Chinese Journal of Tissue Engineering Research ›› 2020, Vol. 24 ›› Issue (3): 477-484.doi: 10.3969/j.issn.2095-4344.2422
Previous Articles Next Articles
A meta-analysis of expandable intramedullary nail versus interlocking intramedullary nail for treatment of femoral shaft fracture
Wang Wei1, Xie Chengxin1, Zhou Haonan1, Zhang Yu1, Wang Chenglong1, Yin Dong2
- 1Graduate School, Guangxi University of Chinese Medicine, Nanning 530000, Guangxi Zhuang Autonomous Region, China; 2People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530000, Guangxi Zhuang Autonomous Region, China
-
Received:2019-05-28Revised:2019-06-04Accepted:2019-09-18Online:2020-01-28Published:2019-12-27 -
Contact:Yin Dong, MD, Professor, Chief physician, People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning 530000, Guangxi Zhuang Autonomous Region, China -
About author:Wang Wei, Master candidate, Graduate School, Guangxi University of Chinese Medicine, Nanning 530000, Guangxi Zhuang Autonomous Region, China
CLC Number:
Cite this article
Wang Wei, Xie Chengxin, Zhou Haonan, Zhang Yu, Wang Chenglong, Yin Dong. A meta-analysis of expandable intramedullary nail versus interlocking intramedullary nail for treatment of femoral shaft fracture[J]. Chinese Journal of Tissue Engineering Research, 2020, 24(3): 477-484.
share this article
Add to citation manager EndNote|Reference Manager|ProCite|BibTeX|RefWorks
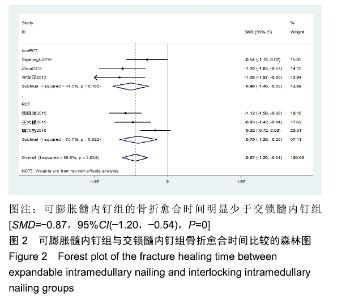
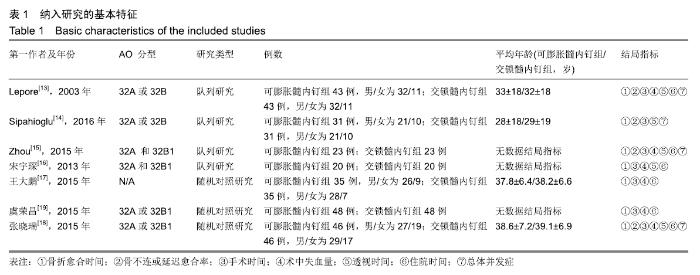
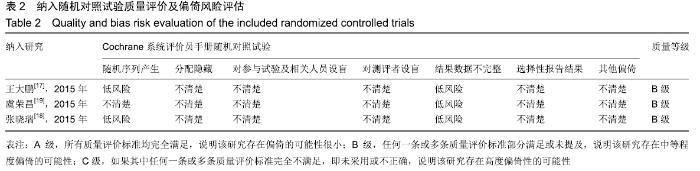
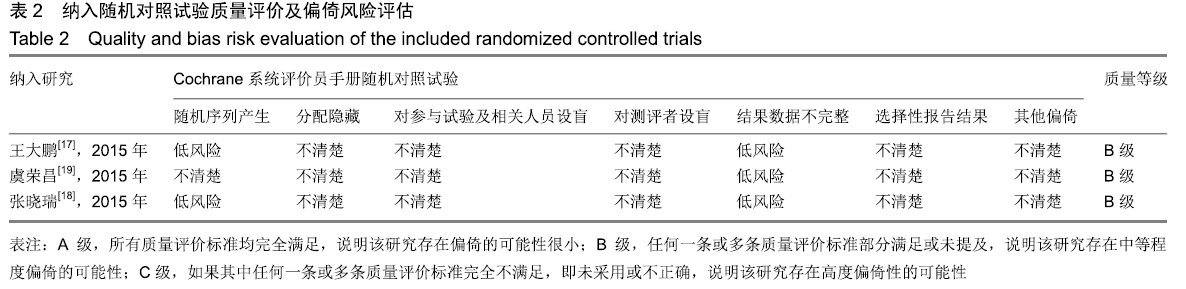
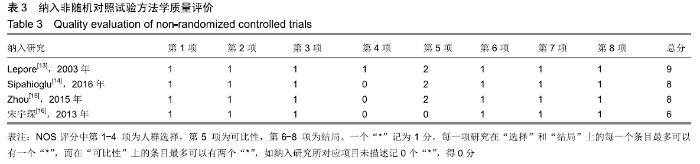
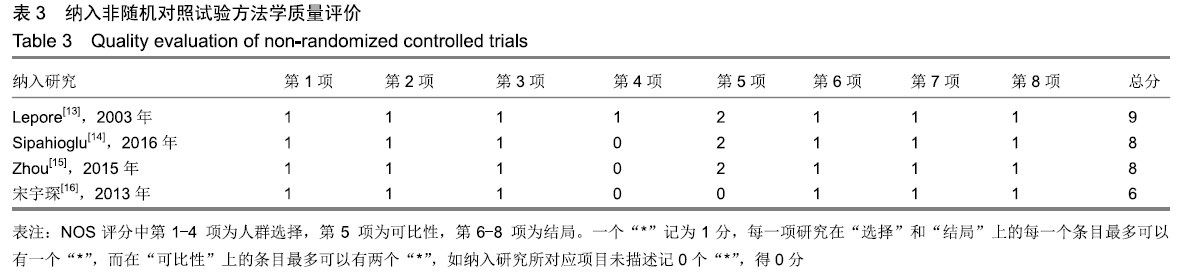
2.2 Meta分析结果 2.2.1 骨折愈合时间 共6篇文献报道了骨折愈合时 间[14-19],共计样本量481例,其中可膨胀髓内钉组239例,交锁髓内钉组242例。其中1篇文献只报道了24例(共计31例)可膨胀髓内钉组和27例(共计31例)交锁髓内钉组的骨折愈合时间[14]。异质性检验提示各研究间存在中度异质性(I2=58.5%,P=0.034),故采用随机效应模型。结果显示可膨胀髓内钉组术后骨折愈合时间明显少于交锁髓内钉组[SMD=-0.87,95%CI(-1.20,-0.54),P=0],见图2。按研究类型亚组分析,3篇非随机对照试验合并显示可膨胀髓内钉组的骨折愈合时间明显少于交锁髓内钉组[SMD=-0.98,95%CI(-1.46,-0.50),P=0][14-16]。3篇随机对照试验合并显示可膨胀髓内钉组的骨折愈合时间明显少于交锁髓内钉组[SMD=-0.78,95%CI(-1.28,-0.28),P=0.002][17-19]。 "
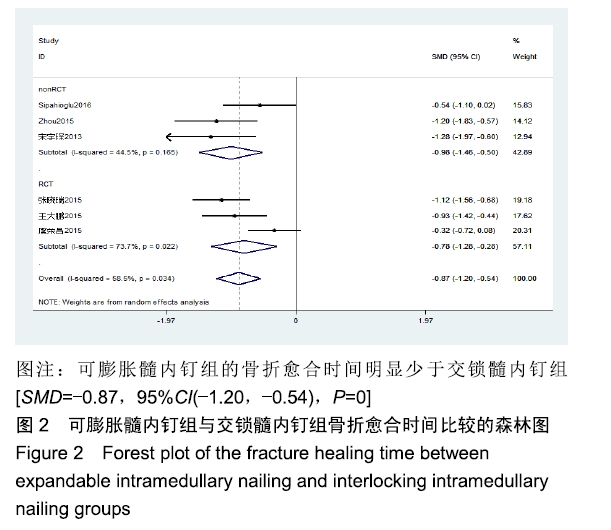
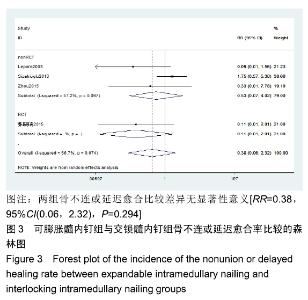
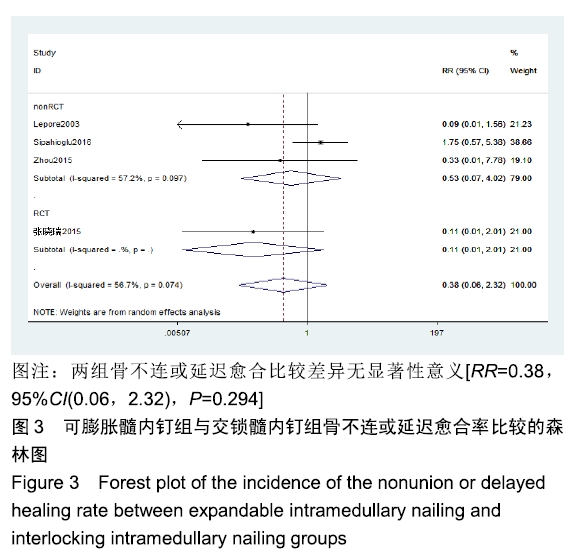
2.2.2 骨不连或延迟愈合 共有4篇文献报道了骨不连或延迟愈合[13-15,18],共计样本量286例,两组样本量各143例,骨不连或延迟愈合在可膨胀髓内钉组和交锁髓内钉组分别为7例(4.8%)和14例(9.7%)。异质性检验提示各研究间存在中度异质性(I2=57.8%,P=0.074),故采用随机效应模型。结果显示两组骨不连或延迟愈合比较差异无显著性意义[RR=0.38,95%CI(0.06,2.32),P=0.294],见图3。按研究类型亚组分析,3篇非随机对照试验合并显示两组骨不连或延迟愈合比较差异无显著性意义[RR=0.53,95%CI(0.07,4.02),P=0.536][13-15];1篇随机对照试验显示两组骨不连或延迟愈合比较差异无显著性意义[RR=0.11,95%CI(0.01,2.01),P=0.137][18]。"
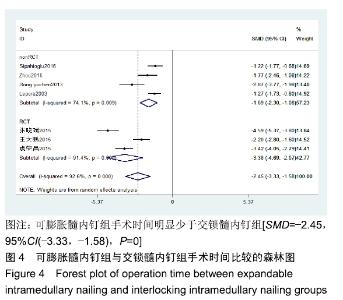
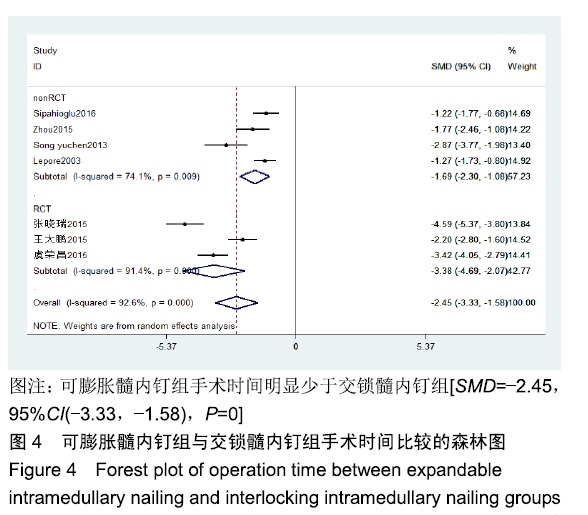
2.2.3 手术时间 共有7篇文献报道了手术时间[13-19],共计样本量492例,两组各246例。异质性检验提示各研究间存在明显异质性(I2=92.6%,P=0),故采用随机效应模型。结果显示可膨胀髓内钉组手术时间明显少于交锁髓内钉组[SMD=-2.45,95%CI(-3.33,-1.58),P=0],见图4。按研究类型亚组分析,4篇非随机对照试验合并显示可膨胀髓内钉组手术时间明显少于交锁髓内钉组[SMD=-1.69,95%CI(-2.30,-1.08),P=0][13-16];3篇随机对照试验合并均显示可膨胀髓内钉组手术时间明显少于交锁髓内钉组[SMD=-3.38,95%CI(-4.69,-2.07),P=0][17-19]。"
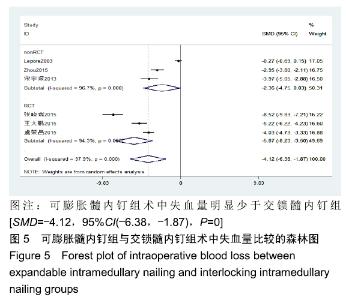
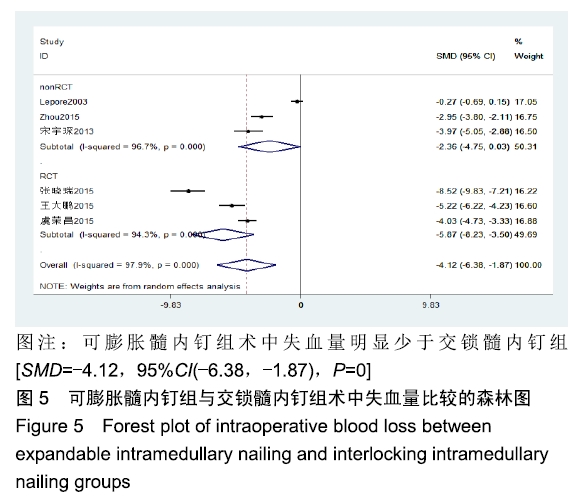
2.2.4 术中失血量 共有6篇文献报道了术中失血量[13,15-19],共计样本量430例,两组各215例。异质性检验提示各研究间存在明显异质性(I2=97.9%,P=0),故采用随机效应模型。结果显示可膨胀髓内钉组术中失血量明显少于交锁髓内钉组[SMD=-4.12,95%CI(-6.38,-1.87),P=0],见图5。按研究类型亚组分析,3篇非随机对照试验合并显示两组术中失血量比较差异无显著性意义[SMD= -2.36,95%CI(-4.75,0.03),P=0.053][13,15-16];3篇随机对照试验合并均显示可膨胀髓内钉组术中失血量明显少于交锁髓内钉组[SMD=-5.87,95%CI(-8.23,-3.50),P=0][17-19]。"
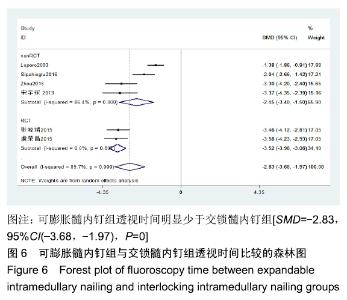
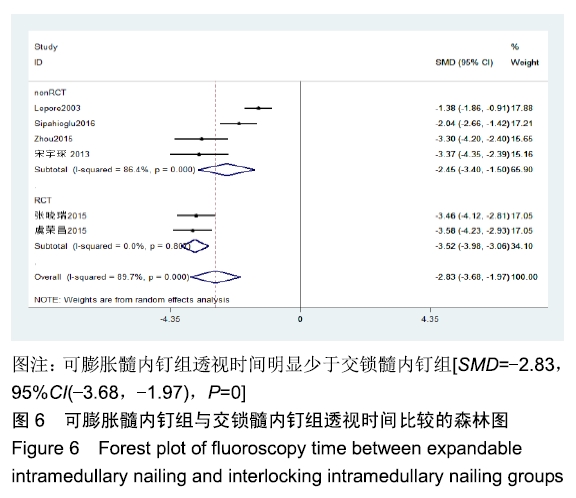
2.2.5 透视时间 共6篇文献报道了术中透视时间[13-16,18-19],共计样本量422例,两组各211例。异质性检验提示各研究间存在明显异质性(I2=89.7%,P=0.000),故采用随机效应模型。结果显示可膨胀髓内钉组透视时间明显少于交锁髓内钉组[SMD=-2.83,95%CI(-3.68,-1.97),P=0],见图6。按研究类型亚组分析,4篇非随机对照试验合并显示可膨胀髓内钉组透视时间明显少于交锁髓内钉组[SMD=-2.45,95%CI(-3.40,-1.50),P=0][13-16];2篇随机对照试验合并均显示可膨胀髓内钉组的透视时间明显少于交锁髓内钉组[SMD=-3.52,95%CI(-3.98,-3.06),P=0][18-19]。"
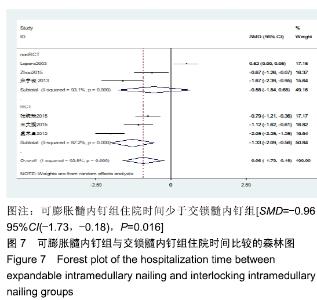
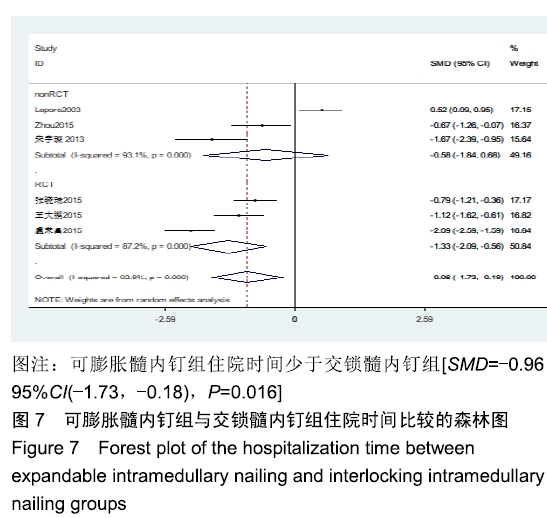
2.2.6 住院时间 共有6篇文献报道了住院时间[13,15-19],共计样本量430例,两组各215例。异质性检验提示,各研究间存在明显异质性(I2=92.8%,P=0),故采用随机效应模型。结果显示可膨胀髓内钉组住院时间少于交锁髓内钉组[SMD=-0.96,95%CI(-1.73,-0.18),P=0.016],见图7。按研究类型亚组分析,3篇非随机对照试验合并显示两组住院时间比较差异无显著性意义[SMD=-0.58,95%CI (-1.84,0.68),P=0.396][13,15-16];3篇随机对照试验合并显示可膨胀髓内钉组住院时间明显少于交锁髓内钉组[SMD=-1.33,95%CI(-2.09,-0.56),P=0.001][17-19]。 "
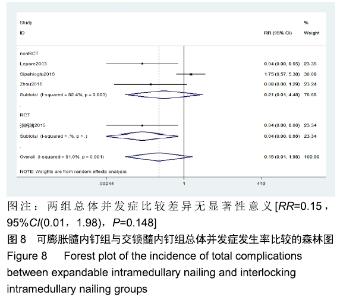
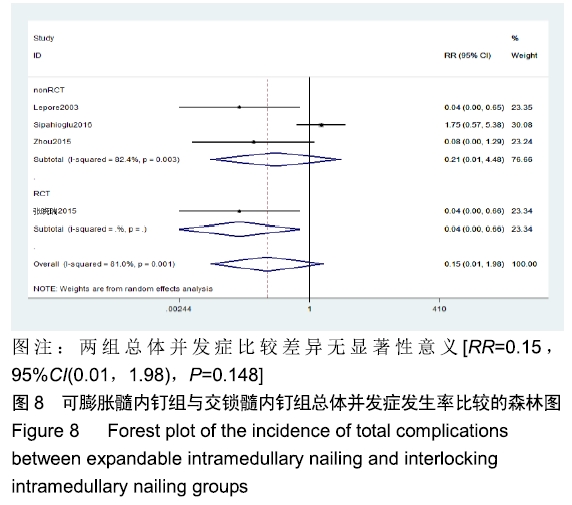
2.2.7 总体并发症 共有4篇文献报道了并发症[13-15,18],包括伤口感染、松动、断钉等不同程度的并发症,共计样本量286例,两组各143例,其中总并发症可膨胀髓内钉组为7例(4.8%),交锁髓内钉组34例(23.8%)。异质性检验提示各研究间存在明显异质性(I2=81%,P=0.001),故采用随机效应模型。结果显示两组总体并发症比较差异无显著性意义[RR=0.15,95%CI(0.01,1.98),P=0.148],见图8。按研究类型亚组分析,3篇非随机对照试验合并显示两组并发症比较差异无显著性意义[RR=0.21,95%CI(0.01,4.48),P=0.320][13-15];只有1篇随机对照试验结果显示可膨胀髓内钉组的总体并发症发生率低于交锁髓内钉组[RR=0.04,95%CI(0.00,0.66),P=0.024][18]。"

2.3 敏感性分析 对骨折愈合时间指标行敏感性分析,逐一剔除文献合并后发现,剔除“虞荣昌,2015年”研究后变为同质,但两组比较差异仍具有统计学意义,提示合并结果相对稳健。考虑该文献可能为异质性来源,详细阅读全文,考虑在记录骨折愈合时间的标准上存在差异(临床愈合时间和影像学愈合时间差异)。对于手术时间、术中失血量及透视时间指标,逐一剔除文献合并后分析发现异质性并未发生明显变化,但两组比较差异仍具有统计学意义,提示合并结果相对稳健。对于骨不连或延迟愈合率、总体并发症发生率指标,均剔除“Sipahioglu,2016年”研究后合并出现同质,且两组差异有统计学意义,可膨胀髓内钉组的骨不连或延迟愈合率及总体并发症发生率均低于交锁髓内钉组。敏感性分析提示合并结果不稳健,还需要更多的随机对照试验来证实。"

| [1] BRÅTEN M, HELLAND P, GRØNTVEDT T, et al. External fixation versus locked intramedullary nailing in tibial shaft fractures: a prospective, randomised study of 78 patients. Arch Orthop Trauma Surg.2005;125(1):21-26. [2] 张绍东,唐天驷,杨惠林,等.带锁髓内钉在股骨干骨折翻修术中的疗效分析[J].中国矫形外科杂志,2010,11(6):427. [3] NIU Y, BAI Y, XU S, et al. Treatment of lower extremity long bone nonunion with expandable intramedullary nailing and autologous bone grafting.Arch Orthop Trauma Surg.2011; 131(7): 885-891. [4] 郭振河,郑晓明,谭春华,等.锁髓内钉在骨折治疗中的相关问题探讨[J].中国矫形外科杂志,2010,11(9):639. [5] BEAZLEY J, MAUFFREY C, SELIGSON D. Treatment of acute tibial shaft fractures with an expandable nailing system: a systematic review of the literature. Injury. 2011; 42 Suppl 4: S11-6. [6] JOVANOVIC A, PIRPIRIS M, SEMIRLI H, et al. Fixion nails for humeral fractures.Injury.2004; 35(11):1140-1142. [7] STEINBERG EL, KEYNAN O, STERNHEIM A, et al. Treatment of diaphyseal nonunion of the femur and tibia using an expandable nailing system.Injury.2009;40(3):309-314. [8] NIU Y, BAI Y, XU S, et al.Treatment of lower extremity long bone nonunion with expandable intramedullary nailing and autologous bone grafting.Arch Orthop Trauma Surg.2011; 131(7):885-891. [9] FRANCK WM, OLIVIERI M, JANNASCH O, et al. Expandable nail system for osteoporotic humeral shaft fractures: preliminary results.J Trauma.2003;54(6):1152-1158. [10] FOLMAN Y, RON N, SHABAT S, et al.The Fixion expandable stem hemi¬arthroplasty for displaced femoral neck frac¬ture: technical features and pilot study.Arch Orthop Trauma Surg. 2010; 130(4):527-531. [11] HIGGINS JPT, GREEN S.Cochrane handbook for systematic reviews of interventions version 5.1.0.2011.Available from www.Cochrane-Handbook.org [12] STANG A.Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta analyses.Eur J Epidemiol.2010;25(9):603-605. [13] LEPORE L, LEPORE S, Maffulli N.Intramedullary nailing of the femur with an inflatable self-locking nail: comparison with locked nailing.J Orthop Sci.2003;8(6):796-801. [14] SIPAHIOGLU S, ZEHIR S, SARIKAYA B, et al.Comparision of the expandable nail with locked nail in the treatment of closed diaphyseal fractures of femur.Niger J Clin Pract. 2017;20(7): 792-798. [15] ZHOU ZT, SONG YC, ZHOU XZ, et al.Femoral midshaft fractures: expandable versus locked nailing.Orthopedics. 2015;38(4):e314-318. [16] 宋宇琛.交锁髓内钉与膨胀髓内钉治疗股骨干骨折的对比研究[J].中国现代医药杂志,2013,15(6):20-22. [17] 王大鹏,彭庆州.交锁髓内钉与膨胀髓内钉治疗股骨干骨折的疗效比较[J].中国实用医药,2015,10(8):89-90. [18] 张晓瑞,高长城,乔永军.可膨胀髓内钉与交锁髓内钉治疗股骨干骨折疗效对比研究[J].河北医学,2015,21(3):419-422. [19] 虞荣昌,李临齐,姜双双.可膨胀髓内钉与交锁髓内钉治疗股骨干骨折的比较分析[J].世界最新医学信息文摘,2015,15(42):55,63. [20] BEKMEZCI T, TONBUL M, KOCABAŞ R, et al.Early treatment results with expandable intramedullary nails in lower extremity shaft fractures.Ulus Travma Acil Cerrahi Derg. 2004;10(2):133-137. [21] PASCARELLA R, NASTA G, NICOLINI M, et al.The Fixion nail in the lower limb. Preliminary results.Chir Organi Mov. 2002; 87(3):169-174. [22] KAPOOR SK, KATARIA H, BORUAH T, et al.Expandable self-locking nail in the management of closed diaphyseal fractures of femur and tibia.Indian J Orthop. 2009;43(3): 264-270. [23] BEKMEZCI T, BACA E, KAYNAK H, et al.Early results of treatment with expandable intramedullary nails in femur shaft fractures.Acta Orthop Traumatol Turc.2006;40(1):1-5. [24] ZOCCALI C, DI FRANCESCO A, RANALLETTA A, et al. Clinical and radiological midterm results from using the Fixion expandable intramedullary nail in transverse and short oblique fractures of femur and tibia.J Orthop Traumatol.2008; 9(3):123-128. [25] BI Q, ZHU DJ, QIU BS, et al.Comparative study on treatment of midshaft tibial fracture with expandable and interlocking intramedullary nails.Chin J Traumatol.2007;10(4):228-232. [26] 黄钿锋,陈昆,郑文忠,等.选择运用可膨胀髓内钉治疗股骨干中、上段骨折60例[J].临床军医杂志,2015,43(8):817-819. [27] SAMIEZADEH S, TAVAKKOLI AVVAL P, FAWAZ Z, et al. Biomechanical assessment of composite versus metallic intramedullary nailing system in femoral shaft fractures: A finite element study.Clin Biomech(Bristol,Avon). 2014; 29(7):803-810. [28] STEINBERG EL, GELLER D, YACOUBIAN SV, et al. Intramedullary fixation of tibial shaft fractures using an expandable nail: early results of 54 acute tibial shaft fractures.J Orthop Trauma.2006; 20:303-309. [29] MOED B, WATSON T, CRAMER K, et al.Unreamed retrograde intramedullary nailing of fractures of the femoral shaft.J Orthop Trauma.1998;12:334-342. [30] SCHEMITSCH EH, KOWALSKI MJ, SWIONTKOWSKI MF, et al.Cortical bone blood flow in reamed and unreamed locked intramedullary nailing: a fractured tibia model in sheep.J Orthop Trauma.1994; 8:373-382. [31] GRUNDNES O, REIKERAS O. Acute effects of intramedullary reaming on bone blood flow in rats. Acta Orthop Scand.1993; 64:203-206. [32] BHANDARI M, GUYATT GH, TONG D, et al.Reamed versus non-reamed intramedullary nailing of lower extremity long bone fractures: a systematic overview and meta-analysis.J Orthop Trauma.2000; 14:2-9. [33] SMITH WR, ZIRAN B, AGUDELO JF, et al.Expandable intramedullary nailing for tibial and femoral fractures: a preliminary analysis of perioperative complications.J Orthop Trauma.2006; 20(5):310-314. [34] OZTURK H, UNSALDI T, OZTEMUR Z, et al.Extreme complications of Fixion nail in treatment of long bone fractures.Arch Orthop Trauma Surg.2008;128(3):301-306. [35] ROSE DM, SMITH TO, NIELSEN D, et al.Expandable intramedullary nails in lower limb trauma: a systematic review of clinical and radiological outcomes.Strat Traum Limb Recon. 2013;8(1):1-12. [36] BLUM J, KARAGÜL G, STERNSTEIN W, et al.Bending and torsional stiffness in cadaver humeri fixed with a self-locking expandable or interlocking nail system: a mechanical study.J Orthop Trauma. 2005;19(8):535-542. [37] OLIVEIRA ML, LEMON MA, MEARS SC, et al. Biomechanical comparison of expandable and locked intramedullary femoral nails.J Orthop Trauma.2008;22(7):446-450. [38] IVANOV D, BARABASH Y, BARABASH A.A numerical comparative analysis of ChM and Fixion nails for diaphyseal femur fractures.Acta Bioeng Biomech.2016;18(3):73-81. [39] ITO K, HUNGERBÜHLER R, WAHL D, et al.Improved intramedullary nail interlocking in osteoporotic bone.J Orthop Trauma. 2001;15(3):192-196. |
| [1] | Hu Kai, Qiao Xiaohong, Zhang Yonghong, Wang Dong, Qin Sihe. Treatment of displaced intra-articular calcaneal fractures with cannulated screws and plates: a meta-analysis of 15 randomized controlled trials [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1465-1470. |
| [2] | Huang Dengcheng, Wang Zhike, Cao Xuewei. Comparison of the short-term efficacy of extracorporeal shock wave therapy for middle-aged and elderly knee osteoarthritis: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1471-1476. |
| [3] | Xu Feng, Kang Hui, Wei Tanjun, Xi Jintao. Biomechanical analysis of different fixation methods of pedicle screws for thoracolumbar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1313-1317. |
| [4] | Zhang Chong, Liu Zhiang, Yao Shuaihui, Gao Junsheng, Jiang Yan, Zhang Lu. Safety and effectiveness of topical application of tranexamic acid to reduce drainage of elderly femoral neck fractures after total hip arthroplasty [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1381-1386. |
| [5] | Chen Xinmin, Li Wenbiao, Xiong Kaikai, Xiong Xiaoyan, Zheng Liqin, Li Musheng, Zheng Yongze, Lin Ziling. Type A3.3 femoral intertrochanteric fracture with augmented proximal femoral nail anti-rotation in the elderly: finite element analysis of the optimal amount of bone cement [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1404-1409. |
| [6] | Du Xiupeng, Yang Zhaohui. Effect of degree of initial deformity of impacted femoral neck fractures under 65 years of age on femoral neck shortening [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1410-1416. |
| [7] | Zhang Chao, Lü Xin. Heterotopic ossification after acetabular fracture fixation: risk factors, prevention and treatment progress [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1434-1439. |
| [8] | Zhou Jihui, Li Xinzhi, Zhou You, Huang Wei, Chen Wenyao. Multiple problems in the selection of implants for patellar fracture [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1440-1445. |
| [9] | Wang Debin, Bi Zhenggang. Related problems in anatomy mechanics, injury characteristics, fixed repair and three-dimensional technology application for olecranon fracture-dislocations [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1446-1451. |
| [10] | Chen Junming, Yue Chen, He Peilin, Zhang Juntao, Sun Moyuan, Liu Youwen. Hip arthroplasty versus proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1452-1457. |
| [11] | Chen Jinping, Li Kui, Chen Qian, Guo Haoran, Zhang Yingbo, Wei Peng. Meta-analysis of the efficacy and safety of tranexamic acid in open spinal surgery [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(9): 1458-1464. |
| [12] | Wang Yongsheng, Wu Yang, Li Yanchun. Effect of acute high-intensity exercise on appetite hormones in adults: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(8): 1305-1312. |
| [13] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [14] | He Li, Tian Wei, Xu Song, Zhao Xiaoyu, Miao Jun, Jia Jian. Factors influencing the efficacy of lumbopelvic internal fixation in the treatment of traumatic spinopelvic dissociation [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 884-889. |
| [15] | Yang Weiqiang, Ding Tong, Yang Weike, Jiang Zhengang. Combined variable stress plate internal fixation affects changes of bone histiocyte function and bone mineral density at the fractured end of goat femur [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(6): 890-894. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||