O3 affect mechanical properties and bioactivity of bioactive glass scaffolds [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 712-716. |
| [5] | Lan Weiwei, Yu Yaodong, Huang Di, Chen Weiyi. In vitro degradation behavior of Mg-Zn-Ca alloys [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 717-723. |
| [6] | Wei Yuxue, Wang Di, Liu Xiaoqiu. Design, synthesis and properties of oral composite resin monomers with different photoinitiators [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 731-735. |
| [7] | Zhang Yihai, Shang Peng, Ma Benyuan, Hou Guanghui, Cui Lunxu, Song Wanzhen, Qi Dexuan, Liu Yancheng. Structural design and mechanical property analysis of trabecular scaffold of triply periodic minimal surface with a radial gradient [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(5): 741-746. |
| [8] | Yuan Xinwei, Huang Yixuan, Xi Hongzhong, Guo Mingbin, Mai Jianbin, Sun Guangquan, Liu Xin, Du Bin. Effect of three-dimensional spatial distribution of necrotic and support areas on outcomes of fibular support for hip preservation [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(18): 2789-2794. |
| [9] | Wan Jian, Wang Ning, Bei Chaoyong, Chen Yuanming, Wang Honggang. Two lumbar fusion regimens in treatment of single-level lumbar degenerative diseases based on propensity score matching [J]. Chinese Journal of Tissue Engineering Research, 2024, 28(12): 1914-1919. |
| [10] | Zheng Bo, Zhang Xiuli, Zhou Hao, He Zebi, Zhou Jin, Zhou Weiyun, Li Peng. Arthroscopy-assisted locking hollow screw fixation and open reduction plate internal fixation in the treatment of Schatzker II-III tibial plateau fractures: early CT evaluation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1410-1416. |
| [11] | He Yinhao, Li Xiaosheng, Chen Hongwen, Chen Tiezhu. 3D printed porous tantalum metal in the treatment of developmental dysplasia of the hip: current status and application prospect [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(9): 1455-1461. |
| [12] | Dong Zhou, Tao Hui, Liu Yiming, Wang Shansong, Li Chun, Hu Yong. Relationship between spine-pelvic sagittal plane balance and effects of percutaneous balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(29): 4635-4640. |
| [13] | Deng Moyuan, Peng Kun. Role and regulation of macrophages in biomaterial-mediated fibrosis formation [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(25): 4085-4092. |
| [14] | Lyu Jiayi, Yao Qingqiang, Zhu Yishen. Role and advantages of carbon nanotubes for tissue engineering [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(25): 4093-4100. |
| [15] | Chen Jianquan, Chen Maoshui, Lyu Zhouming, Chen Rongbin, Yu Zhaoyu, Liu Wanpeng, Lin Xinyuan, Lin Dingkun. Biomechanical properties of cortical bone trajectory combined with pedicle screw fixation on vertebral body motion unit: a finite element analysis [J]. Chinese Journal of Tissue Engineering Research, 2023, 27(22): 3457-3462. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||