[1] DANIAUX H. Transpedicular repositioning and spongioplasty in fractures of the vertebral bodies of the lower thoracic and lumbar spine. Unfallchirurg. 1986;89(5):197-213.
[2] DICK JC, JONES MP, ZDEBLICK TA, et al. A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord. 1994;7(5):402-407.
[3] 刘永强,周纪平. Kümmell病的临床研究进展[J].中国矫形外科杂志, 2023,31(3):242-246.
[4] 孙育良,熊小明,万趸,等. 短节段与长节段骨水泥强化固定联合椎体成形术治疗Ⅲ期Kümmell病疗效比较[J].中国修复重建外科杂志, 2020,34(10):1275-1280.
[5] 李江笔,那士博,公伟权,等.Kümmell病的临床治疗进展[J].中国骨伤, 2020,33(1):81-86.
[6] 唐本强,陈学明,崔利宾,等. Kümmell病经皮椎体成形术骨水泥渗漏的危险因素分析[J].中华骨科杂志,2020,40(23):1592-1600.
[7] LI K, WONG T, KUNG F, et al. Staging of Kümmell’s disease. J Musculoskelet Res. 2004;8(1):43-55.
[8] ZANG JQ, ZENG ZY, LU HG, et al. A comparative study of PSPVP and PSIBG in the treatment of stage II-III Kummell’s disease. Biomed Mater Eng. 2022. doi: 10.3233/BME-221456.
[9] 许正伟,郝定均,贺宝荣.《症状性陈旧性胸腰椎骨质疏松性骨折手术治疗临床指南》要点解读[J].中华创伤杂志,2022,38(4):297-300.
[10] 张天宇,陈小锋,许庭珉,等. Kümmell病诊治的研究进展[J]. 中华创伤杂志,2020,36(11):1046-1050.
[11] 竺军高,万双林,宁磊,等.长节段椎弓根螺钉复位内固定联合椎体后凸成形术治疗Ⅲ期可复型Kummell病的临床效果[J].中华外科杂志, 2022,60(3):230-236.
[12] 陈浩,杨俊松,郝定均.后路短节段固定骨水泥增强治疗Ⅲ期 Kümmell 病伴椎管狭窄[J] .中国修复重建外科杂志,2019,33(6):707-711.
[13] 赵士杰,李长明,许建柱,等.后路楔形截骨与椎体成形术联合长节段椎弓根螺钉内固定治疗骨质疏松性椎体骨折不愈合伴后凸畸形的疗效比较[J].中华创伤杂志,2022,38(9):806-813.
[14] 丁超利,张振辉,朱彦谕,等.经椎弓根打压植入含富集骨髓的同种异体骨联合后路内固定治疗Ⅲ期Kümmell病[J].中华创伤杂志,2022, 38(2):116-124.
[15] PACI M, BURKS S, WANG MY. Consensus Guidelines for the Treatment of Osteoporosis. Neurosurgery. 2018;82(1):N6-N7.
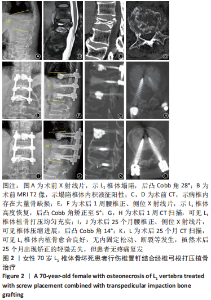
[16] Zhu YY, Zhang ZH, Jiang WT, et al. Therapeutic Efficacy of Transpedicular Impaction Bone Grafting with Long Segmental Posterior Instrumentation in Stage III Kümmell Disease. Spine. 2021;46(13):907-914.
[17] YUDOYONO F.Three-level thoracolumbar vertebroplasty with screw-rod-wire construct in Kummels disease patient with neurological deficit after low impact injury. Neurologico Spinale Medico Chirurgico. 2020;3(3):118-121.
[18] SHENG X, REN S. Surgical techniques for osteoporotic vertebral collapse with delayed neurological deficits:A systematic review. Int J Surg, 2016; 33 Pt A:42-48.
[19] 赵吉鹏,孙传,向学强,等.骨水泥强化椎弓根螺钉联合椎体成形术治疗Ⅲ型Kummell病[J].中国骨伤,2021,34(2):170-174.
[20] IZZO R, GUARNIERI G, GUGLIELMI G, et al. Biomechanics of the spine. Part I: spinal stability. Eur J Radiol. 2013;82(1):118-126.
[21] 张芸,王磊,高观,等.Kummell病不同时期骨组织形态与骨代谢标志物变化[J].中华骨质疏松和骨矿盐疾病杂志,2021,14(5):486-494.
[22] 尹知训,丁红梅,靳安民,等.胸腰椎骨质疏松压缩性骨折经椎弓根植骨的生物力学研究[J].中国临床解剖学杂志,2008,26(2):196-198.
[23] Dai SQ, Qin RQ, Shi X, et al. Percutaneous vertebroplasty versus kyphoplasty for the treatment of neurologically intact osteoporotic Kümmell’s disease. BMC Surg. 2021;21(1):65.
[24] Deng H, Li Y, Zhou J, et al. Therapeutic efficacy of Transpedicular Intracorporeal cement augmentation with short segmental posterior instrumentation in treating osteonecrosis of the vertebral body:a retrospective case series with a miniumum 5-years follow-up. BMC Musculoskelet Disord. 2019;20(1):305.
[25] LI Z, LIU T, YIN P, et al. The therapeutic effects of percutaneous kyphoplasty on osteoporotic vertebral compression fractures with or without intravertebral cleft. Int Orthop. 2019;43(2):359-365.
[26] 姚汝斌,王仕永,杨开舜.椎弓根内骨水泥灌注联合椎体后凸成形治疗Kummell病:增强椎体内骨水泥团块稳定性[J].中国组织工程研究, 2021,25(28):4435-4440.
[27] 肖伟,殷剑,赵清斌,等.经椎弓根植骨治疗胸腰段严重椎体塌陷伴神经功能障碍Kummell病患者临床疗效[J].创伤与急危重病医学,2021, 9(1):50-52.
[28] 张振辉,王庆德,王仲伟,等.后路长、短节段椎弓根螺钉固定联合经椎弓根打压植骨治疗Ⅲ期Kümmell病的疗效比较[J].中华创伤杂志, 2021,37(1):22-29.
[29] JAYANKURA M, SCHULZ AP, DELAHAUT O, et al. Percutaneous administration of allogeneic bone-forming cells for the treatment of delayed unions of fractures: a pilot study. Stem Cell Res Ther. 2021;12(1):363.
[30] 曾庆娟,刘传梅,程艳艳,等.经皮经伤椎与跨伤椎椎弓根置钉术对中青年胸腰椎爆裂性骨折椎体高度恢复的影像学研究[J].中国医学影像学杂志,2022,30(8):834-838+844.
[31] 张树威,李景峰,徐振华.短节段骨水泥螺钉内固定联合椎体成形术治疗Ⅲ期Kümmell病的疗效研究[J].骨科,2021,12(5):409-413.
[32] 朱亮,沈强,丁浩,等.跨伤椎和经伤椎置钉固定治疗胸腰椎爆裂骨折的疗效比较[J].临床骨科杂志,2022,25(3):328-333.
[33] 刘伟,曹爽,倪志豪,等.后路椎弓根螺钉长节段固定、短节段经伤椎固定及短节段跨伤椎固定对A型胸腰椎骨折的疗效比较[J].实用医学杂志,2022,38(19):2440-2445.
|