Chinese Journal of Tissue Engineering Research ›› 2019, Vol. 23 ›› Issue (33): 5404-5412.doi: 10.3969/j.issn.2095-4344.1839
Bone morphogenetic protein 9: osteogenic induction mechanism and clinical application
Zhu Zhengqing, Chen Xiangrun, Jia Fangteng, Huang Lanfeng
- Department of Orthopedics, Second Hospital of Jilin University, Changchun 130041, Jilin Province, China
-
Revised:2019-06-15Online:2019-11-28Published:2019-11-28 -
Contact:Huang Lanfeng, Chief physician, Professor, Master’s supervisor, Department of Orthopedics, Second Hospital of Jilin University, Changchun 130041, Jilin Province, China -
About author:Zhu Zhengqing, Master candidate, Department of Orthopedics, Second Hospital of Jilin University, Changchun 130041, Jilin Province, China -
Supported by:the Health Special Project of Jilin Provincial Finance Department, No. 201817294302 (to HLF)
CLC Number:
Cite this article
Zhu Zhengqing, Chen Xiangrun, Jia Fangteng, Huang Lanfeng. Bone morphogenetic protein 9: osteogenic induction mechanism and clinical application[J]. Chinese Journal of Tissue Engineering Research, 2019, 23(33): 5404-5412.
share this article

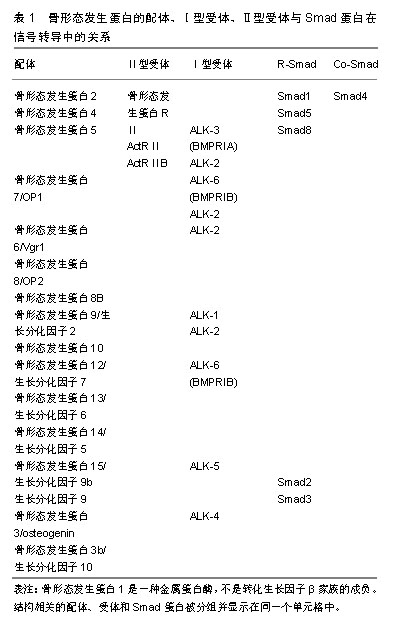
2.1 骨形态发生蛋白9的基本特征 骨形态发生蛋白最初被发现是作为骨提取物中的骨诱导成分,目前已经发现其在各种器官及组织(包括骨、软骨、肌肉、肾脏和血管)的生长和发育过程中发挥重要作用。骨形态发生蛋白是转化生长因子β家族的成员,其通过Ⅰ型和Ⅱ型丝氨酸-苏氨酸激酶受体及其细胞内的下游效应器(包括SMAD蛋白)传递信号。骨形态发生蛋白家族的配体在胚胎发育和保持体内环境稳定的多种过程中起着重要的作用,它通过调节细胞的形态发生、谱系结合、分化、增殖和凋亡,在全身各个类型的细胞中发挥着至关重要的作用[15-16],并已被证明能调节干细胞增殖和成骨分化[17-19]。在过去的几十年中,研究人员研究了骨形态发生蛋白9与成骨细胞分化有关的几种调控途径,如经典WNT信号通路、胰岛素生长因子2(IGF2)/PI3K/AKT信号通路、类维生素A(RAs)信号通路、Notch信号通路、丝裂原活化蛋白激酶(MAPKs)信号通路等[20-24],转录因子、染色质结构修饰剂和骨形态发生蛋白等信号分子在成骨分化过程中起着关键性作用[25-27]。人类中被鉴定的骨形态发生蛋白至少有15种,部分成员是有效的骨诱导因子,如骨形态发生蛋白2、4、6、7和9[28-32]。骨形态发生蛋白的配体、各种受体之间的关系见表1。"
| [1]Hao Z, Song Z, Huang J, et al. The scaffold microenvironment for stem cell based bone tissue engineering. Biomater Sci.2017;5(8): 1382-1392.[2]汤显能,陈跃平,章晓云.骨与软骨组织工程中骨形态发生蛋白的特征与临床应用[J].中国组织工程研究,2019,23(4):591-596.[3]Siddiqui JA, Partridge NC. Physiological Bone Remodeling: Systemic Regulation and Growth Factor Involvement.Physiology (Bethesda). 2016;31(3):233[4]Thoma DS, Lim HC, Sapata VM, et al. Recombinant bone morphogenetic protein-2 and platelet-derived growth factor-BB for localized bone regeneration. Histologic and radiographic outcomes of a rabbit study.Clin Oral Implants Res. 2017;28(11): e236-e243.[5]Lindsey RC, Mohan S. Skeletal Effects of Growth Hormone and Insulin-like Growth Factor-I Therapy. Mol Cell Endocrinol. 2016; 432:44-55.[6]Lamplot JD, Qin J, Nan G, et al. BMP9 signaling in stem cell differentiation and osteogenesis. Am J Stem Cells.2013;2(1):1-21.[7]Reddi AH, Reddi A. Bone morphogenetic proteins (BMPs): from morphogens to metabologens. Cytokine Growth Factor Rev.2009; 20(5-6):341-342.[8]Fujioka-Kobayashi M, Schaller B, Saulacic N,et al. Absorbable collagen sponges loaded with recombinant bone morphogenetic protein 9 induces greater osteoblast differentiation when compared to bone morphogenetic protein 2. Clin Exp Dent Res. 2017; 3(1): 32-40.[9]Fujioka-Kobayashi M, Abd El Raouf M, Saulacic N, et al. Superior bone-inducing potential of rhBMP9 compared to rhBMP2. J Biomed Mater Res A. 2018;106(6):1561-1574.[10]Kang Q, Song WX, Luo Q, et al. A comprehensive analysis of the dual roles of BMPs in regulating adipogenic and osteogenic differentiation of mesenchymal progenitor cells. Stem Cells Dev. 2009;18(4):545-559.[11]Kang Q, Sun MH, Cheng H, et al. Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery. Gene Ther. 2004; 11(17): 1312.[12]Luu HH, Song WX, Luo X, et al. Distinct roles of bone morphogenetic proteins in osteogenic differentiation of mesenchymal stem cells.J Orthop Res. 2007;25(5):665-677.[13]Luther G, Wagner ER, Zhu G,et al. BMP-9 Induced Osteogenic Differentiation of Mesenchymal Stem Cells: Molecular Mechanism and Therapeutic Potential.Curr Gene Ther. 2011;11(3):229-240.[14]Khorsand B, Elangovan S, Hong L,et al.A Comparative Study of the Bone Regenerative Effect of Chemically Modified RNA Encoding BMP-2 or BMP-9. AAPS J.2017;19(2):438.[15]Olsen OE, Sankar M, Elsaadi S, et al. BMPR2 inhibits activin and BMP signaling via wild-type ALK2. J Cell Sci.2018;131(11).[16]Haimov H, Yosupov N, Pinchasov G, et al. Bone Morphogenetic Protein Coating on Titanium Implant Surface: a Systematic Review. J Oral Maxillofac Res.2017;8(2):e1[17]Zhang J, Li L. BMP signaling and stem cell regulation. Dev Biol. 2005;284(1):1-11.[18]Wang RN, Green J, Wang Z, et al. Bone Morphogenetic Protein (BMP) signaling in development and human diseases. Genes Dis. 2014;1(1): 87-105.[19]Zhang F, Song J, Zhang H, et al. Wnt and BMP Signaling Crosstalk in Regulating Dental Stem Cells: Implications in Dental Tissue Engineering. Genes Dis.2016;3(4):263-276.[20]Lindsley HB, Smith DD. Enhanced prostaglandin E2 secretion by cytokine-stimulated human synoviocytes in the presence of subtherapeutic concentrations of nonsteroidal antiinflammatory drugs. Arthritis Rheum.1990; 33(8): 1162-1169.[21]Canalis E. Growth factor control of bone mass. J Cell Biochem. 2009;108(4):769-777.[22]Milat F, Ng KW. Is Wnt signalling the final common pathway leading to bone formation. Mol Cell Endocrinol.2009; 310(1-2): 52-62.[23]Rosen V. BMP2 signaling in bone development and repair. Cytokine Growth Factor Rev.2009; 20(5-6): 475-480.[24]Komori T. Regulation of bone development and extracellular matrix protein genes by RUNX2. Cell Tissue Res.2010;339(1): 189-195.[25]Lian JB, Stein GS, Javed A, et al. Networks and hubs for the transcriptional control of osteoblastogenesis. Rev Endocr Metab Disord.2006;7(1-2):1-16.[26]Jensen ED, Nair AK, Westendorf JJ. Histone deacetylase co-repressor complex control of Runx2 and bone formation. Crit Rev Eukaryot Gene Expr.2007;17(3):187-196.[27]Stein GS, Zaidi SK, Stein JL, et al. Transcription-factor-mediated epigenetic control of cell fate and lineage commitment. Biochem Cell Biol. 2009;87(1):1-6.[28]Haasemann M, Nawratil P, Mülleresterl W. Rat tyrosine kinase inhibitor shows sequence similarity to human alpha 2-HS glycoprotein and bovine fetuin. Biochem J.1991;274 (Pt 3)(3): 899-902.[29]Senta H, Park H, Bergeron E, et al. Cell responses to bone morphogenetic proteins and peptides derived from them: biomedical applications and limitations.Cytokine Growth Factor Rev.2009;20(3): 213-222[30]Singhatanadgit W,Olsen I.Endogenous BMPR-IB signaling is required for early osteoblast differentiation of human bone cells. Vitro Cellular & Developmental Biology Animal.2011; 47(3): 251-259.[31]Bonilla-Claudio M, Wang J, Bai Y,et al. Bmp signaling regulates a dose-dependent transcriptional program to control facial skeletal development. Development.2012;139(4): 709-719.[32]Xiang L, Liang C, Ke ZY,et al. BMP9-Induced Osteogenetic Differentiation and Bone Formation of Muscle-Derived Stem Cells. Biomed Res Int.2012;2012(1):111-113.[33]Song JJ, Celeste AJ, Kong FM,et al. Bone morphogenetic protein-9 binds to liver cells and stimulates proliferation. Endocrinology. 1995;136(10): 4293-4297.[34]Souza A, Bezerra B, Oliveira FS, et al. Effect of bone morphogenetic protein 9 on osteoblast differentiation of cells grown on titanium with nanotopography. J Cell Biochem. 2018; 119(10): 8441-8449.[35]Vhora I, Lalani R, Bhatt P, et al. Lipid-nucleic acid nanoparticles of novel ionizable lipids for systemic BMP-9 gene delivery to bone-marrow mesenchymal stem cells for osteoinduction. Int J Pharm 2019;563:324-336.[36]Huang X, Wang F, Zhao C, et al. Dentinogenesis and Tooth-Alveolar Bone Complex Defects in BMP9/GDF2 Knockout Mice. Stem Cells Dev 2019;28(10):683-694.[37]Nakamura T, Shirakata Y, Shinohara Y, et al. Comparison of the effects of recombinant human bone morphogenetic protein-2 and -9 on bone formation in rat calvarial critical-size defects. Clin Oral Investig.2017; 21(9): 2671-2679.[38]Peng Y, Kang Q, Cheng H, et al. Transcriptional characterization of Bone morphogenetic proteins (BMPs)-mediated osteogenic signaling. J Cell Biochem.2003;90(6):1149–1165.[39]Luo Q, Kang Q, Si W, et al. Connective tissue growth factor (CTGF) is regulated by Wnt and bone morphogenetic proteins signaling in osteoblast differentiation of mesenchymal stem cells. J Biol Chem.2004;279(53):55958-55968.[40]Si W, Kang Q, Luu HH, et al. CCN1/Cyr61 is regulated by the canonical Wnt signal and plays an important role in Wnt3A-induced osteoblast differentiation of mesenchymal stem cells.Mol Cell Biol. 2006;26(8):2955-2964.[41]Liu H, Zhong L, Yuan T, et al. MicroRNA-155 inhibits the osteogenic differentiation of mesenchymal stem cells induced by BMP9 via downregulation of BMP signaling pathway. Int J Mol Med.2018;41(6): 3379-3393.[42]Yan S, Zhang R, Ke W, et al. Characterization of the essential role of Bone Morphogenetic Protein 9 (BMP9) in osteogenic differentiation of mesenchymal stem cells (MSCs) through RNA interference. Genes Dis 2018;5(2):172-184.[43]Zanotti S, Canalis E. Notch Signaling and the Skeleton. Endocr Rev 2016;37(3):223-253.[44]Bolós V, Grego-Bessa J, Jl DLP. Notch signaling in development and cancer. Endocr Rev.2007; 28(3): 339-363.[45]Lardelli M, Dahlstrand J, Lendahl U. The novel Notch homologue mouse Notch 3 lacks specific epidermal growth factor-repeats and is expressed in proliferating neuroepithelium.Mech Dev. 1994; 46(2): 123-136.[46]Uyttendaele H, Marazzi G, Wu G,et al. Notch4/int-3, a mammary proto-oncogene, is an endothelial cell-specific mammalian Notch gene. Development. 1996.122(7):2251-2259.[47]Shutter JR, Scully S, Fan W, et al. Dll4, a novel Notch ligand expressed in arterial endothelium. Genes Dev.2000;14(11): 1313-1318.[48]Yavropoulou MP, Yovos JG. The role of Notch signaling in bone development and disease. Hormones. 2014;13(1): 24-37.[49]Cui J, Zhang W, Huang E, et al. BMP9-induced osteoblastic differentiation requires functional Notch signaling in mesenchymal stem cells. Lab Invest. 2019;99(1):58-71.[50]Cao J, Wei Y, Lian J, et al. Notch signaling pathway promotes osteogenic differentiation of mesenchymal stem cells by enhancing BMP9/Smad signaling.Int J Mol Med. 2017;40(2): 378-388.[51]Fujiokakobayashi M, Schaler P, Shirakata D,et al. Comparison of Two Porcine Collagen Membranes Combined with rhBMP-2 and rhBMP-9 on Osteoblast Behavior In Vitro. Int J Oral Maxillofac Implants. 2017;32(4):221-230.[52]Liao J, Wei Q, Zou Y, et al. Notch Signaling Augments BMP9-Induced Bone Formation by Promoting the Osteogenesis-Angiogenesis Coupling Process in Mesenchymal Stem Cells (MSCs). Cell Physiol Biochem. 2017;41(5):1905-1923.[53]Wang J, Wynshaw-Boris A.The canonical Wnt pathway in early mammalian embryogenesis and stem cell maintenance/ differentiation. Curr Opin Genet Dev.2004;14(5):533-539.[54]Cadigan KM, Nusse R.Wnt signaling: a common theme in animal?development. Genes Dev. 1997;11(24):3286-3305.[55]Nd GD, Karsenty G. In vivo analysis of Wnt signaling in bone. Endocrinology 2007;148(6):2630-2634.[56]Nd GD, Karsenty G. Molecular bases of the regulation of bone remodeling by the canonical Wnt signaling pathway. Curr Top Dev Biol.2006;73(73):43-84.[57]Liu Y, Liu Y, Zhang R, et al. All-trans retinoic acid modulates bone morphogenic protein 9-induced osteogenesis and adipogenesis of preadipocytes through BMP/Smad and Wnt/β-catenin signaling pathways. Int J Biochem Cell Biol.2014; 47: 47-56.[58]Wang H, He XQ, Jin T, et al. Wnt11 plays an important role in the osteogenesis of human mesenchymal stem cells in a PHA/FN/ALG composite scaffold: possible treatment for infected bone defect. Stem Cell Res Ther.2016;7(1):1-13.[59]Zhu JH, Liao YP, Li FS, et al. Wnt11 promotes BMP9-induced osteogenic differentiation through BMPs/Smads and p38 MAPK in mesenchymal stem cells. J Cell Biochem.2018;119(11): 9462-9473.[60]Liao YP, Du WM, Hu Y, et al. CREB/Wnt10b mediates the effect of COX-2 on promoting BMP9-induced osteogenic differentiation via reducing adipogenic differentiation in mesenchymal stem cells. J Cell Biochem. 2019;120(6):9572-9587.[61]Tang N,Song W,Luo J,et al. BMP‐9‐induced osteogenic differentiation of mesenchymal progenitors requires functional canonical Wnt/β‐catenin signalling.J Cell Mol Med. 2009;13(8B): 2448-2464.[62]Deng ZL, Sharff KA, Tang N, et al.Regulation of osteogenic differentiation during skeletal development. Front Biosci.2008; 13(6):2001-2021.[63]Yuan C, Gou X, Deng J,et al. FAK and BMP-9 synergistically trigger osteogenic differentiation and bone formation of adipose derived stem cells through enhancing Wnt-β-catenin signaling. Biomed Pharmacother. 2018l105 753-757.[64]Zhang H, Wang J, Deng F, et al. Canonical Wnt signaling acts synergistically on BMP9-induced osteo/odontoblastic differentiation of stem cells of dental apical papilla (SCAPs). Biomaterials 2015;39:145-154.[65]Li XL, Liu YB, Ma EG, et al. Synergistic effect of BMP9 and TGF-β in the proliferation and differentiation of osteoblasts.Genet Mol Res. 2015;14(3):7605-7615.[66]Wang P, Wang Y, Tang W, et al. Bone Morphogenetic Protein-9 Enhances Osteogenic Differentiation of Human Periodontal Ligament Stem Cells via the JNK Pathway. PLoS One. 2017;12(1): e0169123.[67]Fietz MJ, Concordet JP, Barbosa R, et al. The hedgehog gene family in Drosophila and vertebrate development. Dev Suppl. 1994:43-51.[68]Mundy GR, Yang X. Hedgehog coordination of postnatal osteoclast and osteoblast activities. Dev Cell. 2008;14(5): 637-638.[69]Ingham PW, Mcmahon AP. Hedgehog signaling in animal development: paradigms and principles.Genes Dev. 2001; 15(23): 3059-3087.[70]Ohba S, Kawaguchi H, F, et al. Patched1 Haploinsufficiency Increases Adult Bone Mass and Modulates Gli3 Repressor Activity. Dev Cell.2008;14(5):674-688.[71]Li L, Dong Q, Wang Y, et al.Hedgehog signaling is involved in the BMP9-induced osteogenic differentiation of mesenchymal stem cells. Int J Mol Med.2015;35(6):1641-1650.[72]Choi JY, Pratap J, Javed A, et al. Subnuclear targeting of Runx/Cbfa/AML factors is essential for tissue-specific differentiation during embryonic development. Proc Natl Acad Sci U S A.2001.98(15):8650-8655.[73]Ji C, Liu X, Xu L, et al.RUNX1 Plays an Important Role in Mediating BMP9-Induced Osteogenic Differentiation of Mesenchymal Stem Cells Line C3H10T1/2, Murine Multi-Lineage Cells Lines C2C12 and MEFs. Int J Mol Sci.2017;18(7):1348.[74]Sharff KA, Song WX, Luo X, et al. Hey1 Basic Helix-Loop-Helix Protein Plays an Important Role in Mediating BMP9-induced Osteogenic Differentiation of Mesenchymal Progenitor Cells. J Biol Chem.2009;284(1): 649-659.[75]Wang Y, Feng Q, Ji C,et al. RUNX3 plays an important role in mediating the BMP9-induced osteogenic differentiation of mesenchymal stem cells.Int J Mol Med. 2017;40(6):1991-1999. [76]Wöltje K, Jabs M, Fischer A. Serum Induces Transcription of Hey1 and Hey2 Genes by Alk1 but Not Notch Signaling in Endothelial Cells. PLoS One.2015;10(3): e0120547.[77]Xiao Y, Zeng Z, Xing J. Hey1 functions as a positive regulator of odontogenic differentiation in odontoblast-lineage cells. Int J Mol Med. 2018;41(1): 331-339.[78]Wang JH, Liu YZ, Yin LJ, et al. BMP9 and COX-2 form an important regulatory loop in BMP9-induced osteogenic differentiation of mesenchymal stem cells. Bone.2013; 57(1): 311-321.[79]Su X, Wei Y, Cao J, et al. CCN3 and DLL1 co-regulate osteogenic differentiation of mouse embryonic fibroblasts in a Hey1-dependent manner. Cell Death Dis. 2018;9(12):1188.[80]Wang Y, Yuan M, Guo QY,et al. Mesenchymal Stem Cells for Treating Articular Cartilage Defects and Osteoarthritis.Cell Transplant. 2015; 24(9): 1661-1678.[81]Liu X, Du M, Wang Y,et al. BMP9 overexpressing adipose-derived mesenchymal stem cells promote cartilage repair in osteoarthritis-affected knee joint via the Notch1/Jagged1 signaling pathway. Exp Ther Med.2018;16(6):4623-4631.[82]van Baardewijk LJ, van der Ende J, Lissenberg-Thunnissen S, et al. Circulating bone morphogenetic protein levels and delayed fracture healing. Int Orthop. 2013;37(3):523-527.[83]Wang X, Huang J, Huang F, et al.Bone morphogenetic protein 9 stimulates callus formation in osteoporotic rats during fracture healing. Mol Med Rep. 2017;15(5):2537-2545.[84]Yu L, Dawson LA, Yan M, et al. BMP9 stimulates joint regeneration at digit amputation wounds in mice. Nat Commun. 2019;10(1): 424.[85]Shui W, Zhang W, Yin L, et al. Characterization of scaffold carriers for BMP9-transduced osteoblastic progenitor cells in bone regeneration.J Biomed Mater Res A.2014; 102(10): 3429-3438.[86]Dumont RJ, Dayoub H, Li JZ, et al. Ex vivo bone morphogenetic protein-9 gene therapy using human mesenchymal stem cells induces spinal fusion in rodents. Neurosurgery.2002; 51(5): 1239-1245.[87]Zhang R, Li X, Liu Y, et al. Acceleration of Bone Regeneration in Critical-Size Defect Using BMP-9-Loaded nHA/ColI/MWCNTs Scaffolds Seeded with Bone Marrow Mesenchymal Stem Cells. Biomed Res Int.2019;2019:7343957. |
| [1] | Pu Rui, Chen Ziyang, Yuan Lingyan. Characteristics and effects of exosomes from different cell sources in cardioprotection [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 1-. |
| [2] | Lin Qingfan, Xie Yixin, Chen Wanqing, Ye Zhenzhong, Chen Youfang. Human placenta-derived mesenchymal stem cell conditioned medium can upregulate BeWo cell viability and zonula occludens expression under hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(在线): 4970-4975. |
| [3] | Hou Jingying, Yu Menglei, Guo Tianzhu, Long Huibao, Wu Hao. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival and vascularization through the activation of HIF-1α/MALAT1/VEGFA pathway [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 985-990. |
| [4] | Shi Yangyang, Qin Yingfei, Wu Fuling, He Xiao, Zhang Xuejing. Pretreatment of placental mesenchymal stem cells to prevent bronchiolitis in mice [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 991-995. |
| [5] | Liang Xueqi, Guo Lijiao, Chen Hejie, Wu Jie, Sun Yaqi, Xing Zhikun, Zou Hailiang, Chen Xueling, Wu Xiangwei. Alveolar echinococcosis protoscolices inhibits the differentiation of bone marrow mesenchymal stem cells into fibroblasts [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 996-1001. |
| [6] | Fan Quanbao, Luo Huina, Wang Bingyun, Chen Shengfeng, Cui Lianxu, Jiang Wenkang, Zhao Mingming, Wang Jingjing, Luo Dongzhang, Chen Zhisheng, Bai Yinshan, Liu Canying, Zhang Hui. Biological characteristics of canine adipose-derived mesenchymal stem cells cultured in hypoxia [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1002-1007. |
| [7] | Geng Yao, Yin Zhiliang, Li Xingping, Xiao Dongqin, Hou Weiguang. Role of hsa-miRNA-223-3p in regulating osteogenic differentiation of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1008-1013. |
| [8] | Lun Zhigang, Jin Jing, Wang Tianyan, Li Aimin. Effect of peroxiredoxin 6 on proliferation and differentiation of bone marrow mesenchymal stem cells into neural lineage in vitro [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1014-1018. |
| [9] | Zhu Xuefen, Huang Cheng, Ding Jian, Dai Yongping, Liu Yuanbing, Le Lixiang, Wang Liangliang, Yang Jiandong. Mechanism of bone marrow mesenchymal stem cells differentiation into functional neurons induced by glial cell line derived neurotrophic factor [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1019-1025. |
| [10] | Duan Liyun, Cao Xiaocang. Human placenta mesenchymal stem cells-derived extracellular vesicles regulate collagen deposition in intestinal mucosa of mice with colitis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1026-1031. |
| [11] | Pei Lili, Sun Guicai, Wang Di. Salvianolic acid B inhibits oxidative damage of bone marrow mesenchymal stem cells and promotes differentiation into cardiomyocytes [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1032-1036. |
| [12] | Wang Xianyao, Guan Yalin, Liu Zhongshan. Strategies for improving the therapeutic efficacy of mesenchymal stem cells in the treatment of nonhealing wounds [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1081-1087. |
| [13] | Wang Shiqi, Zhang Jinsheng. Effects of Chinese medicine on proliferation, differentiation and aging of bone marrow mesenchymal stem cells regulating ischemia-hypoxia microenvironment [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1129-1134. |
| [14] | Kong Desheng, He Jingjing, Feng Baofeng, Guo Ruiyun, Asiamah Ernest Amponsah, Lü Fei, Zhang Shuhan, Zhang Xiaolin, Ma Jun, Cui Huixian. Efficacy of mesenchymal stem cells in the spinal cord injury of large animal models: a meta-analysis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(7): 1142-1148. |
| [15] | Liu Bo, Chen Xianghe, Yang Kang, Yu Huilin, Lu Pengcheng. Mechanism of DNA methylation in exercise intervention for osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2021, 25(5): 791-797. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||