Chinese Journal of Tissue Engineering Research ›› 2017, Vol. 21 ›› Issue (35): 5733-5740.doi: 10.3969/j.issn.2095-4344.2017.35.026
Injured vertebra pedicle screw fixation versus short-segment pedicle instrumentation for thoracolumbar fracture: a meta-analysis
Mo Ling1, Lin Shun-xin2, Liang De1, Zhang Shun-cong1, Yang Zhi-dong1, Cui Jian-chao1, Jiang Xiao-bing1, Jin Da-xiang1
- 1Department of Spinal Surgery, the First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China; 2Depatment of Orthopedics, Zhaoqing Gaoyao People’s Hospital, Zhaoqing 526000, Guangdong Province, China
-
Online:2017-12-18Published:2018-01-02 -
Contact:Yang Zhi-dong, Chief physician, Master’s supervisor, Department of Spinal Surgery, the First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China -
About author:Mo Ling, Master, Physician, Department of Spinal Surgery, the First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China
CLC Number:
Cite this article
Mo Ling, Lin Shun-xin, Liang De, Zhang Shun-cong, Yang Zhi-dong, Cui Jian-chao, Jiang Xiao-bing, Jin Da-xiang. Injured vertebra pedicle screw fixation versus short-segment pedicle instrumentation for thoracolumbar fracture: a meta-analysis[J]. Chinese Journal of Tissue Engineering Research, 2017, 21(35): 5733-5740.
share this article

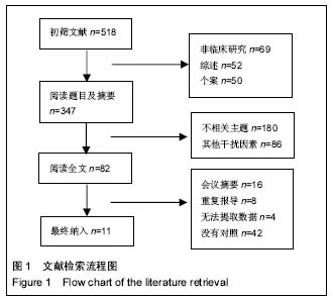
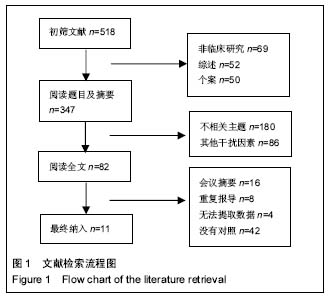
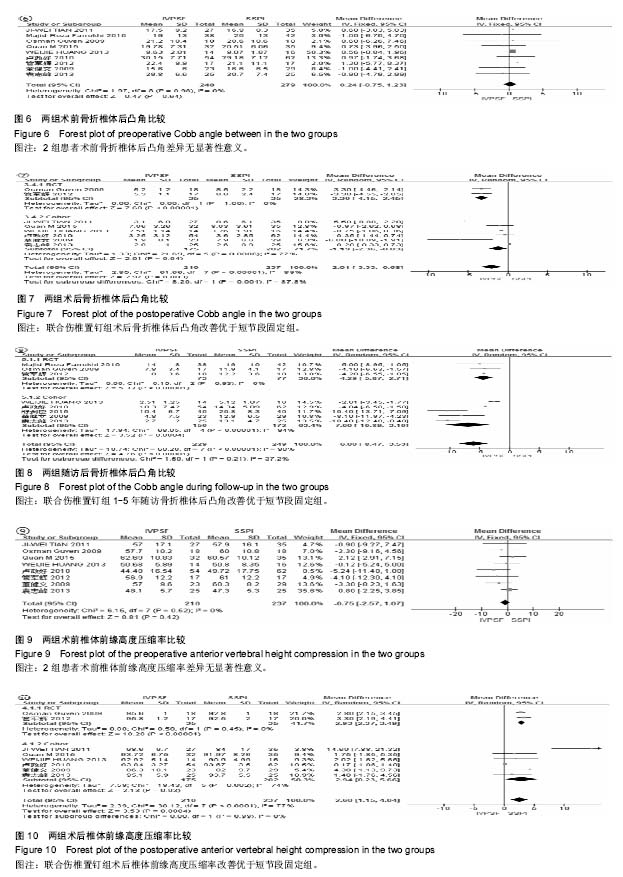
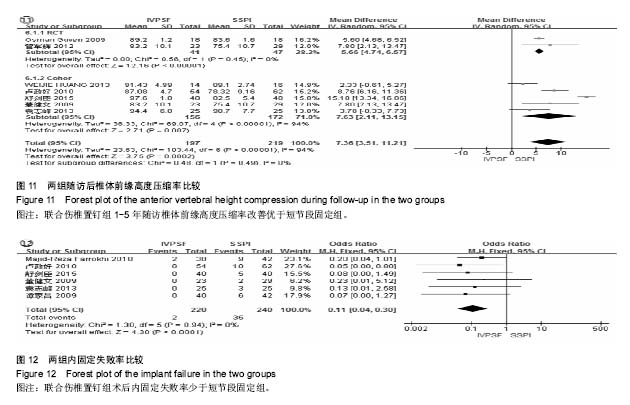
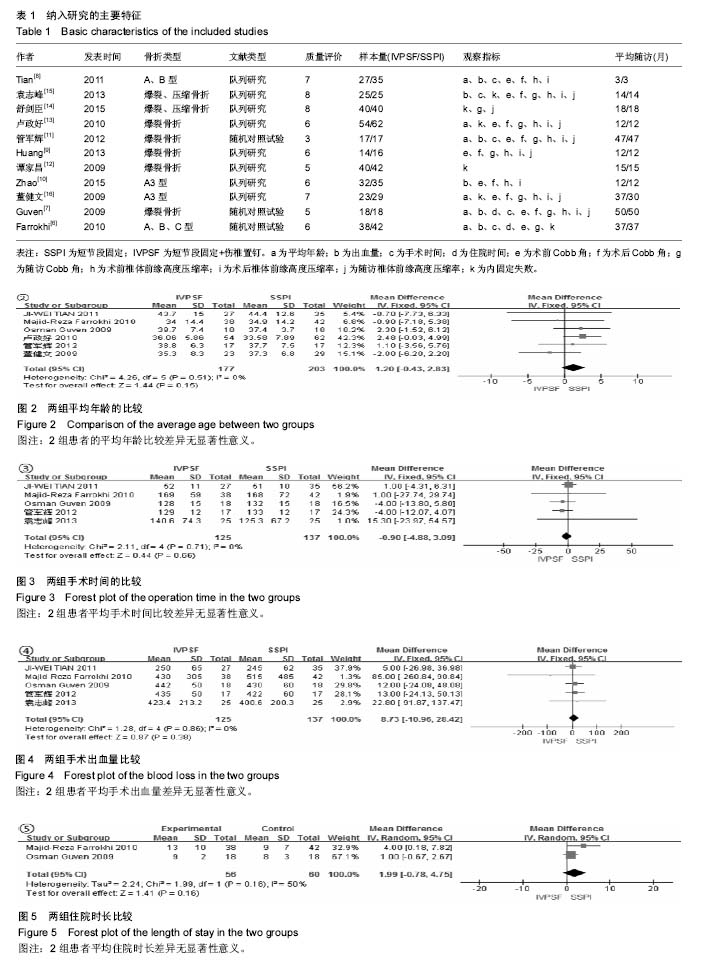
2.2 文献方法学质量评估 纳入的11篇文献中[6-11],应用改良Jadad量表评估3篇随机对照试验文献,3分有1篇,5分有1篇,6分1篇;NOS量表评估8篇队列研究,5分1篇,6分3篇,7分2篇,8分2篇。纳入文献基本特征见表1。 2.3 Meta分析结果 2.3.1 平均年龄 6个研究报告了2组患者平均年 龄[6-8,11,13,16](图2),各研究间无统计学异质性(I2=0%),采用固定效应模型,效应量合并分析指标选用MD。2种手术方式患者的平均年龄差异无显著性意义[MD=1.20,95%CI(-0.43,2.83),P=0.15]。 2.3.2 手术时间 5个研究报告了2种手术方式的平均手术时间[6-8,11,15](图3)。各组间研究无明显统计学异质性(I2=0%),采用固定效应模型,效应量合并分析指标选用MD。2种手术方式的平均手术时间差异无显著性意义[MD=-0.9,95%CI(-4.88,3.09),P=0.66]。 2.3.3 失血量 5个研究报告了2种手术方式的失血 量[6-8,11,15](图4),各研究间无统计学异质性(I2=0%),采用固定效应模型,效应量合并分析指标选用MD。2种手术方式的平均失血量差异无显著性意义[MD=8.73,95%CI (-10.96,28.42),P=0.38]。 2.3.4 住院时间 2个研究报告了患者的平均住院时 间[6-7](图5),研究间存在较大统计学异质性(I2=50%),采用随机效应模型,效应量合并分析指标采用MD。患者平均住院时间差异无显著性意义[MD=1.99,95%CI(-0.78,4.75),P=0.16]。 2.3.5 后凸畸形情况 9个研究报告2组患者术前骨折椎体Cobb角[6-11,13,15-16](图6),I2=0%,无统计学异质性,采用固定效应模型,2组患者术前骨折椎体Cobb角差异无显著性意义[MD=0.24,95%CI(-0.75,1.23),P=0.64]。 8个研究报告了术后Cobb角改善情况[7-11,13,15-16](图7),I2=90%,有高度异质性,根据纳入研究的类型分为随机对照试验组及队列研究组2个亚组进行分析,其中2个研究为随机对照试验组,各研究间无明显统计学异质性(I2=0%);6个研究为队列研究组,各研究间存在明显统计学异质性(I2=77%),因此采用随机效应模型,术后短期Cobb角恢复2组差异均有显著性意义,其中随机对照试验组[MD=-3.30,95%CI(-4.15,-2.45),P < 0.000 1]、队列研究组[MD=-1.19,95%CI(-2.36,-0.03),P=0.04]。 8个研究报告了平均1-5年Cobb角随访情况[6-7,9,11,13-16] (图8),I2=90%,存在明显异质性,根据研究类型进行亚组分析,其中3个研究为随机对照试验组,I2=0%;5个研究为队列研究组,I2=94%,仍存在明显异质性,采用随机效应模型,术后随访Cobb角恢复差异有显著性意义,随机对照试验组[MD=-4.29,95%CI(-5.87,-2.71),P < 0.000 1],队列研究组[MD=-7.00,95%CI(-10.89,-3.10),P=0.000 4]。 2.3.6 骨折椎体前缘恢复情况 8个研究报告了2组患者术前及术后骨折椎体前缘高度压缩率(骨折椎体高度前缘压缩率=骨折椎体前缘高度/骨折椎体相邻上、下椎体前缘高度的均值)[7-11,13,15-16],见图9,10。术前各研究间无明显统计学异质性(I2=0%),采用固定效应模型,2组患者术前骨折椎体前缘高度压缩率差异无显著性意义[MD=-0.75,95%CI (-2.57,1.07),P=0.42];术后各研究间存在明显异质性(I2=77%),依据研究类型进行亚组分析,其中2个研究为随机对照试验组,I2=0%;6个研究为队列研究组,I2=74%, 采用随机效应模型,2组术后骨折椎体前缘高度压缩率差异均有显著性意义,随机对照试验组[MD=2.93,95%CI (2.37,3.49),P < 0.000 01],队列研究组[MD=2.94,95%CI (0.23,5.66),P=0.03]。 7个研究报告了2组患者1-5年随访骨折椎体前缘高度压缩率随访情况[7,9,11,13-16](图11),各研究间存在明显异质性(I2=95%),依据研究类型进行亚组分析,2个研究为随机对照试验组,I2=0%,5个研究为队列研究组,I2=94%,采用随机效应模型,2组差异均有显著性意义,随机对照试验组[MD=5.66,95%CI(4.74,6.57),P < 0.000 01],队列研究组[MD=7.63,95%CI(2.11,13.15),P=0.007]。 2.3.7 内固定失败情况 6个研究出现了内固定失败病 例[6,12-16](图12),各研究间无统计学异质性(I2=0%),采用固定效应模型。2种手术方式的内固定失败差异有显著性意义[MD=0.11,95%CI(0.04,0.03),P < 0.000 1]。 "
| [1] Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture. Asian Spine J. 2015;9(1):133-146.[2] Kim HY, Kim HS, Kim SW, et al. Short segment screw fixation without fusion for unstable thoracolumbar and lumbar burst fracture: a prospective study on selective consecutive patients. J Korean Neurosurg Soc. 2012;51(4):203-207.[3] Mahar A, Kim C, Wedemeyer M, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976). 2007;32(14):1503-1507.[4] 丁文彬,郑召民,王建儒,等. 微创与开放经椎间孔椎体间融合术治疗单节段腰椎病变的Meta分析[J]. 中国脊柱脊髓杂志, 2015, 25(1):45-53.[5] 于亮, 徐荣明, 马维虎, 等. TLIF与PLIF治疗腰椎退行性疾病疗效的Meta分析[J]. 中国脊柱脊髓杂志, 2013,23(10):886-890.[6] Farrokhi MR, Razmkon A, Maghami Z, et al. Inclusion of the fracture level in short segment fixation of thoracolumbar fractures. Eur Spine J. 2010;19(10):1651-1656.[7] Guven O, Kocaoglu B, Bezer M, et al. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2009;22(6):417-421.[8] Tian JW, Wang L, Xia T, et al. Posterior short-segmental fixation combined with intermediate screws vs conventional intersegmental fixation for monosegmental thoracolumbar fractures. Orthopedics. 2011;34(8):389-396.[9] Huang W, Luo T. Efficacy analysis of pedicle screw internal fixation of fractured vertebrae in the treatment of thoracolumbar fractures. Exp Ther Med. 2013;5(3):678-682.[10] Zhao QM, Gu XF, Yang HL, et al. Surgical outcome of posterior fixation, including fractured vertebra, for thoracolumbar fractures. Neurosciences (Riyadh). 2015;20(4): 362-367.[11] 管军辉,冉波,郑文标,等. 伤椎置钉治疗胸腰椎爆裂骨折的临床研究[J]. 中国现代医生, 2012,50(26):53-55.[12] 谭家昌,徐鸿育,杨有猛,等. 伤椎置钉与跨节段椎弓根螺钉内固定术治疗胸腰椎骨折的比较研究[J]. 中国矫形外科杂志, 2009, 17(14):1094-1096.[13] 卢政好,李平元,苏小桃,等. 伤椎置钉技术治疗胸腰椎爆裂性骨折的临床疗效[J]. 第二军医大学学报, 2010,31(12):1368-1371.[14] 舒剑臣,邱志杰,史可测,等. 经伤椎置钉短节段椎弓根钉固定治疗胸腰椎骨折的临床研究[J]. 中国骨与关节损伤杂志, 2015, 30(7):743-745.[15] 袁志峰,邵斌,曾景平. 经伤椎置钉治疗胸腰椎骨折的临床运用及疗效分析[J]. 脊柱外科杂志, 2013,11(1):32-35.[16] 董健文,戎利民,刘斌,等. 经伤椎与跨节段固定治疗无脊髓损伤的胸腰段a3型骨折[J]. 中华外科杂志, 2009,47(24):1883-1887.[17] Kifune M, Panjabi MM, Liu W, et al. Functional morphology of the spinal canal after endplate, wedge, and burst fractures. J Spinal Disord. 1997;10(6):457-466.[18] Hsu JM, Joseph T, Ellis AM. Thoracolumbar fracture in blunt trauma patients: guidelines for diagnosis and imaging. Injury. 2003;34(6):426-433.[19] McLain RF. Functional outcomes after surgery for spinal fractures: return to work and activity. Spine (Phila Pa 1976). 2004;29(4):470-477.[20] Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8(8):817-831.[21] Tezeren IK. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005;18(6):485-488.[22] JW Parker JRL, EE Karaikovic RWG. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 4½-year series. Spine (Phila Pa 1976). 2000;25(9):1157-1170.[23] Altay M, Ozkurt B, Aktekin CN, et al. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007;16(8):1145-1155.[24] McLain RF, Burkus JK, Benson DR. Segmental instrumentation for thoracic and thoracolumbar fractures: prospective analysis of construct survival and five-year follow-up. Spine J. 2001;1(5):310-323.[25] Dubousset J. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1995;77(4):648-649.[26] Hirano T, Hasegawa K, Takahashi HE, et al. Structural characteristics of the pedicle and its role in screw stability. Spine (Phila Pa 1976). 1997;22(21):2504-2509.[27] Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 2001;26(9): 1038-1045.[28] Esses SI, Botsford DJ, Kostuik JP. Evaluation of surgical treatment for burst fractures. Spine (Phila Pa 1976). 1990; 15(7):667-673.[29] Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976). 1992;17(8): 317-324.[30] Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003; 53(6):1354-1360.[31] McNamara MJ, Stephens GC, Spengler DM. Transpedicular short-segment fusions for treatment of lumbar burst fractures. J Spinal Disord. 1992;5(2):183-187.[32] Gelb D, Ludwig S, Karp JE, et al. Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech. 2010;23(5):293-301.[33] 曾忠友,黄伟,张建乔,等. 椎弓根螺钉系统同时经伤椎置钉固定治疗胸腰椎骨折[J]. 中国脊柱脊髓杂志, 2009,19(8):609-613.[34] Kopperdahl DL, Morgan EF, Keaveny TM. Quantitative computed tomography estimates of the mechanical properties of human vertebral trabecular bone. J Orthop Res. 2002;20(4): 801-805.[35] He D, Wu L, Chi Y, et al. Facet joint plus interspinous process graft fusion to prevent postoperative late correction loss in thoracolumbar fractures with disc damage: finite element analysis and small clinical trials. Clin Biomech (Bristol, Avon). 2011;26(3):229-237.[36] D Lin LG, Z Ding WZ, J Hong KL. Modified surgery for acute thoracolumbar fractures: a prospective report. Eur Orthop Traumatol. 2011;2(1):33-39.[37] Andress HJ, Braun H, Helmberger T, et al. Long-term results after posterior fixation of thoraco-lumbar burst fractures. Injury. 2002;33(4):357-365.[38] Qiu TX, Tan KW, Lee VS, et al. Investigation of thoracolumbar T12-L1 burst fracture mechanism using finite element method. Med Eng Phys. 2006;28(7):656-664.[39] Liu L, Pei F, Song Y, et al. The influence of the intervertebral disc on stress distribution of the thoracolumbar vertebrae under destructive load. Chin J Traumatol.2002;5(5):279-283.[40] Norton RP, Milne EL, Kaimrajh DN, et al. Biomechanical analysis of four- versus six-screw constructs for short-segment pedicle screw and rod instrumentation of unstable thoracolumbar fractures. Spine J. 2014;14(8): 1734-1739.[41] Dick JC, Jones MP, Zdeblick TA, et al. A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord. 1994;7(5):402-407. |
| [1] | Xue Yadong, Zhou Xinshe, Pei Lijia, Meng Fanyu, Li Jian, Wang Jinzi . Reconstruction of Paprosky III type acetabular defect by autogenous iliac bone block combined with titanium plate: providing a strong initial fixation for the prosthesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1424-1428. |
| [2] | Zhuang Zhikun, Wu Rongkai, Lin Hanghui, Gong Zhibing, Zhang Qianjin, Wei Qiushi, Zhang Qingwen, Wu Zhaoke. Application of stable and enhanced lined hip joint system in total hip arthroplasty in elderly patients with femoral neck fractures complicated with hemiplegia [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1429-1433. |
| [3] | Yao Xiaoling, Peng Jiancheng, Xu Yuerong, Yang Zhidong, Zhang Shuncong. Variable-angle zero-notch anterior interbody fusion system in the treatment of cervical spondylotic myelopathy: 30-month follow-up [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1377-1382. |
| [4] | Jiang Huanchang, Zhang Zhaofei, Liang De, Jiang Xiaobing, Yang Xiaodong, Liu Zhixiang. Comparison of advantages between unilateral multidirectional curved and straight vertebroplasty in the treatment of thoracolumbar osteoporotic vertebral compression fracture [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(9): 1407-1411. |
| [5] | Li Wei, Zhu Hanmin, Wang Xin, Gao Xue, Cui Jing, Liu Yuxin, Huang Shuming. Effect of Zuogui Wan on bone morphogenetic protein 2 signaling pathway in ovariectomized osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1173-1179. |
| [6] | Wang Jing, Xiong Shan, Cao Jin, Feng Linwei, Wang Xin. Role and mechanism of interleukin-3 in bone metabolism [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1260-1265. |
| [7] | Xiao Hao, Liu Jing, Zhou Jun. Research progress of pulsed electromagnetic field in the treatment of postmenopausal osteoporosis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1266-1271. |
| [8] | Wu Bingshuang, Wang Zhi, Tang Yi, Tang Xiaoyu, Li Qi. Anterior cruciate ligament reconstruction: from enthesis to tendon-to-bone healing [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(8): 1293-1298. |
| [9] | An Weizheng, He Xiao, Ren Shuai, Liu Jianyu. Potential of muscle-derived stem cells in peripheral nerve regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1130-1136. |
| [10] | Tian Chuan, Zhu Xiangqing, Yang Zailing, Yan Donghai, Li Ye, Wang Yanying, Yang Yukun, He Jie, Lü Guanke, Cai Xuemin, Shu Liping, He Zhixu, Pan Xinghua. Bone marrow mesenchymal stem cells regulate ovarian aging in macaques [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 985-991. |
| [11] | Hu Wei, Xie Xingqi, Tu Guanjun. Exosomes derived from bone marrow mesenchymal stem cells improve the integrity of the blood-spinal cord barrier after spinal cord injury [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 992-998. |
| [12] | Gao Yujin, Peng Shuanglin, Ma Zhichao, Lu Shi, Cao Huayue, Wang Lang, Xiao Jingang. Osteogenic ability of adipose stem cells in diabetic osteoporosis mice [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 999-1004. |
| [13] | Fang Xiaolei, Leng Jun, Zhang Chen, Liu Huimin, Guo Wen. Systematic evaluation of different therapeutic effects of mesenchymal stem cell transplantation in the treatment of ischemic stroke [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1085-1092. |
| [14] | Wu Weiyue, Guo Xiaodong, Bao Chongyun. Application of engineered exosomes in bone repair and regeneration [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1102-1106. |
| [15] | Zhou Hongqin, Wu Dandan, Yang Kun, Liu Qi. Exosomes that deliver specific miRNAs can regulate osteogenesis and promote angiogenesis [J]. Chinese Journal of Tissue Engineering Research, 2022, 26(7): 1107-1112. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||